- Briefly describe Spirochetes
- Spirochetes is derived from the word “Spirochaetae”, having the latin root “Spira” meaning spiraled or coiled, and the Greek root “Khaite” meaning long hair or mane (Thus “Coiled hair”)
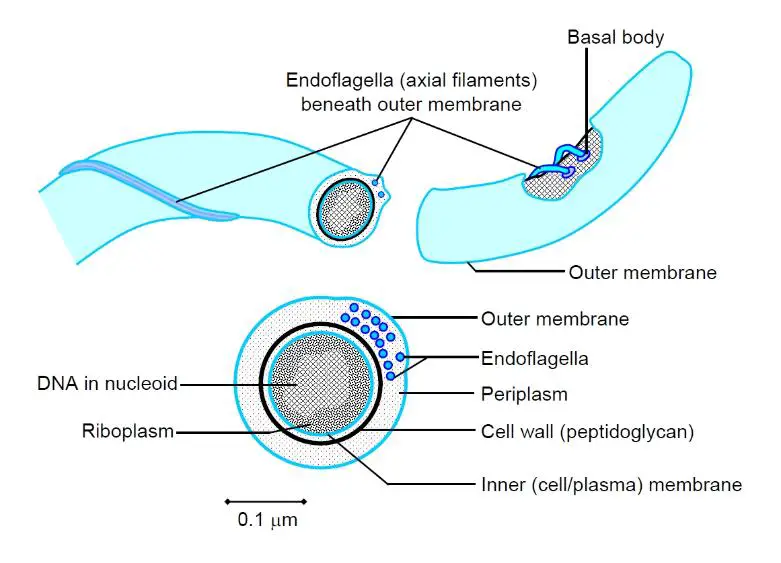
- They are long, thin, tightly coiled helical (corkscrew) bacilli with tapered ends.
- They are motile and have rational movement.
- Flagella (Endoflagella) are located within the periplasm.
- Disease associated genera include
- Treponema spp.
- Borrelia spp.
- Leptospira spp.
- Using a diagram, describe the structure of Spirochetes
- Structure: Sheath, Outer membrane, Periplasmic space, Periplasmic flagellae (Axial fibrils, Axial filaments, Internal flagella, endoflagella), Peptidoglycan (Cytoplasmic membrane layer), Membrane proteins, protoplasm
- List the virulence factors associated with Spirochetes
- Outer membrane proteins: Adherence to host cell surface
- Hyaluronidase: Perivascular infiltration
- Coating with host cell fibronectin: Protective against phagocytosis
- Briefly describe Treponemes
- All treponemes are morphologically similar and share antigens and significant DNA homology.
- They give cross-reactions in serological tests.
- They are differentiated by geographical location and clinical features.
- Non-pathogenic species
- Normal flora
- Oral cavity: Treponema microdentium, Treponema macrodentium
- Genital tract: Treponema calligyrum, Treponema genitalis
- Saprophytes (Used in lab experiments)
- Reiter’s strain (Antigenically related to Treponema pallidum)
- Nichol’s Treponema pallidum
- Normal flora
- Pathogenic species
- Treponema pallidum subsp. pallidum (Syphilis)
- Treponema pallidum subsp. endemicum (Bejel)
- Treponema pallidum subsp. pertenue (Yaws)
- Treponema carateum (Pinta)
- List the virulence factors of Treponema pallidum
- LPS
- Membrane proteins: Covalently bound lipids at amino terminals that anchor the proteins to the cytoplasmic outer membrane, kept inaccessible to antibodies
- Hyaluroinidase: Contributes towards its invasiveness
- Cardiolipin: Important component of treponemal antigens
- No important toxins
- Briefly describe the epidemiology of Syphilis
- Found worldwide, 3rd most common STI after Chlamydia and Gonorrhea. Prevalent in 6.4% of HIV-1 and 1.6% of HIV-negative individuals in Kenya (2011). Disease incidence has decreased sharply with penicillin therapy. Periodic increases have been observed with changes in sexual practices. Natural syphilis is exclusive to humans and has no other known natural hosts
- Briefly describe the pathogenesis of syphilis
- Incubation: varies from 9-90 days (Averages 3 weeks – 21 days)
- Initial contact → penetration of mucous membranes and damaged skins → enters lymphatics → bloodstream → organs
- Infects the endothelium of small blood vessels causing endarteritis (Tertiary syphilis!)
- Tissue destruction and lesions are due to immune response against treponemal antigens (inflammation)
- Organism aren’t eliminated despite the vigorous host response, and can persist for decades
- Classify Syphilis according to the mode of acquisition
- Sexually Transmitted Syphilis: The Organism enters through broken skin of genitalia or elsewhere depending on sexual practice → Multiply at entry site → Long incubation period (9-90 days) where individual is non-infectious
- Congenital Syphilis: Transmitted at any time throughout pregnancy. Associated with septicemia in foetus and widespread dissemination.
- Occupational Syphilis: Occurs in medics and paramedics in handling a case of secondary syphilis. Infection is through lesions on the palm of the health workers or on any other exposed body part
- What are the complications (or possible outcomes) of Congenital Syphilis
- Death of foetus (Miscarriage)
- Stillbirth at term
- Born alive with latent infection, OR develops signs and symptoms shortly after birth or within 2 years of infection: Failure to thrive, skin rash, Saddle nose, Organomegaly, Eye defects, blindness, Hutchinson teeth, Snuffles (Syphilitic rhinitis), Saber shin (Bilateral destruction of medial tibial metaphyses -Wimberger sign) Sensorineural deafness. Preventable through screening and treatment of pregnant women
- Hutchinson’s triad: Hutchinson incisors, Interstitial keratitis, Sensorineural deafness
- Outline the laboratory features of Treponema pallidum
- Specimen: Fluid, scrapings from lesions
- Demonstration of Treponema pallidum in specimen
- Dark-field microscopy: Spiral cells with typical motility (in primary or secondary stages)
- Immunofluorescence: Spiral cells with typical motility (Stained with fluorescein labelled anti-treponeme antibody, high sensitivity)
- Silver staining and microscopy: Spiral cells with typical microscopy
- Electron and phase contrast microscopy
- Serology – Most effective, does not distinguish syphilis from other treponemes
- Non-treponemal tests: Detects reagin Ab using cardiolipin Ag, cardiolipin is present in large amounts of mammalian mitochondira, probably formed as a result of tissue destruction caused by the infection
- Standard non-specific tests
- Venereal Disease Research Laboratory (VDRL): Flocculation read microscopically, Quantitative and qualitative. False positive: EBV, Hepatitis, Drugs, Rheumatic Fever, SLE, Leprosy, Tuberculosis, Pregnancy, IVDU
- Rapid Plasma Reagin (RPR card test): Read microscopically, measures IgG and IgM against Cardiolipin-Cholesterol-Lecithin. False positives: EBV, Hepatitis, Drugs, Rheumatic Fever, SLE, Leprosy, Tuberculosis, Pregnancy, IVDU. More sensitive during the middle (Secondary) stage of syphillis
- Wasserman test
- Kahn test
- Specific Treponemal tests – used as a follow up to positive VDRL to rule out false positives, Qualitative (Negative or positive, no titres), remain positive for many years (IgG persists)
- Treponema pallidum hemagglutination test (TPHA): Serum added to red cell that have been coupled with treponemal antigens, antibody-antigen interaction results in agglutination, positive 4 weeks post-exposure
- Fluorescent treponemal antibody absorption test (FTA-ABS): positive 10 days (3 weeks) post exposure)
- Treponema pallidum particle agglutination (TP-PA)
- ELISA: detects specific treponemal antibodies
- Rapid immunochromatographic tests: Currently all such tests detect specific treponemal antibodies
- Outline the stages of syphilis
- Primary Syphilis: Chancre (Primary sore, hard chancre), **Rapid organism multiplication, 10-90 days post-infection (**3 weeks average)
- Secondary Syphilis: Generalized rash and lymphadenopathy, Snail-tract ulcers, Condylomata lata, 6-weeks post-chancre
- Latent Syphilis: Clinically well but have asymptomatic syphilitic infection, infectiousness declines over time, detected by serological tests, may develop into Cardiovascular or neurosyphilis
- Tertiary (Late) syphilis: 10-20 years after primary disease
- Cardiovascular syphilis: Aortitis, incompetence, aortic (Mycotic) aneurysm
- Neurosyphilis: Meningovascular syphilis (Menigitis, Cranial nerve involvement), Tabes dorsalis (DCML), General paresis of the insane (Brain parenchyma involved, Personality changes, dementia)
- Outline the treatment for the different stages of Syphilis
- DOC: Penicillin
- Primary or Secondary: Benzathine penicillin IM
- Latent or tertiary syphilis: Benzathine penicillin IM
- Neurosyphilis: Penicillin G IV
- Alternatives: Tetracycline, Erythromycin
- Briefly describe the non-venereal diseases caused by Treponema
- Bejel/ Endemic Syphilis – Africa, Asia
- Causative agent: Treponema endemicium
- Endemic: Dry subtropical or temperate areas of Middle East, India, Asia and parts of Africa
- Transmission: contact with mucosa lesions, or contaminated eating utensils or water
- Occurs in childhood, associated with poor hygiene,
- Yaws – Africa, Asia
- Causative agent: Treponema pertenue
- Endemic: Humid tropics, C Africa, S america, SE asia, Parts of Indian subcontinent
- Acquired in childhood through contact with infectious skin lesions, Incubation of 3 weeks
- Painless nodules widely distributed initially, later later inflammatory lesions of skin and bones
- Pinta – South America
- Causative agent: Treonema carateum
- Most benign of the endemic treponematoses, affecting only the skin. Incubation of 2-3 weeks
- Endemic: South and Central America
- Spread: Contact with infected skin
- Primary lesion: Papule or erythematous plaque on exposed surfaces of the legs, foot, forearm, or hands, which slowly enlarge, becoming pigmented and hyperkeratotic
- Secondary lesions: Disseminated, of similar appearance, appear 3-9 months later
- Late/ tertiary pinta: Disfiguring pigmentary changes, and atrophic lesions
- Bejel/ Endemic Syphilis – Africa, Asia



