PCOS is a genetic, hormonal, metabolic, *and *reproductive disorder. It is the most common endocrine disorder of women in reproductive age. Etiology is unknown but there is a genetic component. Endocrine/hormonal disturbances lead to a constellation of sx. Sx vary among ethnicities but incidence does not. PCOS is a diagnosis of exclusion. 60-80% of reproductive age will present with hirsutism.
LH:FSH >2 is consistent with PCOS.
- Risk factors
- Genetic predisposition – Several susceptible genes have been identified as contributors. Twin studies suggest high risk of inheritability
- Obesity especially pre-pubertal obesity
- Early onset menarche
- Large/small for gestational age
- Insulin resistance
- Use of sodium valproate
- Fetal androgen exposure
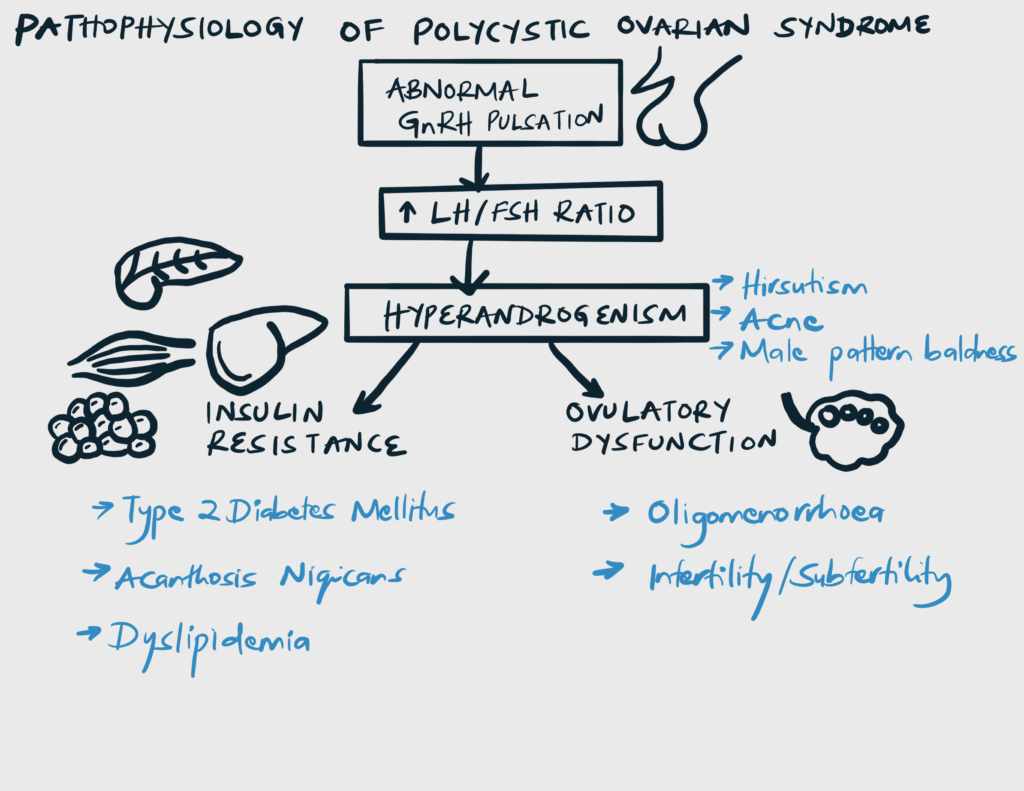
- Pathophysiology
- Gonadotropins
- Classic LH:FSH > 2:1 due disturbed GnRH pulsatility
- Insulin resistance
- Women with PCOS have insulin resistance
- Increased incidence of T2DM
- Androgens
- Insulin and LH stimulate andogen production by ovarian theca cells
- Estrone increases d/t peripheral aromatization
- SHBG
- Women with PCOS have lower SHBG.
- Adiponectin
- 60-80% of women with PCOS will be obese d/t low levels of adiponectin
- Gonadotropins
- Rotterdam criteria for PCOS (at least 2 of 3)
- Menstrual irregularities
- Oligomenorrhoea
- Amenorrhoea
- Hyperandrogenism
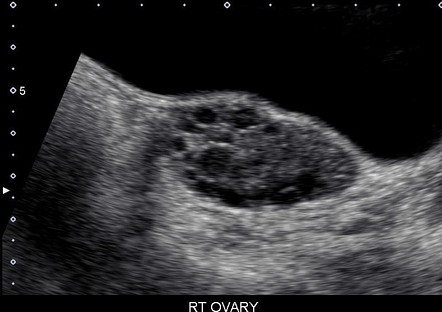
- Polycystic ovaries on ultrasound
- Menstrual irregularities
- Signs and symptoms
- Disturbed LH, FSH levels
- Oligomenorrhoea (Anovulation/Hypoovulation)
- Increased androgens
- Hirsutism (terminal hair on side-burns, upper lip, chin, belly, back – not same as hypertrichosis)
- Acne
- Male pattern balding
- Dyslipidemia
- Increased estrone/Low progesterone (Unopposed estrogen)
- Abnormal menstruation
- Insulin resistance
- Acanthosis nigricans
- T2DM (polyuria, polydipsia)
- Low adiponectin levels
- Obesity (BMI > 30)
- Disturbed LH, FSH levels
- Differentials for oligo-/anovulation
- Pregnancy
- Hyper-prolactinemia
- Use of dopamine antagonists
- Pituitary tumors
- Prolactin secreting tumors
- Hyperthyroidism
- Hypothyroidism
- Hypogonadotropic hypogonadism
- Premature Ovarian Failure (POF)
- Differentials for hyperandrogenism
- CAH (21-OHase deficiency, Frank virilization = “becoming a man”)
- Cushing’s syndrome
- Androgen-secreting tumor
- Exogenous androgens
- Investigations
- Urine or serum bHCG – rule out pregnancy as it can cause amenorrhea
- FSH
- LH
- TSH
- Prolactin
- Androgen levels
- Testosterone
- DHEA-S
-
- 17-OH progesterone
- To rule out non-classical congenital adrenal hyperplasia where it will be elevated
- Lipid proile
- Transvaginal sonography (TVS): to visualize ovaries
- Chain of pearl appearance
- 17-OH progesterone
- Treatment
- Combine oral contraceptives (COCs): cornerstone for medical management of PCOS
- Suppresses GnRH release → reduces androgens
- Progestin component of COCs → reduces endometrial proliferation (risk of endometrial ca)
- The progestin component also decreases LH levels, indirectly decreasing ovarian androgen production.
- Some progestins have been shown to have direct antiandrogenic properties as a direct inhibitor of 5 alpha-reductase activity to prevent the conversion of free testosterone to its more potent form, 5 alpha-dihydrotestosterone.
- Step 1: Induce withdrawal bleeding
- MPA 10mg PO qd for 10 days, or bid for 5 days
- Micronized progesterone 200mg PO qd for 10 days
- Step 2: Introduce oral contraceptives
- Ethinyestradiol/drospirenone (Yasmin)
- Ethinylestradiol/norgestimate
- Ethinylestradiol/desogestrel
- Alternative step 2: Cyclic progestins (will not get rid of hirsutism or acne)
- MPA
- Micronized progesterone
- Acne
- Topical retinoids (Tretinoin, Adapalene, Tazarotene)
- Topical benzoyl peroxide +/- topical antibiotics (Benzoyl peroxide/clindamycine, Benzoyl peroxide/erythromycine)
- Oral retinoids (Isotretinoin)
- Hirsutism
- Eflornithine topical
- Spirinolactone
- Cosmetic interventions such as bleaching, temporary removal
- Surgical removal
- Others
- Leuprolide (GnRH agonist)
- Metformin (for insulin resistance)
- Statins for dyslipidemia
- Metformin is also a second-line therapy for menstrual irregularities in patients with a contraindication for hormonal contraceptives. It is commonly used in adolescent monotherapy, and it helps restore normal menses and weight loss and reduce insulin resistance. Even though it should not be used primarily to treat clinical hyperandrogenism, it can mildly improve androgen excess symptoms.
- Combine oral contraceptives (COCs): cornerstone for medical management of PCOS
- Lifestyle modifications
- Exercise
- Calorie restrictive meals
- General medical complications
- Dyslipidemia (70%)
- Cardiovascular disease
- Endometrial neoplasia (RR 3X) – Long standing unopposed estrogen causes endometrial neoplasia
- Type 2 diabetes and impaired glucose regulation
- Obstructive sleep apnea (RR 30-40X)
- Non alcoholic fatty liver disease
- Anxiety and depression
- Obstetric complications
- Infertility/subfertility (d/t anovulation)
- Early miscarriage (30-50%)
- Gestational hypertension
- Gestational diabetes
- Preterm birth
- Perinatal mortality