Overview
Vulvar carcinoma (squamous cell) can occur anywhere from the mons pubis to the perianal region. It is rare (3-5% of gynaecologic cancers). The incidence of Vulvar Carcinoma in Situ (VCIS) has increased by 411% between 1973 to 2000 due to increased HPV infection rates. The mean age of diagnosing vulvar cancer is 65 years. Vulvar Intraepithelial neoplasia is diagnosed at a younger age (39 – 50 years).
- Classic Presentation of vulvar malignancy 4 P’s
- Papule formation: Raised lesion +/- erosion and bleeding
- Pruritic
- Patriotic: Red, white, and blue in colour (similar to melanoma)
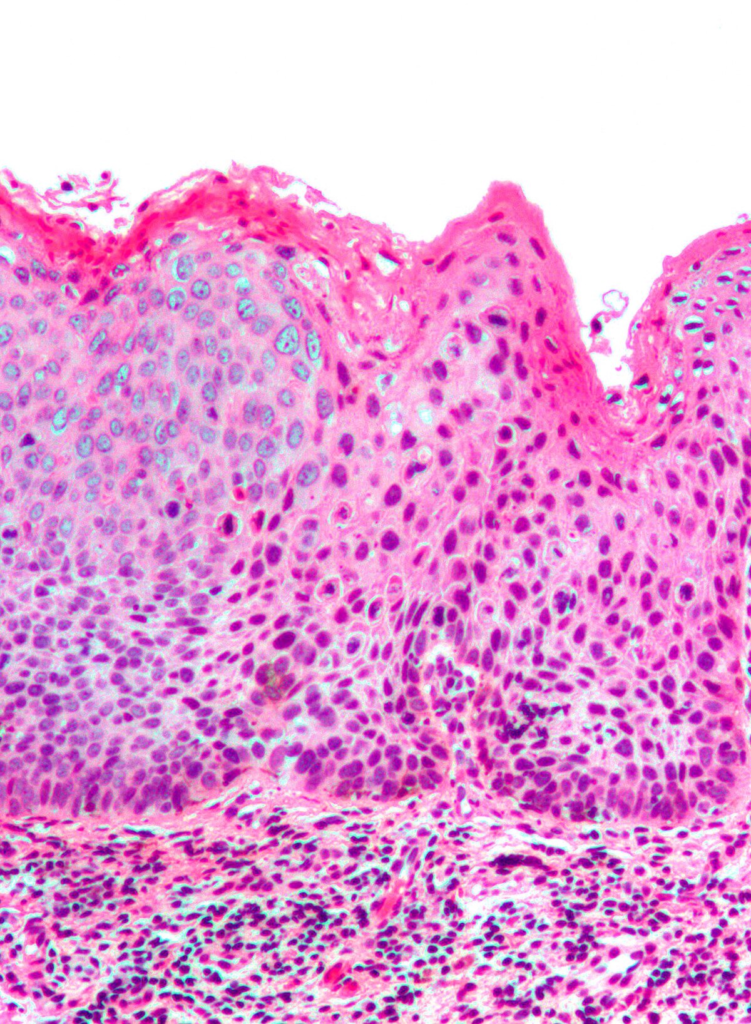
- Parakeratosis: retention of nuclei in the stratum corneum
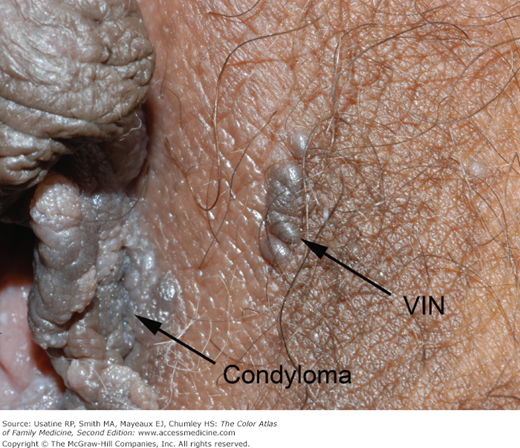
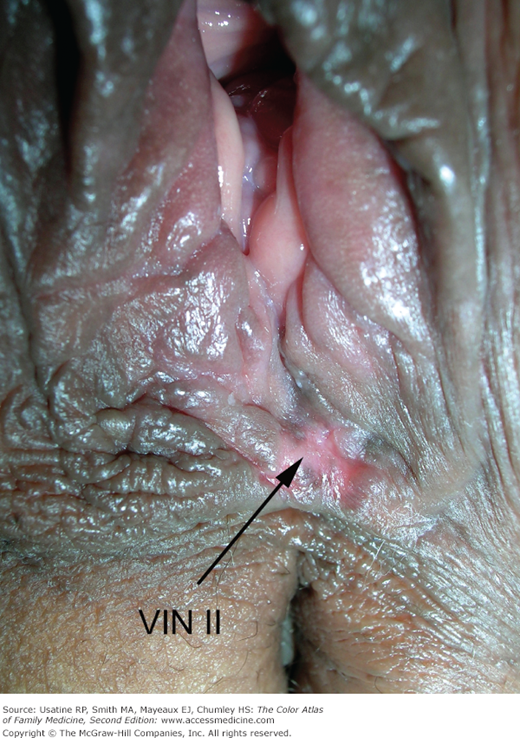
Vulvar Intraepithelial Neoplasia (VIN)
Vin is a premalignant change in the vulvar epithelium characterized by cellular atypia.
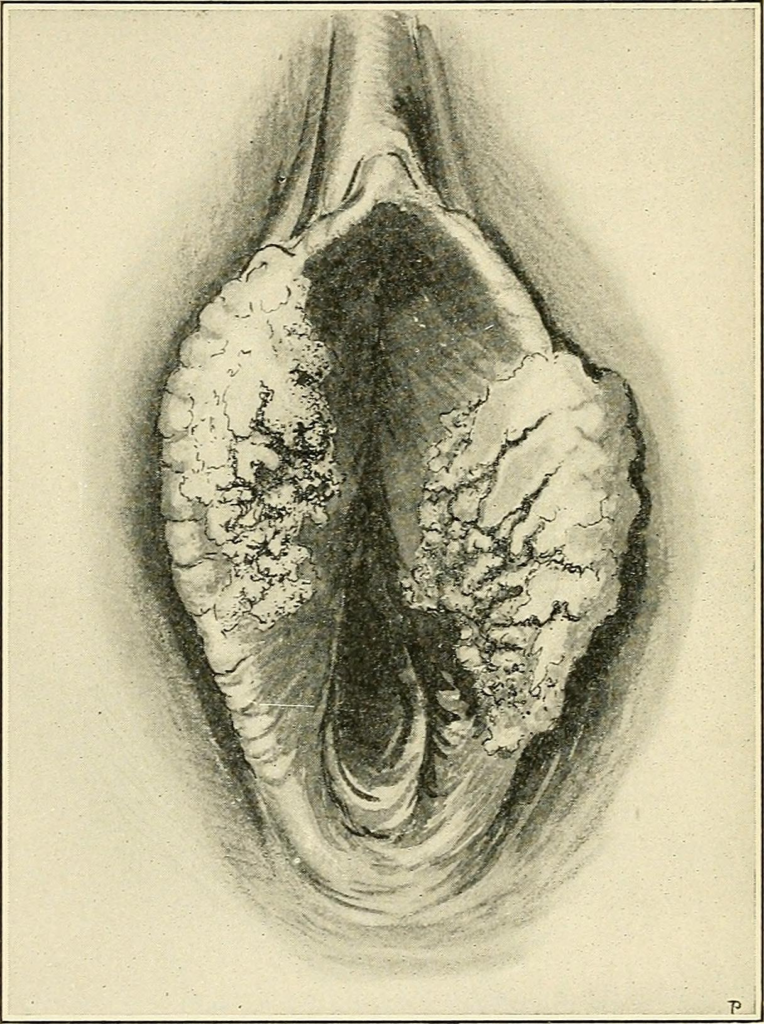
90% of vulvar cancers are squamous cell carcinomas. Typically presents as a pruritic, keratinized or pigmented, bleeding mass in a post-menopausal woman. Diagnosis is by punch biopsy obtained via vulvoscopy – the most abnormal-looking area is biopsied. Dyes are not necessary as in cervical malignancies.
- Indications for biopsy
- Pigmented lesion
- Genital warts in an immunocompromised or post-menopausal woman
- Genital warts that persist despite topical therapy (Podophyllin)
- Evolving lesion (always suspicious for malignancy)
- Treatment of VIN
- If invasive cancer is suspected: Wide local excision
- If invasive cancer is not suspected: Laser ablation
1986 ISSVD Classification
| Classification | Description |
|---|---|
| VIN-1 | Atypia in the deep 1/3 of the epithelium |
| VIN-2 | Atypia in the deep 1/2 of the epithelium |
| VIN-3 | Atypia in the deep 2/3 of the epithelium |
| VCIS | Full-thickness atypia confined to the basement membrane |
2002 ISSVD Classification
VIN-1: eliminated because it was confirmed not to progress to vulvar carcinoma
VIN, usual type: strongly associated with HPV and smoking
VIN, differentiated type: less common, occurs in older women and is associated with lichen sclerosis and squamous cell hyperplasia. More likely to progress to SCC
| Classification | Description |
|---|---|
| VIN-1 | (Eliminated) |
| VIN/VCIS | VIN, usual type (warty, basaloid, mixed) |
| VIN, differentiated type | |
| VIN, unclassified type (Paget’s) |
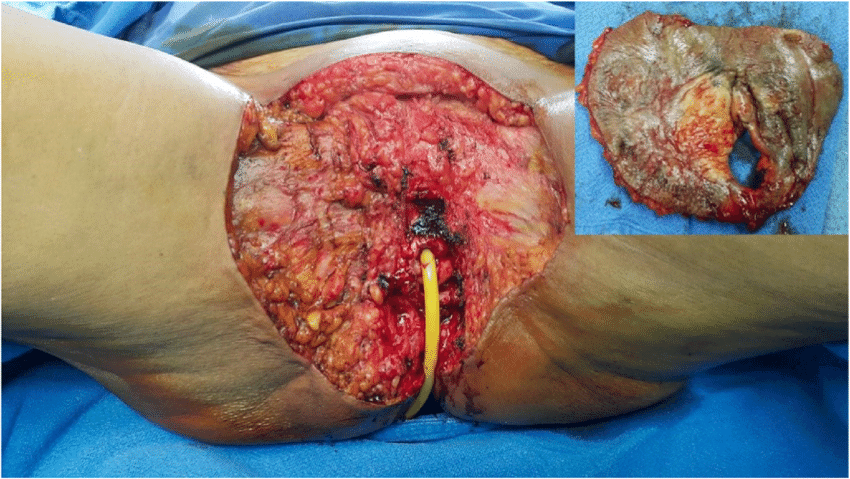
Vulvar Cancer
Vulvar cancer is VIN + destruction of the basement membrane and invasion.
90% of vulvar cancers are SCC. Others include melanoma and Bartholin’s gland adenocarcinoma. The smaller the tumor the more likely the patient will be alive in five years.
- Risk factors
- VIN (especially the differentiated type)
- High-risk HPV infection
- HSV infection
- Lichen sclerosis
- Smoking
- Chronic immunosuppression (especially HIV/AIDS)
- Treatment
- Stage IA: Wide local excision (1-2cm margins)
- Stage IB and II: Partial radical vulvectomy including ipsilateral inguinofemoral lymphadenectomy (bilateral lymphadenectomy should be performed if the tumor crosses midline)
- Stage III: Radical vulvectomy including inguinofemoral lymphadenectomy. Followed by pelvic-groin irradiation +/- chemotherapy (Platinum based – Cisplatin/5-FU)
- Stage IV: Radical vulvectomy including inguinofemoral lymphadenectomy. Occasional pelvic exenteration is done. Followed by chemoradiation
Staging of Vulvar cancer (TNM and Surgical)
1A can get wide local excision. 1B needs vulvectomy. Nodes to examine include the inguinofemoral nodes. Adjacent perineal structures include the lower 1/3 of the urethra, lower 1/3 of the vagina and anus.
| Stage | Description | Treatment |
|---|---|---|
| Stage I | Tumor confined to the vulva. Negative nodes | |
| Stage IA | ≤ 2cm in size and ≤ 1 mm of stromal invasion | Wide local excision |
| Stage IB | > 2cm in size or > 1 mm of stromal invasion | Partial radical vulvectomy including ipsilateral inguinofemoral lymphadenectomy |
| Stage II | Extension to adjacent perineal structures. Negative nodes | Partial radical vulvectomy including ipsilateral inguinofemoral lymphadenectomy |
| Stage III | Extension to adjacent perineal structures. Positive nodes | Radical vulvectomy including inguinofemoral lymphadenectomy. Followed by pelvic-groin irradiation +/- chemotherapy |
| Stage IV | Invasion of other regional or distant structures | Radical vulvectomy including inguinofemoral lymphadenectomy. Occasional pelvic exenteration is done. Followed by chemoradiation |