Anorectal abscess
An anorectal abscess is a pus-filled cavity that most commonly develops from an infected anal crypt gland (cryptoglandular infection) following obstruction and bacterial overgrowth**.** The infection begins in the intersphincteris space and may spread upward, downward, and laterally to involve other spaces around the anus and lower rectum. About 50% of anorectal abscesses heal within several weeks after drainage and do not recur. The remainder can form a fistula in ano. If anorectal abscesses remain undrained, necrotizing soft-tissue infection can occur. These carry a 50% mortality.
More common in men than women. Mean age of onset is 40 years (20 – 60 years range). 50% of abscesses develop into fistulas.
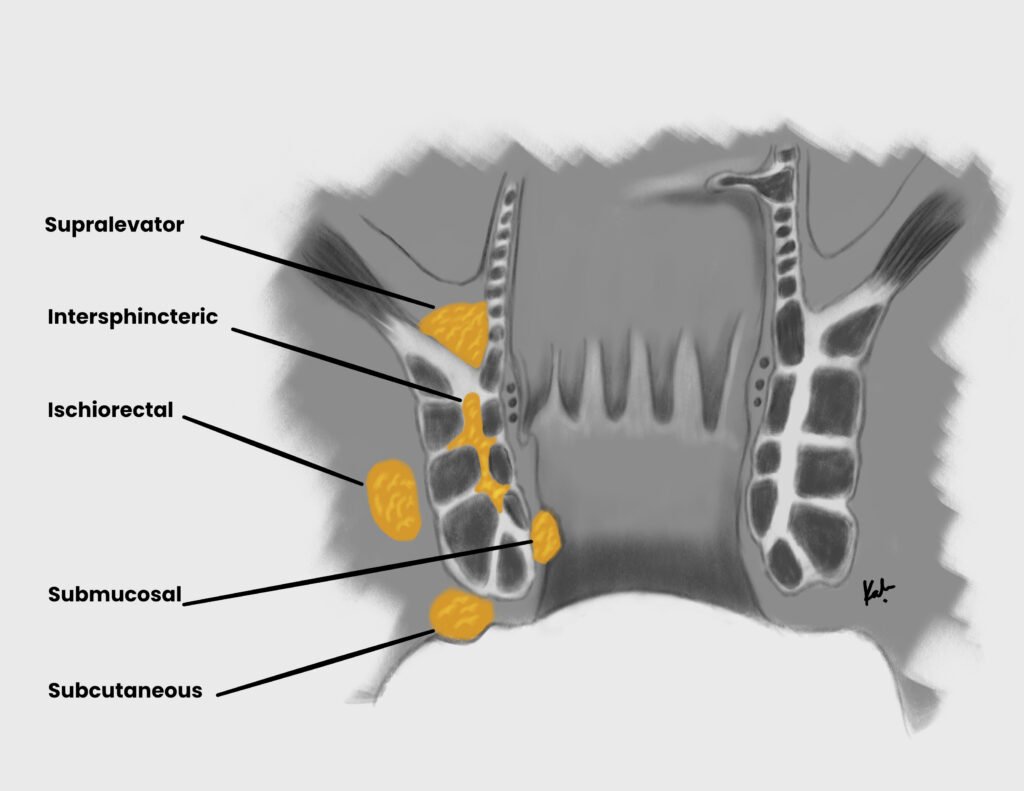
Anatomical locations of anorectal abscess
| Anorectal abscess | Location |
|---|---|
| Ischiorectal abscess (most common) | Abscess beneath the levator ani, traverses the external sphincter into the ischiorectal space. Spreads laterally from the crypts, through the external sphincter and into fatty tissue of ischiorectal space |
| Perianal abscess | Abscess beneath the perianal skin, does not traverse the external sphincter. Extends distally from the crypts to skin surrounding anal verge |
| Intersphincteric abscess | Abscess between the internal and external sphincter. Confined to crypts and glands. |
| Supralevator abscess (least common) | Abscess above the levator ani, extension of intersphincteric abscess OR suppurative abdominal condition (appendicitis, complicated diverticulitis). Extends proximally from crypts past the levator ani muscles into the supralevator space. |
- Risk factors for anorectal abscess
- Flow obstruction and infection of anal crypt glands (MCC, 90%)
- Inflammatory bowel disease (chron’s, ulcerative colitis)
- Acute appendicitis, Complicated diverticulitis
- Radiation-induced proctitis (secondary to radiotherapy for ca prostate)
- Iatrogenic (post-hemorrhoidectomy via iatrogenic sinuses or fistulas)
- Foreign bodies (ingested toothpick or bones; stuff in anus >.<)
- Colorectal cancer
- Immunosuppression (may present with leukopenia or perianal pain without noticeable swelling or signs of infection)
- Pathophysiology
- Obstruction of anal glands by debris → stasis and bacterial overgrowth → Abscess
- Extension of abscess into perirectal spaces (intersphincteric, transphincteric, suprasphincteric, extrasphincteric) → fistula formation, bacteremia, sepsis
- Signs and symptoms
- Constant anorectal pain not associated or worsened with defecation
- Swelling at or around the rectum/anus
- Fever and chills
- Apparent cellulitis or abscess on buttock
- Area of focal tenderness on DRE
- Erythematous, subcutaneous mass near the anus = perianal abscess
- Rectal or perirectal drainage (bloody, purulent, mucoid) = perirectal abscess
- Purulent drainage from the anal canal or anoderm = Fistula
- DRE findings for anorectal abscess
- Fluctuant, indurated mass
- Pain with pressure
- Investigations
- CT or MRI scan: confirm location of deep abscess
- Anal ultrasound: confirm deep abscess
- Proctosigmoidoscopy or anoscopy: rule out other comorbidities (IBD, Malignancy)
- Fistula probe with methylene blue: identify possible fistulae and comorbidities (IBD, Malignancy)
- Treatment
- Incision and drainage: stops further infection and tissue damage (can lead to sphincter damage, promote fistula formation, and lead to sepsis)
- Sitz bath
- Analgesics and stool softeners
- Post-op antibiotics: ciprofloxaxin and metronidazole to cover gram-negatives and anerobes.
- Indications for post-operative antibiotics
- Immunocompromised patients
- Diabetic patients
- Patients with valvular heart disease



