Overview
Malnutrition is defined as a lack of macronutrients (calories) OR a lack of micronutrients (Vitamins, minerals). For this discussion, we will consider undernutrition in terms of inadequate consumption of macronutrients.
- Top 5 concerns in SAM
- Hypothermia
- Dehydration due to vomiting and diarrhoea
- Anaemia (can request for stool for O/C – look for hookworms)
- Infection
- Hypoglycemia
- Investigations
- CBC: look for anemia due to Iron deficiency, folate/B12 deficiency (transfuse if Hb < 4mg/dL); Signs of infection
- Random Blood Sugar: look for hypoglycemia (cut-off at 3 mmol/L)
- U/E/C: look for electrolyte disturbances
- TFTs: look for iodine deficiency
- Liver Function Tests: for albumin
- Total protein: usually low
- Stool studies: look for Gastrointestinal infections
- Other labs as indicated by individual patient status (history/symptoms/physical exam)
Weight, height, and age
For children, percentiles using growth charts are used to determine whether a child has undernutrition or is obese
- Weight for height (W/H)
- Low W/H = wasting (acute malnutrition)
- Weight for age (W/A)
- Cannot distinguish acute from chronic malnutrition. Used to monitor growth in the MCH booklet
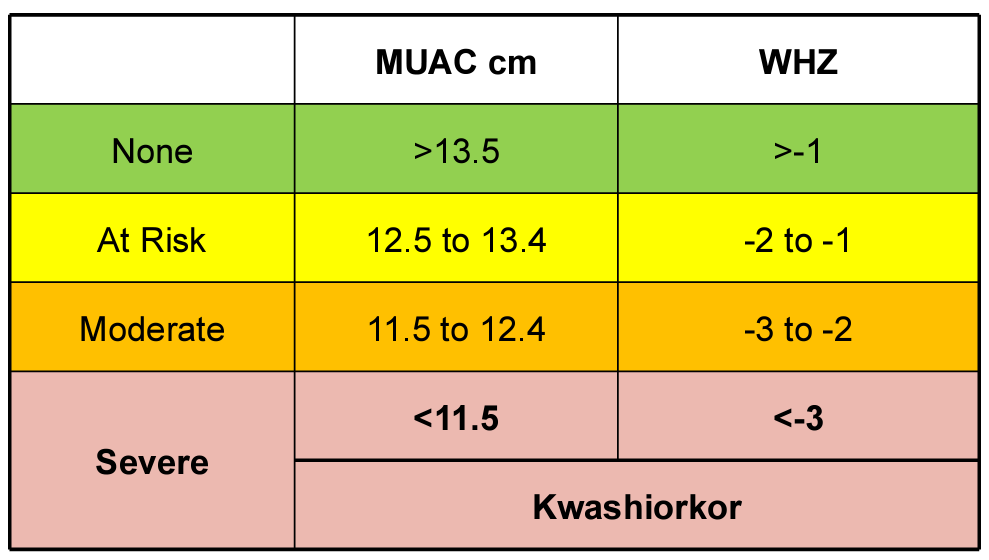
Mid-upper arm circumference (MUAC)
Mid-upper arm circumference (MUAC) is used to quickly ass ess the nutritional status in emergency setting.
The BMI scale can be used for adults and in some extent for children
| BMI | Category |
|---|---|
| > 30 | Obese |
| 25 – 30 | Overweight |
| 18.5 – 25 | Normal |
| < 18.5 | Underweight |
Signs of undernutrition
Worldwide; approximately 20% of children under 5 years are wasted (W/H); 32% are stunted (H/A). By 1 year of age undernutrition is likely to have caused significant damage that can affect future health, cognition, welfare, and well-being.
- Wasting
- Weight for age/height < 2 SD below the normal weight for a child that age.
- Stunting
- Height for age < 2 SD below the normal height for a child that age
- What is the measure of acute malnutrition?
- Wasting (W/H)
- What is the measure of chronic malnutrition?
- Stunting (H/A)
- Most immediate consequence of undernutrition?
- Premature death
Micronutrients of high concern in undernutrition
In the developing world, GI parasites can contribute and exacerbate undernutrition
- Zinc
- Important during rehydration/refeeding process
- Urinary zinc is proportional to overall zinc status
- Iodine
- Deficiency results in goiterous hypothyroidism, and developmental issues (particularly in cognition)
- Vitamin A
- Deficiency causes night blindness, keratinous changes of cornea, conjunctivae, skin and increased susceptibility to GI infections
- Iron
- Reduced synthesis of heme → microcytic anemia
- Folic acid
- Megaloblastic anemia
Severe Acute Malnutrition (SAM)
Worldwide, SAM is the leading cause of death among children <5 yrs. Malnutrition causes about 5.6 – 10 million deaths per year, with severe malnutriotion contributing to about 1.5 million.
SAM is defined as Severe wasting with a W/H < 3SD OR W/L <3SD OR MUAC <11.5, OR Gross severe Wasting OR Bilateral oedema w/o any other explainable cause
- Factors that contribute towards SAM
- Poverty
- Single mothers
- Single parents
- Displacement by clashes
- Birth out of wedlock
- Mother and child staying separate from father due to working conditions
- Sharing of income with extended families
- Precipitating factors for SAM
- Lack of food (famine, poverty)
- Inadequate breast feeding
- Wrong concepts about nutrition
- Diarrhoea and malabsorption
- Infections (worms, measles, TB)
The term Protein Energy Malnutrition is outdated. PEM referred to a life-threatening deficiency of macronutrients, which is practically always accompanied by deficiency of some or many micronutrients. It was defined by the WHO as a cellular imbalance between supply of nutrients and energy and the body’s demand for them to ensure growth, maintenance and normal functioning.
A patient may present with features of both Marasmus, Kwashiorkor, or both.
| SAM (Non-oedematous/ Marasmus ) | Oedematous SAM (kwashiokor) |
|---|---|
| Weight loss; Listlessness | Weight loss; lethargy, irritability |
| Loss of skin tugor/ wrinkling | Edema; flabby skin tissue |
| Simian facies | Moon facies |
| Pt appears dehydrated | Pt appears volume overload |
| Constipation or starvation diarrhoea | Diarrhoea, vomiting |
| Abdomen may be distended or flat | +/- Hepatomegaly |
| Low muscle tone/hypotonia | Loss of muscle tissue |
| Hypothermia | Dermatitis – hyper-pigmenation and desquamation |
Clinical Features and Pathophysiology
- Skin changes
- Ulcerations (Zn deficiency)
- Excessive dryness (atrophy of sweat and sebaceous glands)
- Hyperpigmentation, erythema, duskiness of exposed areas (Niacin deficiency)
- Cracking and fissuring
- Generalized hypopigmentation (due to stretching of the skin by edema)
- Hair changes
- Brittle hair (impaire keratin synthesis due to cysteine and methionine deficiency)
- Hair color pigment changes to reddish or grey (Tyrosine deficiency)
- Dullness and lack of lustre (due to withering of hair cuticle)
- Oedema
- Hypoalbuminemia causing reduced oncotic pressure
- Hypovolemia causing activation of RAAS
- Pump malfunction causing vessel leak
- Free radicals damage cell membrane
- Diarrhoea
- Recurrent infection (low secretory IgA, reduced acid production in stomach)
- Malabsorption (deficeincy pancreatic enzymes)
- Villous atrophy
- Disaccardases (lactase) deficiency
- Candida albicans overgrowth
- Recurrent infections
- Atrophy of thymo-lymphatic glands
- Reduced phagocytic and bactericidal activity
- Reduced complement
- Reduced cytokines
- Anaemia
- Dietary deficiency of iron and folate
- Parasitic infestations (hookworm)
- Malabsorption due to recurrent diarrhoea
- Reduced protein intake and synthesis
- Apathy
- Muscle weakness and easy fatiguability (hypokalemia)
- Mental slowing (lack of stimulation and deprivation causing reduced growth of brain)
- Low BMR
- Zinc deficiency
- Consequences of infection
- Poor appetitie
- Dietary restriction (misconception of low feeds during diarrhoea
- Malabsorption of nutrients
- Frank protein-losing enteropathy (measles, HIV)
- Leads to a vicious cycle
- Consequences of Zinc deficiency
- Reduced appetite
- Reduced immunity
- Reduced GI function (longer period of diarrhoea)
- Reduced ability to gain weight (even with adequate feeding)
- Consequences of copper deficiency
- Anemia
- Poor bone growth
- Consequences of selenium deficiency
- Reduced cardiac muscle function
- Renal function
- Reduced GFR and Renal plasma flow rate (due to dehydration)
- Overflow aminoaciduria
- Insufficient excretion acid load
- Reduced ability to concentrate urine
- Decreased plasma urea, increased sodium and water retention
- Hypokalemia and high total body water
- Na+/K+ pump on energy saving mode causing low intracellular potassium and high intracellular sodium
- Hepatomegaly
- Fatty liver
Treatment of SAM
Management of SAM is phased to prevent Refeeding syndrome. Takes place in 2 phasee: stabilization and rehabilitation. During the stabilization phase, start with smaller and more frequent feeds before phasing up to larger and less frequent feeds as tolerated. The pt is discharged after 6 weeks and continued on a feeding protocol for catch up.

- Stabilization phase (week 1)
- Correct hypoglycemia: if < 3mmol/L or if AVPU <A give 5ml/kg of 10% dextrose, oral/NG glucose or feeds should be started no later than 30 minutes
- Correct hypothermia: if axillary temp <35 C use warm blankets, warm fluids, heater
- Correct Dehydration: preferably w/PO fluids (ReSoMal); IV fluids are necessary if in shock, transfuse with with whole blood 10mls/kg in 3hrs + Furosemide 1mg/kg if Hb /, 4g/dL.
- Correct electrolyte imbalances: use commercial F75 OR mineral mix and 4mmol/kg/day of potassium added to feeds. Do frequent electrolyte checks.
- Antibiotics for any suspected infection: IV Penicillin (or Ampicillin) and Gentamicin, Nystatin/Clotrimazole for oral thrush, Albendazole after 7 days treatment. TEO (+ Atropine) for pus/ulceration in the eyes
- Correct micronutrient deficiency: Vitamin A PO if eye signs on admission and days 2 and 14, if no RUTF or F75/F100 give Multivits for at least 2 weeks, Folic acid 2.5mg for alternate days. Give Iron only when child is gaining weight and no RUTF.
- Begin cautious feeding: F75 3 hourly for at least 7 days. (130mls/kg/day, 100mls/kg/day if severe edema or face)
- Achieve catch-up growth: F100 or RUTF 8 hourly. They are very high in energy and proteins.
- Provide sensory stimulation and emotional support
- Prepare for follow-up after recovery
- Rehabilitation phase (week 2 – 6)
- Continue Nutrition: F100 or RUTF diet (100 kcal/kg/d)
- Iron replacement
- When is the child transitioned from cautious feeding to catch-up growth?
- When they start tolerating feeds
- When there is weight gain
- When there is resolving oedema
Refeeding syndrome
A complication of nutritional rehabilitation causes severe hypophosphatemia. Diagnosis is by Low serum PO4 in the setting of signs and symptoms.
- Signs and symptoms
- Weakness
- Neutrophil dysfunction
- Rhabdomyolysis
- Arrhythmia
- Seizures
- Altered mental status
- Cardiorespiratory failure
- Treatment
- Administer Thiamine
- Replace phosphate
- Frequent PO4 checks
Noma
Noma is a rapidly progressive, necrotizing, ulcerating gingival and perioral inflammation seen in patients with SAM. It is usually preceded by an infection or debilitating illness.

- Signs and symptoms
- Gingivitis
- Halitosis
- Fever
- Anaemia
- Treatment
- Local wound care
- Penicillin + Metronidazole
- Treat the underlying infection

