Pelvic Inflammatory Disease
Pelvic inflammatory disease is a subacute to chronic infectious disease that affects the upper female reproductive tract (cervix, uterus, fallopian tubes, ovaries) and/or peritoneum. The most common causative organisms are C. trachomatis and Neisseria gonorrhoeae, but most cases can be polymicrobial (involving anaerobes hence empiric antibiotics should be broad-spectrum).
Infertility is a common complication of PID. Infections may spread into the peritoneum and involve peri-hepatic structures (Fitz-Hugh Curtis Syndrome – can be confused as gallbladder disease if there is RUQ pain). Diagnosis is clinical. Most patients are treated outpatient with antibiotics. The threshold for diagnosis of PID is low. Empiric antibiotics can be initiated at presentation if there is suspicion. Screening for lower genital tract chlamydial infection in young and high-risk individuals is recommended to reduce the incidence of PID, and asymptomatic disease in patients who return positive should be treated.
- Risk factors
- Multiple sex partners/ new sexual partner
- Age <25 years
- Unprotected sex
- History of STD (chlamydia, gonorrhea)
- Younger age at first intercourse
- Substance abuse
- Lower socioeconomic status
- Intrauterine contraceptive device (IUD) use
- Instrumentation of the uterus such as surgical termination of pregnancy
- Post-partum endometritis.
- Protective factors
- Barrier contraception
- Combined oral contraceptive pill
- Patient history
- Young woman of reproductive age
- Unprotected intercourse with multiple partners
- Signs and symptoms
- Lower abdominal pain
- Acute and constant
- Dull and crampy
- Usually non-severe
- Bilateral
- Associated with menstruation (begins a few days after menses)
- Mucopurulent vaginal discharge
- Deep dyspareunia
- Post-coital vaginal bleeding (inflammation makes tissue more friable)
- Fever
- Nausea and vomiting
- Irregular and/or more painful menses.
- Lower abdominal pain
- Physical examination
- Cervical motion tenderness
- Uterine tenderness
- Global uterine or adnexal tenderness (most sensitive finding)
- Mucopurulent discharge
- Erythematous inflammed cervix
- Fever +/- other systemic symptoms
- RUQ pain/ tenderness (Fitz-Hugh-Curtis syndrome)
- Rebound tenderness and guarding (in tubo-ovarian abscess or generalized peritonitis)
- Differentials
- Ectopic pregnancy
- Endometriosis
- Ovarian torsion
- Ovarian cysts
- Tubo-ovarian abscess
- Urinary tract infection
- Interstitial cystitis
- Appendicitis
- Clinical criteria for diagnosis
- Cervical motion tendernes or,
- Uterine tenderness, or
- Adnexal tenderness
- Investigations
- Qualitative B-hCG: rule out ectopic pregnancy
- Culture and microscopy of vaginal secretions
- Tests for gonorrhoea and chlamydia.
- Transvaginal sonography or CT-scan: to rule out tubo-ovarian abscess, particularly in more ill-appearing patients and those who do not respond to outpatient treatment
- Liver Function Tests: if there is RUQ pain
- Outpatient treatment
- IM Ceftriaxone 500mg single-dose + PO doxycycline 100mg q12h for 14 days
- May add PO Metronidazole 500mg q12 for 14 days (to target anaerobes)
- Azithromycin single-dose if allergic to cephalosporins
- Indications for inpatient treatment (IV antibiotics)
- Adolescent
- Cannot complete a course of oral antibiotics (including nausea or vomiting that precludes oral treatment)
- Failed outpatient treatment
- Pregnant patient
- Tubo-ovarian abscess (large abscesses will need to be drained)
- Severe disease (high fever, toxic appearing)
- Generalized peritonitis
- Drug abuse
- Recent intrauterine instrumentation
- WBCs > 15,000
- Inpatient treatment
- IV cefoxitin 2g q 6h + doxycycline 100mg q12 h
- Clindamycin or metronidazole for anaerobic coverage
- Transition to oral antibiotics and discharge 24-48 hours after clinical improvement with IV therapy
- If treatment fails perform imaging to rule out tubo-ovarian abscess
- Treatment of tubo-ovarian abscess
- IV antibiotics: abscess 4-6 cm can be managed with antibiotics alone
- Percutaneous drainage (especially for large abscess > 10 cm)
- Surgical drainage with salpingo-oophorectomy (rarely requires total hysterectomy with bilateral salpinho-oophorectomy)
- Indications for surgical drainage of a tubo-ovarian abscess
- Sepsis
- Drainage is unfeasable
- Patient fails antibiotics
- Rupture of abscess
- Complications of pelvic inflammatory disease
- Ectopic pregnancy
- Infertility
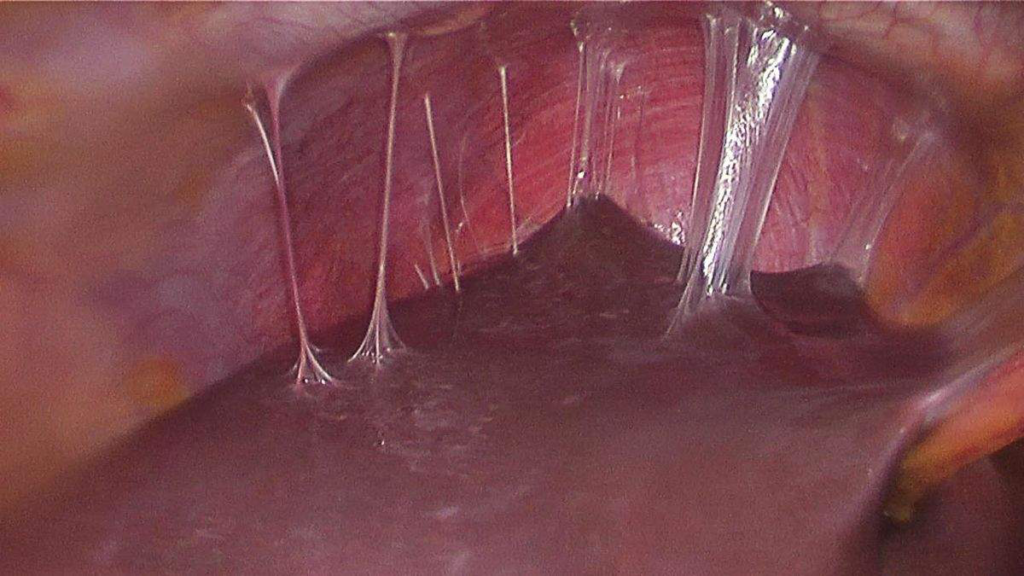
- Fitz-Hugh-Curtis syndrome
- Chronic pelvic pain
- Tubo-ovarian abscess.