Overview
Sympathetic outflow works to favor relaxation of the bladder (reduces intravesicular pressure) and constriction of the neck and urethra (increases intraurethral pressure) favoring urinary retention. Parasympathetic outflow stimulates contraction (raises intravesicular pressure) favoring voiding. Normal bladder post-void residual is about 50mL. The bladder typically holds about 1L max. The urge to urinate usually begins at around 400 mL of bladder volume.

| Location | Receptors |
|---|---|
| Detrusor muscles | M2 (80%), M3 (20%), B-adrenergic |
| Bladder dome (mucosa and submucosa) | M2, M3 |
| Bladder neck and urethra | a-adrenergic receptors |
| External urethral sphincter and Pelvic floor muscles | Nicotinic receptors (voluntary) |
Muscarinic (M) receptor → Contracts detrusor muscles
a-adrenergic (a) receptor → constriction of bladder neck and urethra
B adrenergic (B) receptor → relax bladder dome (allows the bladder to become more compliant, reducing pressure)
Nicotinic (N) receptors → constrict external urethral sphincter
Innervation of the bladder

Pharmacologics
| Anticholinergics | TCA | Cholinergics | |
|---|---|---|---|
| Mechanism | Relax detrusor muscle | Relax the dome, Constrict the urethra | Strengthen detrusor muscle |
| Drugs | Propantheline, Oxybutinin, Tolterodine, Fexofenadine | Imipramine | Bethanechol, Neostigmine |
| Use | OAB/UUI, Detrusor hyperactivity | SUI, UUI, Mixed urinary incontinence | OUI, Detrusor hypoactivity |
Overview
| Stress UI | Urge UI | Overflow UI | Bypass UI | |
|---|---|---|---|---|
| Inc. frequency | No | Yes | No | No |
| Urgency | No | Yes | No | No |
| Voluntary voiding? | Yes | Yes | No | Yes |
| Loss w/valsava | Yes | No | No | No |
| Amount lost | Small (intermittent) | Large | Small (persistent) | Small (persistent) |
| Nocturnal Sx | No | Yes (wake up) | Yes (leak) | Yes (leak) |
| S2-S4 reflex | Present | Present | Absent | Present |
| Urinalysis | Normal | Variable | Normal | Normal |
| Q-tip test | > 30 degrees motility | < 30 degrees | < 30 degrees | < 30 degrees |
| Urodynamics | Low IUP | Invol. detrusor contraction | High residual volume | N/A |
| Treatment | Kegels, Surgery | Anticholinergics, Underlying cause | Cholinergic, catheterization | Surgery |
Stress Urinary Incontinence
Stress urinary incontinence is the involuntary leakage of urine following raised intra-abdominal pressure due to weak pelvic floor muscles. No problems with the nervous system, no problems with the detrusor muscles. Little things can cause incontinence, and can adversely impact quality of life. All patients should get urinalysis regardless of the suspected diagnosis. The first step in management is usually conservative.
- Causes
- Weakening of the pelvic floor anatomy due to hypoestrogenism (e.g. menopause)
- Direct injury to the pelvic floor (e.g., traumatic childbirth, surgery)
- Pregnancy (increased IAP → increased IVP)
- Pelvic masses
- Obesity
- Smoking
- Medications
- a-adrenergic antagonists (phenoxybenzamine, trazodone)
- Some antipsychotics and antidepressants
- ACEi (if it causes significant cough)
- Risk factors
- Age (more common in older women)
- Race (more common in white)
- Obesity
- Smoking
- Hypoestrogenism
- Family history
- Patient history
- Postmenopausal
- Multiparous
- Past gynaecological surgeries
- Young woman active in sports
- Signs and symptoms
- Incontinence of urine during valsava (coughing, sneezing, laughing, lifting, orgasm, standing up from siting)
- Intermittent but persistent (may occur so frequently that it is described as ‘continuous’)
- Frequent changing pads
- No symptoms at night
- No urgency
- No increased frequency
- Physical exam
- Mostly unremarkable (normal external genitalia, signs of atrophy may be present)
- No vagina diverticulae
- Bulbocavernous and anocutaneous reflexes are normal (intact S2-S4/pudendal circuit)
- Cough stress test: The patient is asked to cough to demonstrate the involuntary leakage of urine.
- Cotton swab test: ****The female patient is asked to Valsalva after insertion of a lubricated cotton swab placed just into the bladder through the urethra to demonstrate the degree of urethral hypermobility (associated with stress urinary incontinence), with an angle change >30° being a positive result.
- Pediatric Foley catheter test: This test is used to screen for intrinsic sphincteric deficiency, a subtype of stress incontinence. An 8-French pediatric Foley catheter is placed in the bladder, the balloon is inflated, and the catheter is gently withdrawn. If the catheter, with its bulb inflated, can be easily extracted from the urethra, the test is positive, suggesting intrinsic sphincteric deficiency.
- Investigations
- Urinalysis with culture: rule out UTI
- Urodynamic studies: IUP does not rise with (or rise to the same degree as) abdominal pressure. PVR is normal.
- Treatment
- Conservative
- Behavioral modification (Scheduled urine visits, controlled fluid intake)
- Pelvic floor muscle strengthening (Kegel exercises)
- Weight loss
- Use of pads, such as diapers, condom catheters
- Dietary adjustments, such as eliminating caffeine and other irritants
- Pessary (when in conjunction with Pelvic Organ Prolapse)
- Pharmacologic management: Alpha-adrenergic agonists, such as phenylpropanolamine; duloxetine
- Surgery
- Urethral bulking agents
- Retropubic urethropexy
- Sling procedures: Pubovaginal (autologous) or mid urethral (synthetic)
- Conservative

Urge Urinary Incontinence
Urge urinary incontinence is involuntary leakage accompanied by or immediately preceded by a perceived, strong imminent need to void. It differs from Overactive bladder (OAB) which is just increased urgency with or without incontinence. Patients with urge urinary incontinence have OAB but not all patients with OAB have urge urinary incontinence. Most causes are idiopathic and multifactorial. The first step in urge urinary incontinence is to get a urinalysis to rule out sensory irritative incontinence (caused by UTI, urolithiasis, tumors etc.) that presents the same as urge urinary incontinence. Pharmacologic management is preferred in the treatment of urge urinary incontinence.
The NOBLE study found that 16.5% of adults met the cutoff criteria for OAB (8 times per day). M:F ratio is 1. However, women are more likely than men to be incontinent. Overweight individuals are also more likely to be incontinent.
- Medical Causes (DIAPPERS)
- Dementia/Delirium (or other functional inhibitive handicaps. They are physically or mentally incapable to get to the restroom)
- Infection (UTI)
- Atrophic vaginitis
- Psychological
- Pharmacological (EtOH, Caffeine, alpha blockers, ACEIs, CCBs, COX-2 inhibitors, Diuretics, Narcotic analgesics, TZDs)
- Endocrine (DM, Hypothyroidism)
- Restricted mobility
- Stool impaction (due to irritation of the detrusor or physical impaction of the urethra)/ Stones (renal calculi)
- Others – Neurological conditions such as stroke, Parkinson disease, or multiple sclerosis which can cause detrusor instability
- Patient history
- Elderly
- Post-menopausal
- History of bladder surgery (possible iatrogenic urethral compression that can cause detrusor instability)
- Signs and symptoms
- Urgency
- which prompts them to need the bathroom enough to interfere with daily activities
- Waking up to urinate (Nocturia)
- Incontinence
- large amount of urine lost during an episode
- Other UTI symptoms e.g. dysuria, increased frequency
- Urgency
- Physical examination
- Mostly unremarkable
- External genitalia is normal. May have signs of atrophy
- No vagina diverticula
- Bulbocavvernous and anocutaneous reflexes are normal indicating an intact S2-S4/pudendal circuit
- Valsava during the vaginal examination to rule out stress UI
- Q-tip test is negative in pure urge UI
- Investigations
- Urinalysis
- Urodynamic studies: if suspecting a neurologic cause
- Involuntary detrusor contractions despite low urinary volume in bladder
- Treatment
- Conservative management
- Pelvic floor muscle strengthening (Kegel’s)
- Avoid caffeine
- Behavioral modification (Scheduled urine visits, controlled fluid intake)
- Weight loss
- Pharmacologic
- Anticholinergics (Cornerstone of management – Tolterodine, Fesoterodine, Oxybutynin)
- Beta-3 adrenergic agonists (Mirabegron/”Myrbetriq”– relaxes the dome of the bladder)
- Tricyclic antidepressants (Imipramine – preferred if in combination with stress urinary incontinence)
- Topical estrogens (considered in patients with concurrent atrophic vaginitis)
- Surgical
- Sacral neuromodulation
- Tibial nerve stimulation
- Onabotulinum toxin A bladder injections
- Augmentation cystoplasty
- Conservative management
Overflow Urinary Incontinence
Overflow urinary incontinence is the involuntary leakage of urine from an overdistended bladder. Pathophysiologically it is due to detrusor insufficiency (bladder hypotonia) or detrusor areflexia (neurogenic bladder). Because the bladder pressure in these patients is at maximum, any intra-abdominal pressure increase causes some features resembling Stress UI. The difference with bypass urinary incontinence is that these patients are unable to go whenever they want to. It is important to get an ultrasound of the bladder for post-void residual. Treatment is dependent on the underlying cause.
- Causes
- Neurologic (Lower motor neuron disease, Autonomic neuropathy, Multiple sclerosis, Spinal cord lesion)
- Obstruction (Pelvic mass, fecal impaction, urethral stricture)
- Iatrogenic (post-surgical urethral obstruction, post-op overdistension)
- Pharmacologic (anticholinergic, alpha-adrenergic agonists, calcium channel blockers, opioid analgesics, epidurals)
- Obstetric risk factors for overflow urinary incontinence
- Primipara
- Prolonged second stage of labor
- Epidural
- Instrumental delivery
- Caesarean delivery
- Patient history
- Primipara with prolonged second stage of labor +/- epidural
- Medications (anticholinergics, epidural, spinal anaesthesia)
- Recent surgery (abdominopelvic surgery)
- Signs and symptoms
- Incontinence: constant slow loss of urine
- Inability to void: If the patient is able to void there is difficulty in initiating and maintaining a stream
- Features of stress urinary incontinence (due to increased bladder pressure)
- There may be a desire to void
- Physical examination
- External genitalia are usually normal
- No vaginal diverticuli
- Bulbocavernous reflex may be abnormal (indicating a neurologic etiology)
- Investigation
- Post-void residual: Mandatory. Volume ≥ 50 mL
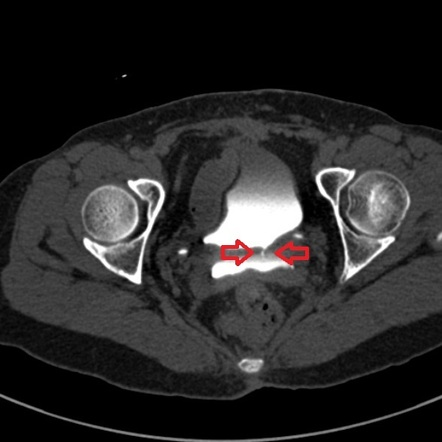
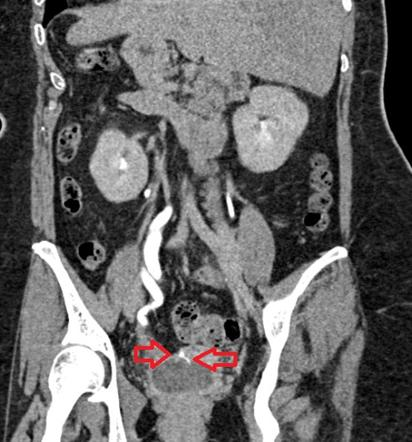
- CT KUB: if obstruction is suspected (to identify the site of obstruction
- Urodynamic studies: Lack of involuntary contractions despite a large volume of urine in the urethra
- Serum blood urea nitrogen and creatinine: if obstruction is suspected to assess renal function
- Treatment
- Temporary Overflow UI
- Intermittent self-catheterization or Foley catheter
- Cholinergic (Bethanechol)
- Permanent Overflow UI
- Long-term intermittent self-catheterization
- Placement of a suprapubic catheter
- Urinary obstruction
- Surgical correction
- Temporary Overflow UI
Bypass Urinary Incontinence
Bypass incontinence is the involuntary leakage of urine occurring when the normal continence mechanism is bypassed. Usually due to fistulas, which become apparent between 1-2 weeks post-op or after the inciting event. The risk for developing fistulas following surgery is higher in women with pre-existing pelvic pathology (endometriosis, PID, pre-op radiation, etc.).
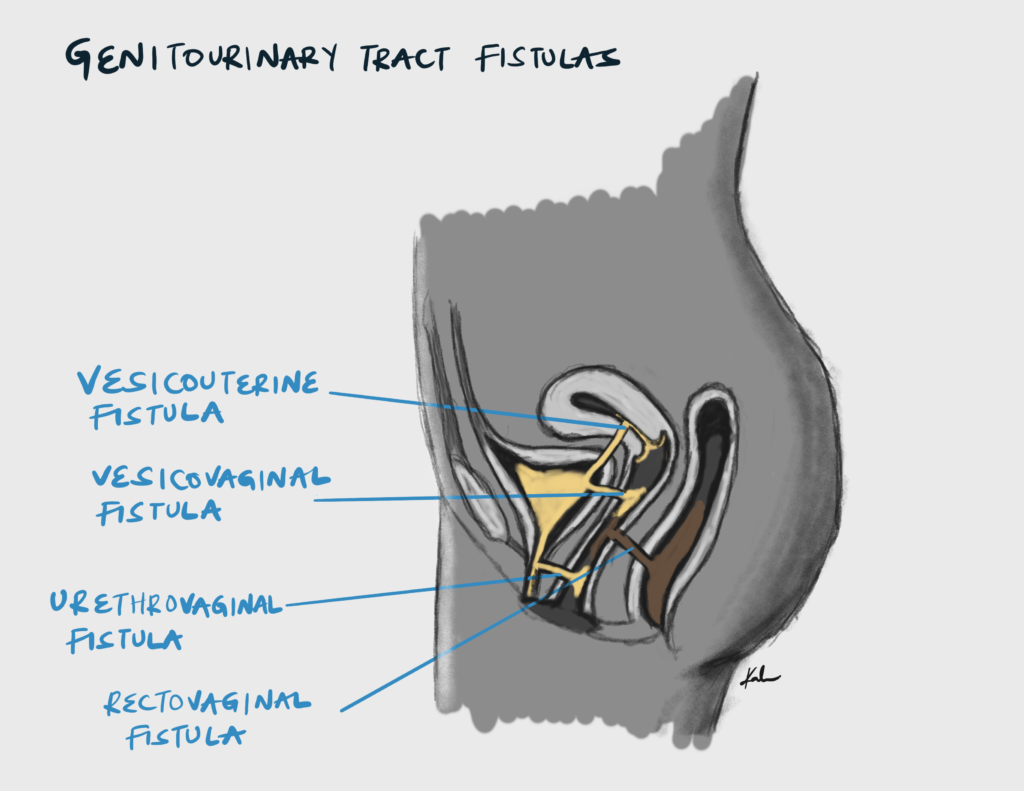
- Causes
- Obstetric trauma following complicated labor (MCC in the developing world due to obstructed labor, prolonged second stage, operative delivery, etc.)
- Pelvic surgery (Hysterectomy – MCC in the developed world)
- Pelvic radiation
- Signs and symptoms
- Incontinence is similar to overflow incontinence
- However, the patient will be able to void when desired
- Investigations
- Urinalysis and culture: rule out concurrent UTI
- Double dye test: pack the vagina with sterile gauze and give dye intravesical via foley or Per Oral
- Instillation of methylene blue into the bladder: identifies vesicovaginal fistula
- Methyleneblue crosses from the bladder and into the vagina staining the gauze blue
- PO Phenazopydidine (Pyridium): identifies ureterovaginal fistula
- Pyridium crosses the uterus into the vagina staining the tampon orange
- Instillation of methylene blue into the bladder: identifies vesicovaginal fistula
- CT KUB or IV pyelography or Cystoscopy or Retrograde pyelogram
- Retrograde pyelography is the most definitive test to diagnose a ureterovaginal fistula
- Treatment
- Surgical correction

Mixed Urinary Incontinence
This is the involuntary leakage of urine caused by a combination of stress and urge urinary incontinence. Treatment and management focus on the most dominant symptoms.
Functional Urinary Incontinence
This is the involuntary leakage of urine due to environmental or physical barriers to toileting. This type of incontinence is sometimes referred to as toileting difficulty.
The history may suggest physical or cognitive impairment. Underlying causes should be addressed and alleviated if possible.

