Rheumatoid Arthritis
Rheumatoid arthritis is a chronic systemic inflammatory disease characterized by severe symmetrical peripheral joint pain and deformation due to erosive arthritis. It is progressive and drastically reduces quality of life, hence early referral and treatment is important. It is linked to HLA DR4/DR1, which when present is makes RA more severe. Early RA presents with joint inflammation with no damge. Later during the disease course the joints become damaged and deformed. Seronegative RA affects < 5% of individuals with RA.
The global prevalence of RA is is 1%, and is higher in smokers. It affects women more than men (2:1) and has a peak onset in the 50 – 60s. 40% of patients with RA presents with extra-articular signs and symptoms.
Features of rheumatoid arthritis
| Component | Rheumatoid arthritis |
|---|---|
| Systemic | Yes. Fatigue, malaise, weakness, anaemia of chronic disease, felty syndrome etc. |
| Location | Small joints of hands. Large joints affected lest frequently. DIPs and lower back notably spared. |
| Inflammation | Prominent. Joints warm and erythematous |
| Chronicity | Chronic, insidious and progressive. Pain is worse in the morning. |
| Evidence of trauma | No |
Summary of diagnostic criteria for RA (≥ 6 points required)
| Category | Component |
|---|---|
| A | Joint involvement (Number of joints, large vs small) |
| B | Serology (RF and anti-CCP) |
| C | Acute phase reactants (CRP and ESR) |
| D | Duration of symptoms (less than or more than 6 weeks) |
- Patient history
- Recurrent mono/polyarthritis (palindromic RA)
- Persistent monoarthritis (of the knee shoulder or hip)
- Vague limb girdle aches (polymyalgic onset)
- Recurrent soft tissue problems e.g. frozen shoulder, carpal tunnel syndrome, de Quervain’s tenosynovitis
- Signs and symptoms
- Joint pain, swelling and stiffness
- Symmetrical
- Affects small joints of the hands and feet (but can affect larger joints)
- Worse in the morning
- Fatigue
- Fever
- Weight loss
- Chest pain (pericarditic and pleuritic)
- Joint pain, swelling and stiffness
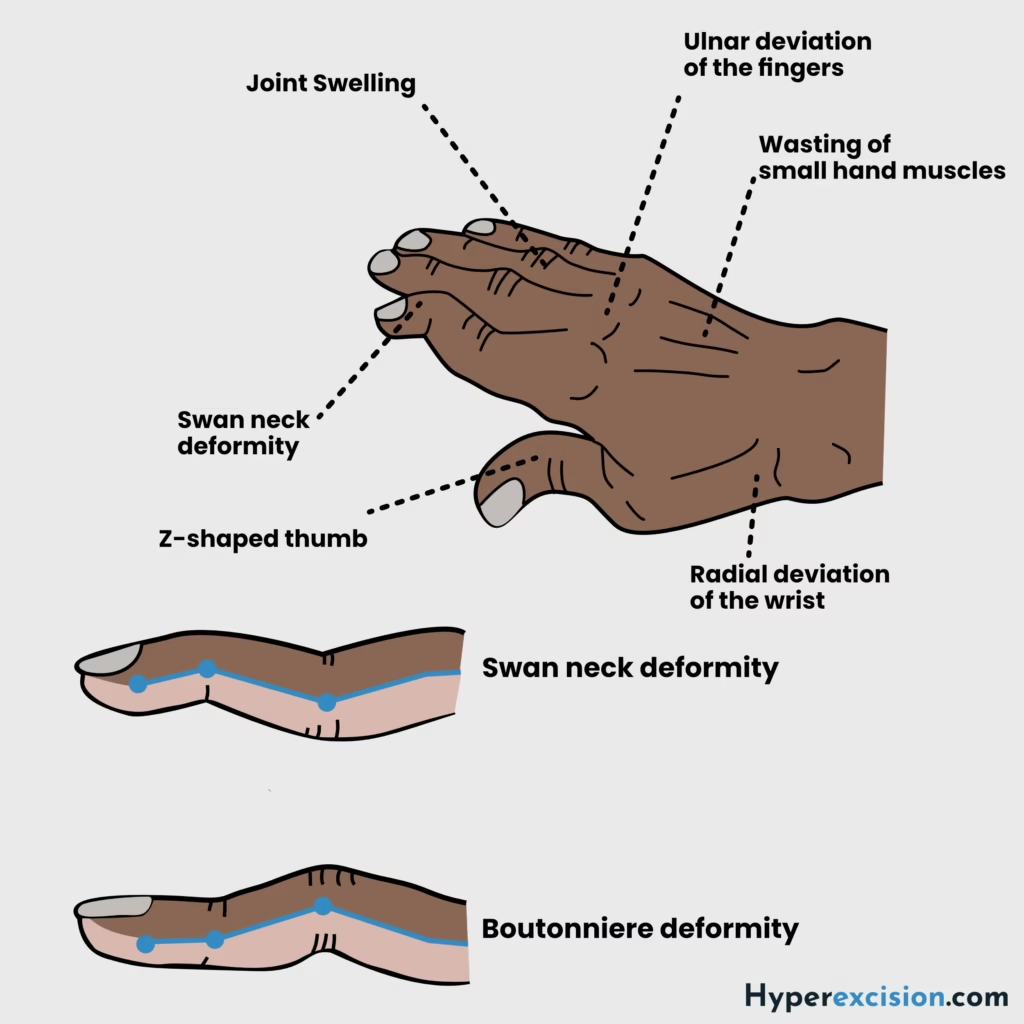
- Physical examination
- Symmetrically swollen MCP, PIP, wrist or MTP joints
- Ulnar deviation and subluxation of wrist and fingers
- Boutonniere and swan-neck deformitis of fingers
- Rheumatoid nodules on bony prominences
- Z-deformity of thumbs
- Foot changes (similar to hand changes)
- Atlanto-axial joint sublaxation (rare)
- Baker’s cyst
- Differentials
- Psoriatic arthritis: negative rheumatoid factor, psoriasis and involvement of DIPs
- Reactive arhtritis: acute onset, uveitis and urethritis following infection
- Viral polyarhtritis
- Gout: acute onset, older patient affecting the knee or first MTP. Usually self-limited
- CPPD
- SLE: similar patient group, malar rash and non-erosive findings
- Osteoarthritis: worsens with use, chronic onset, older patient, and overweight
- Investigations
- Rheumatoid factor: positive in 70%. High titres are associated with severe disease, erosions and extra-articular disease
- Antinuclear antibodies: to rule out SLE
- Anticyclic citrillinated peptide antibodies (anti-CCP): highly specific for RA (98%) with a moderate sensitivity of 70-80%.
- Complete blood count
- Anaemia of chronic disease
- Thrombocytosis
- ESR
- Elevated
- CRP
- Elevated
- Arhtrocentest with analysis
- Yellow cloudy fluid
- Elevated WBC (not as high as septic arthritis)
- X-ray: best initial diagnostic test.
- Soft tissue swelling
- Juxta-articular osteopaenia
- Reduced joint spacing
- Bony erosiions
- Sublaxation
- Complete carpal destruction (late)
- Ultraound: to detect tenosynovitis and bone erosions
- MRI: most accurate imaging tool for the detection of early RA. Detects synovitis and bone erosions
- Liver function tests: before starting MTX
- Hepatitis serology: before starting MTX
- Pregnancy test: before starting MTX
- Supportive treatment
- Early referral to a rheumatologist
- Measure disease activity using DAS28
- Referral to physiotherapist
- Referral to occupational therapist
- Manage risk factors e.g. smoking
- Counsel about risk factors of medication
- Pharmacological treatment
- Disease-modifying antirheumatic drugs (DMARDs): first-line agents. Should be started within 3 months of persistent symptoms. Takes 6 – 12 weeks for symptomatic benefit They can be combined. Early DMARDs improve long-term outcomes
- Methotrexate: mainstay of treatment
- Sulfasalazine
- Hydroxychloroquine
- Leflunomide
- Biologic agents: early biologics improve long-term outcomes
- TNF-a inhibitors e.g. infliximab, etanercept, adalimumab (1st line)
- B-cell depletion eg. rituximab
- IL-1 and IL-6 inhibition e.g tocilizumab
- Inhibition of T-cell co-stimulation e.g. abatacept
- Intra-articular or Intramascular steroids: for acute exacerbation or as a bridge to DMARDs
- NSAIDs: included for symptom relief
- Surgery e.g. synovectomy, arthroplasties
- Disease-modifying antirheumatic drugs (DMARDs): first-line agents. Should be started within 3 months of persistent symptoms. Takes 6 – 12 weeks for symptomatic benefit They can be combined. Early DMARDs improve long-term outcomes
- Complications of rheumatoid arthritis
- Felty syndrome: RA + neutropaenia + splenomegaly. A sign of poorly controlled RA
- Carpal tunnel syndrome
- Atlanto-axial subluxation
- Progressive reduction in quality of life
Extraarticular manifestations of RA
| Classification | Extraarticular manifestations |
|---|---|
| Nodules | Elbow, lungs, cardiac, CNS, lymphadenopathy, vasculitis |
| Lungs | Pleural disease, intersitial fibrosis, bronchiolitis obliterans, organizing pneumonia |
| Cardiac | Ischemc heart disease, pericarditis, pericardial effusion, carpal tunnel syndrome, peripheral neuropathy, splenomegaly (including Felty’s syndrome) |
| Musculoskeletal | Carpal tunnel syndrome, peripheral neuropathy, osteoporosis |
| Ophthalmologic | Episcleritis, scleritis, scleromalacia, keratoconjuncitivitis sicca |
| Haematologic | Anaemia, splenomegaly (including Felty’s syndrome), amyloidosis |
Side effects of DMARDs
| Category | Side effects |
|---|---|
| General | Immunosuppression, pancytopaenia (especially if combined with methotrexate |
| Methotrexate | Pneumonitis, oral ulcers, hepatotoxicity, teratogenic |
| Sulfasalazine | Rash, reduced sperm count, oral ulcers, gastrointestinal upset |
| Leflunomide | Teratogenic, oral ulcers, hypertension, hepatotoxicity |
| Hydroxychloroquine | Retinopathy |
- Side effects of biological agents
- Serious infection
- Reactivation of TB and hepatitis B
- Worsening heart failure
- Hypersensitivity
- Injection-site reactions and blood disorders
- Evolution of ANA and reversible SLE-type illness