Rheumatic Heart Disease (RHD)
Rheumatic heart disease (RHD) is a chronic, systemic, immune-mediated condition that develops as a serious complication of rheumatic fever (RF), often following recurrent episodes of acute illness. It is the most significant consequence of acute rheumatic fever (ARF) and is characterised by permanent damage to the heart valves.
First we will discuss Acute Rheumatic Fever.
Acute Rheumatic Fever
Acute rheumatic fever (ARF) is an autoimmune inflammatory condition that results from an abnormal immunologic response to group A Streptococcus (GAS) infections. It affects multiple systems: Cardiac, neurologic, musculoskeletal and skin.
While anyone can develop ARF, the disease is most commonly seen in children aged 5-15 years of age and young adults. There is no gender predilection for ARF, but females are more likely to progress to RHD.
Etiopathogenesis
ARF commonly follows pharyngeal (or tonsillar) infection with group A Streptococcus (GAS). Untreated or inadequately treated GAS infection leads to the development of ARF around 2-4 weeks after initial infection.
Streptococcal skin infections, particularly impetigo, may also cause ARF in high-risk populations such as the Indigenous people of Australia.
- Factors that increase risk of GAS pharyngitis
- Overcrowding
- Poor sanitation
- Lack or inadequate access to healthcare
How does a sore throat cause systemic inflammation?
- Group A Streptococcus (GAS) produces M and M-like proteins, which serve as major virulence factors due to their strong anti-phagocytic properties. These proteins disrupt the immune response by destroying C3 convertase and inhibiting opsonization by C3b, allowing the bacteria to evade immune detection.
- However, B cells can generate antibodies against the M protein, which promote opsonization and enhance the recognition and destruction of the microorganism by macrophages and neutrophils.
- M proteins and other components of GAS share structural similarities with human tissues, especially those in the heart, joints, skin, and brain. This phenomenon is known as molecular mimicry.
- In particular, the M protein moiety and N-acetyl-β-D-glucosamine (NABG) of GAS species exhibit structural similarity to myosin causing carditis.
- Hence, antibodies formed against GAS antigens crossreact with self-antigens, leading to a dysregulated immune response.
- Ensuing inflammation and tissue damage causes:
- Carditis – inflammation of the endocardium, myocardium, and pericardium as well as heart valves (Mitral valve is affected most commonly and severely; Aortic valve is affected second most commonly). May progress to Rheumatic Heart Disease after multiple episodes of ARF.
- Arthritis – due to antibody-antigen complexes deposit in joints
- CNS manifestations (Syndenham chorea) – due to autoantibodies reacting with brain ganglioside. Mainly affects the basal ganglia
- Dermatological manifestations – Erythema marginatum (pink, non-itchy rashes) or subcutaneous nodules.
Note: Not every individual who has GAS pharyngitis develops ARF. Genetic susceptibility plays a role in disease progression
Histopathology
Carditis
Aschoff bodies
- Considered pathognomonic for rheumatic heart disease
- They are composed of multinucleated giant cells surrounded by macrophages and T lymphocytes
- Usually seen in the subacute and chronic cases
- Enlarged macrophages with condensed nuclei termed Anitschkow cells can be seen as well
Erythema marginatum
Polymorphous infiltrate of neutrophils and mononuclear cells in the papillary and upper half of the reticular dermis
Subcutaneous nodule
Edema, fibrinoid necrosis, and mononuclear cell infiltrate
Clinical Presentation
- Preceding, untreated GAS infection
- GAS Pharyngitis presents with:
- Fever and chills
- Throat pain
- Headaches
- Younger children may complain of GIT disturbances such as abdominal pain, nausea and vomiting
- GAS Pharyngitis presents with:
- Constitutional symptoms
- Fever and chills
- Fatigue
- Anorexia
- Migratory polyarthritis
- Usually the earliest manifestations of ARF (except in children)
- Painful involvement of large joints such as knees, ankles, elbows, or shoulder
- Joints are erythematous, swollen, and extremely tender
- Carditis
- Most significant complication of ARF.
- Younger children tend to develop carditis before arthritis hence cardiac symptoms may be the initial complaint.
- Symptoms depend on what part is affected: Pericardium, myocardium, endocardium, heart valves.
- Present with the following symptoms:
- Dyspnea on exertion
- Cough
- Palpitations
- Paroxysmal nocturnal dyspnea
- Chest pain
- Orthopnea
- Mitral valve is most commonly affected (50-60%) with regurgitation that initial effect; mitral stenosis follows progressive damage.
- Aortic valve involvement occurs in about 20% of cases; initially – aortic regurgitation then with progressive valvular damage – aortic stenosis.
- Tricuspid valve involvement occurs in 10% of cases and mostly presents as a regurgitation.
- As such on physical examination you expect:
- Mitral regurgitation – holosystolic murmur loudest at the apex and radiating to the left axilla
- Mitral stenosis – mid diastolic murmur
- Aortic regurgitation – early diastolic murmur best at the base of the heart and increased by the patient sitting forward
- Aortic stenosis – ejection systolic murmur; best heard over the carotid arteries as patient holds breath
- Tricuspid regurgitation – pansystolic murmur at the left sternal edge
- Carey Coombs murmur – soft mid-diastolic murmur; typically due to valvulitis, with nodules forming on the mitral valve leaflets causing valve thickening.
- Other findings on CVS examination
- Tachycardia
- Third heart sound
- Rales
- Lower limb edema
- Pericardial rub – indicating pericarditis
- Dermatological manifestations
- Subcutaneous nodules
- Associated with severe carditis; self limited
- Firm, painless lesions over joints, predominately on extensor surfaces
- Erythema marginatum
- Rare; self-limited
- Pink or pale red annular, non-pruritic macular rash; fade in the centre but remain red at the edges as they advance ; found on the trunk and proximal end of limbs.
- Appear on one body part, fade, and reappear elsewhere very quickly.
- Subcutaneous nodules
- Sydenham chorea (St Vitus dance)
- Rapid, irregular, aimless involuntary movements of the arms and legs, trunk, and facial muscles. Emotional lability and personality change are present.
- Late manifestation; self-limited
- The motor symptoms usually disappear during sleep and may be partially suppressed by sedation.
Evaluation
Revised Jones Criteria
| Low risk population | Moderate to high risk population | |
|---|---|---|
| Major criteria | Carditis (clinical or subclinical i.e detected by echocardiography) | Carditis (clinical or subclinical i.e detected by echocardiography) |
| Polyarthritis | Monoarthritis, polyarthritis, or polyarthralgia | |
| Chorea | Chorea | |
| Subcutaneous nodules | Subcutaneous nodules | |
| Erythema marginatum | Erythema marginatum | |
| Minor criteria | Polyarthralgia | Monoarthralgia |
| Fever ≥38.5° C | Fever ≥38°C | |
| ESR >60 mm/h and/or CRP >3.0 mg/dL | ESR >30 mm/h and/or CRP >3.0 mg/dL | |
| ECG with prolonged PR interval | ECG with prolonged PR interval |
Low-risk populations have an ARF incidence of ≤ 2 per 100,000, and moderate- and high-risk populations have an ARF incidence of >2 per 100,000.
Interpretation:
- Diagnosis of an initial episode of ARF in any risk population
- Presence of 2 major criteria or 1 major and 2 minor criteria
- Diagnosis of a recurrent episode of ARF
- Requires 2 major criteria, 1 major and 2 minor criteria, or 3 minor criteria
- Diagnosis of possible ARF
- 1 major and 1 minor criteria with evidence of a preceding GAS infection
- A presumptive diagnosis of ARF without using Jones Criteria
- Patients presenting with Sydenham chorea or indolent carditis months after GAS infection
- Further investigation is indicated such as echocardiography
Laboratory investigations
- GAS detection
- Streptococcal antibody titer – best as anti-streptococcal antibodies usually reach a peak titer at the time of onset of ARF and are more useful for diagnosis
- Throat culture for group A β-hemolytic streptococci
- Rapid streptococcal tests
- Inflammatory markers such as CRP and ESR are elevated
- Other tests:
- Cardiac troponin – evaluate myocardial damage
- Rheumatoid factor – rule out rheumatoid arthritis
- Lyme serology – rule out Lyme disease
- Blood cultures – rule out septicemia
- Joint aspiration – rule out septic arthritis
Imaging investigations
- Echocardiography
- May reveal signs of valvulopathy or heart failure
- Electrocardiogram
- Sinus tachycardia
- First-degree atrioventricular (AV) block (prolongation of PR interval)
- Chest x-ray
- Cardiomegaly and pulmonary edema
Treatment
Supportive care
- Bed rest
Medical care
- Antibiotics
- If the patient weighs less than 27kg, penicillin V 250 mg 2 to 3 times daily for 10 days OR
- If the patient weighs more than 27kg, penicillin V 500 mg 2 to 3 times daily for 10 days OR
- A single intramuscular dose of penicillin G benzathine 600,000 units (if below 27 kg) or 1.2 million units (if above 27 kg) OR
- Amoxicillin dose is 50 mg/kg/d orally for 10 days, administered once or twice daily.
- Azithromycin at 12 mg/kg/d for 5 days with a maximum dose of 500 mg/dose
- Clarithromycin at 7.5 mg/kg/dose twice daily for 10 days with a maximum dose of 250 mg/dose
- Cephalosporins can be used as well
- Aspirin
- 60 to 100 mg/kg/day in divided doses until symptom resolution
- Used to manage arthritis
- Corticosteroids
- 1.0–2.0 mg/kg per day in divided doses should be continued until the ESR is normal and then tailed off
- Indicated in cases with carditis or severe arthritis.
- Treat heart failure as discussed in previous cheat sheet on heart failure management.
- Sydenham chorea
- Pharmacotherapy is recommended if symptoms are negatively impacting activities of daily life.
- Can use: carbamazepine, pimozide, haloperidol, and valproic acid
Secondary antibiotic prophylaxis
Patients with a history of ARF are at increased risk for disease recurrence and worsening RHD and should receive secondary antibiotic prophylaxis against GAS infections.
- Intramuscular penicillin G benzathine every 28 days (or every 21 days in high risk populations)
- Oral penicillin V twice daily can be used
- In event of penicillin allergy – sulfadiazines and macrolides
| Level of carditis | Duration of antimicrobial prophylaxis |
|---|---|
| Carditis and detectably persistent heart disease | 10 y from the last episode of ARF or until age 40 y, whichever is longer |
| Carditis without detectably persistent heart disease | 10 y from the last episode of ARF or until age 21 y, whichever is longer |
| No evidence of carditis | 5 y from the last episode of ARF or until age 21 y, whichever is longer |
Complications
- Rheumatic heart disease which can progress to:
- Heart failure
- Pulmonary hypertension
- Dysrhythmias
- Embolic strokes
- Sudden cardiac death
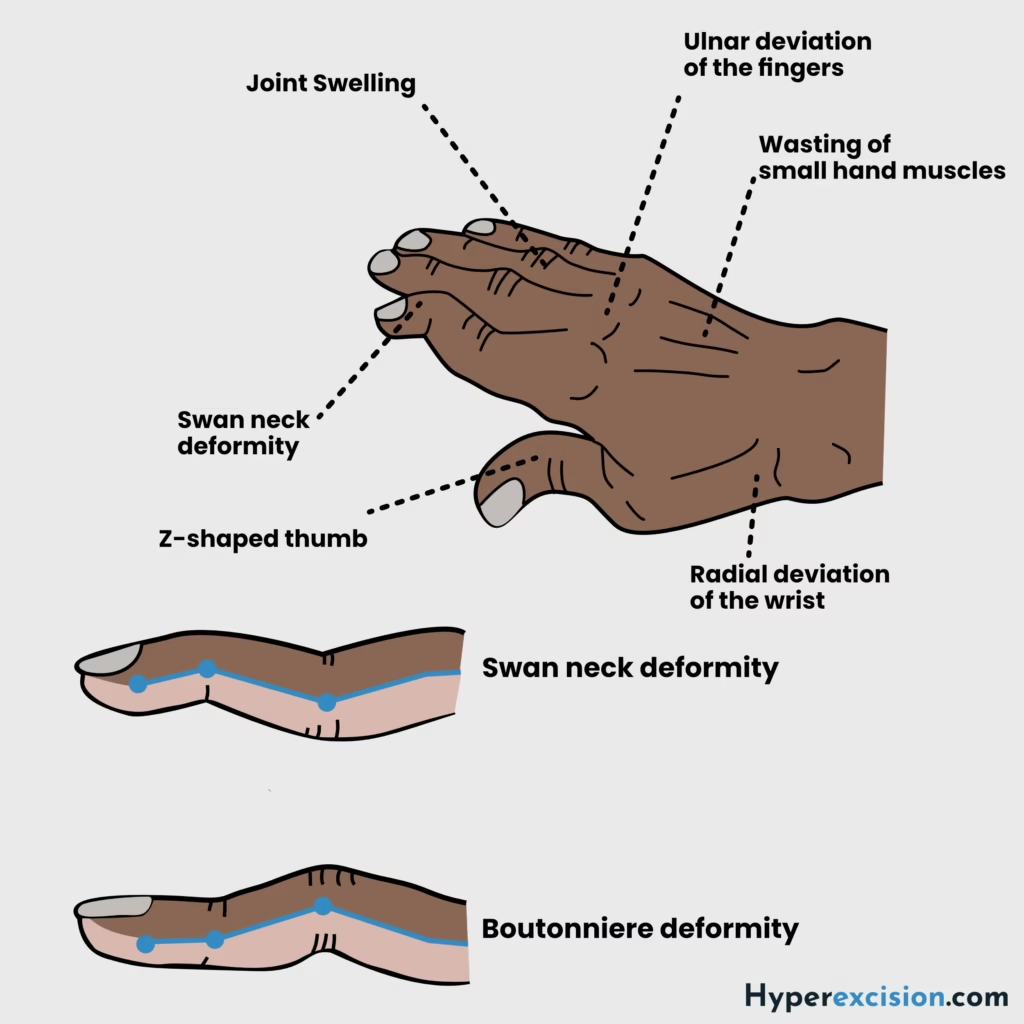
- Jaccuod arthropathy – chronic, benign arthropathy that may result in joint deformities due to repeated bouts of arthritis caused by ARF
- Syndenham chorea is related to increased psychiatric symptoms
- Chronic Rheumatic Heart Disease
- Develops in at least half of those affected by rheumatic fever with carditis.
- Two-thirds of cases occur in women.
- The main pathological process is progressive fibrosis causing valvular stenosis leading to hemodynamic disturbances