Overview
For a woman to delivery vaginally they need to have a pelvis that is adequate in size and shape. The best indicator of an adequate pelvis is good progress during labour. Even so, the pelvis can be assessed for adequacy clinically using clinical pelvimetry, where 3 planes are assessed – the inlet, mid-pelvis and outlet.
The midpelvis has the smallest pelvic diameter (ischial spines – interspinous diameter and the largest pelvic dimension (sacral curve – AP diameter of the mid-pelvis).
Timing for clinical pelvimetry
| Category | Timing for clinical pelvimetry |
|---|---|
| Primigravida | Beyond 37 weeks |
| Multigravida | During labor |
Quick estimation of pelvic adequacy
| Measurment | Estimation |
|---|---|
| Diagnoal conjugate | Ability to touch the tip the sacral promontory |
| Inter-ischial diameter (transverse diameter of mid-pelvis) | Ability to touch the ischial promontory with two fingers simultaneously |
| Inter-tuberous diamter (transverse diameter of the outlet) | Ability to accomodate a fist between the ishcial tuberosities |
| Sub-pubic angle | Ability to place 2 fingers under the symphysis comfortably |
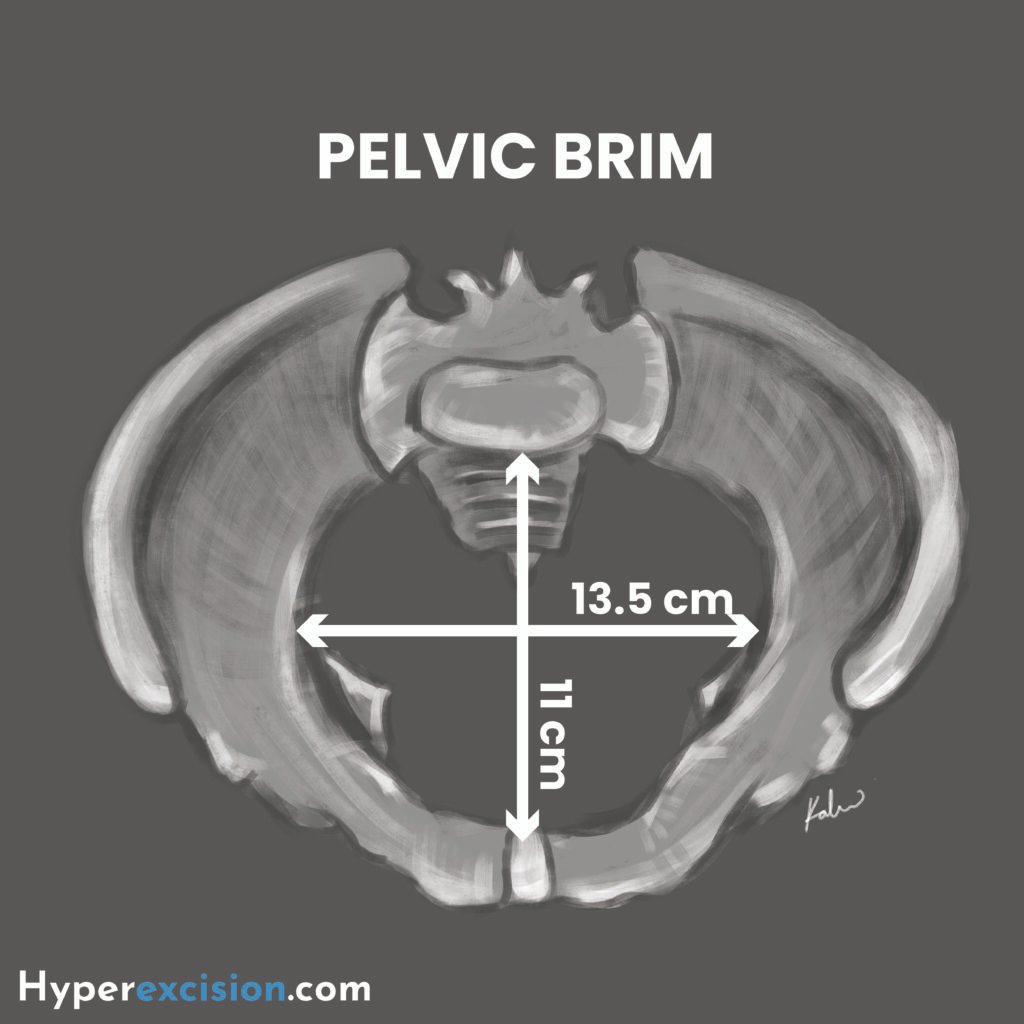
Pelvic Inlet
The pelvic inlet is also known as the pelvic brim. It is involved in fetal engagement. The fetal head enters the inlet in a trasnverse position since the transverse diameter of the inlet is wider than the anterior-posterio (AP) diameter.
Boundaries of the pelvic inlet
| Boundary | Structure |
|---|---|
| Anterior | Upper border of the pubic symphysis |
| Lateral | Upper margins of the pubic bone, iliopectineal line, and ala of sacrum |
| Posterior | Sacral promontory |
Measurements of the pelvic inlet
| Measurement | Estimation |
|---|---|
| AP diameter (11cm) | Reach the middle finger to the sacral promontory and measure the distance to the pubic symphysis (diagonal conjugate). Subtract 1.5 cm to get the obstetric conjugate |
| Transverse diameter (13.5 cm) | |
| Pelvic shape | Slide fingers along the pelvic brim to assess contour (gynaecoid vs android) |
| Retropubic angle | Palpate behind the pubic symphysis. Flat and narrow suggest non-gynaecoid pelvis |
Mid-pelvis
Mid-pelvis is also known as the mid-cavity. The transverse and AP diameter of the mid-pelvis are almost equal at 12 cm.
Boundaries of the mid-pelvis
| Boundary | Structure |
|---|---|
| Anterior | Middle of pubic symphysis |
| Lateral | Pubic bones, obturator fascia, and inner aspect of ischial bones and spine |
| Posterior | Junction of the sendon and third section of the sacrum |
Measurments of the mid pelvis
| Measurement | Estimation |
|---|---|
| Ischial spines | Palpate for prominence or bluntness |
| Lateral pelvic sidewalls | Run fingers along the sidewaal for diverging (gynecoid) or converging (android) side-walls |
| Sacral curve | Deep J-shaped sacral curve is favourable for internal rotation while a flat sacrum is unfavourable |
Pelvic Outlet
The pelvic outlet provides space for delivery. The AP diameter is widest at the outlet, which means that the fetal head must rotate from a transverse to an AP position as it passes through the mid-pelvis.
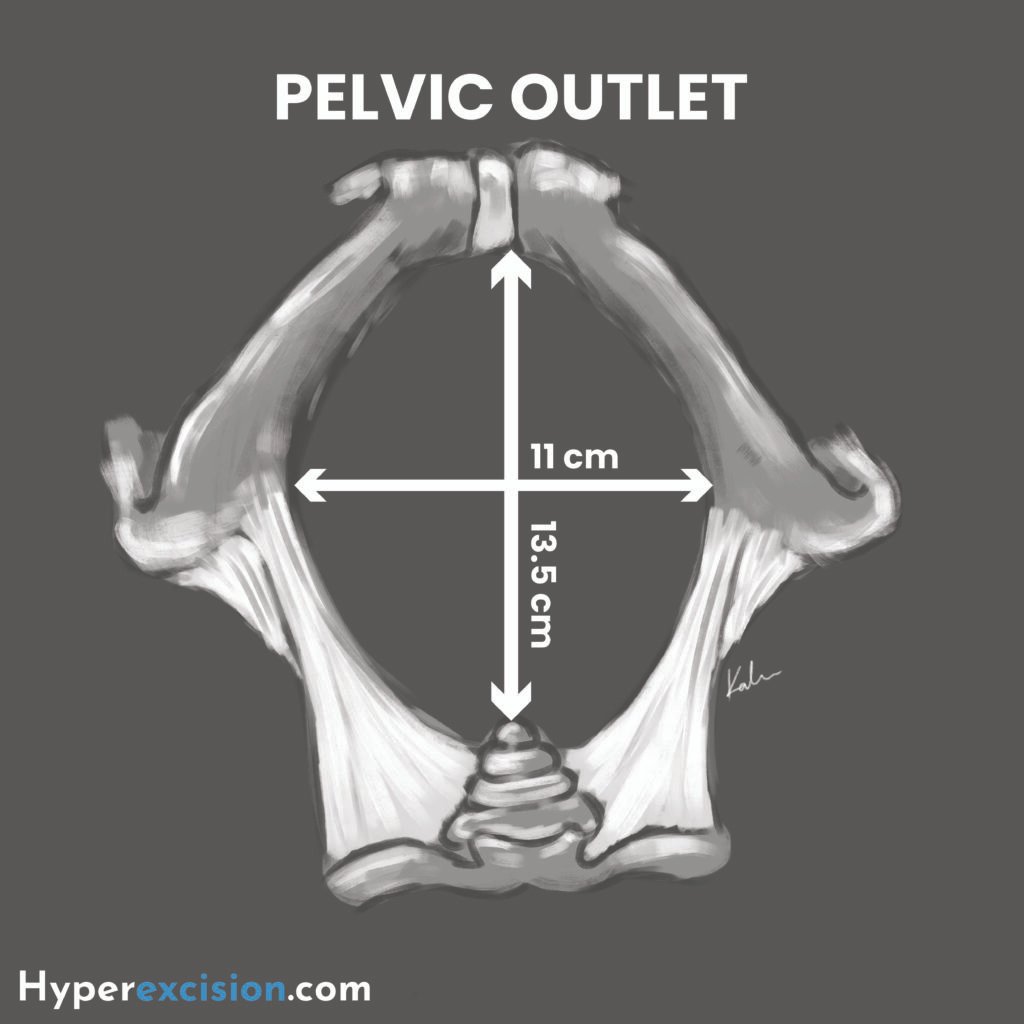
Boundaries of the pelvic outlet
| Boundary | Structure |
|---|---|
| Anterior | Lower margin of the symphysis pubis |
| Lateral | Inferior ramus of the pubis, ischial tuberosity, sacrotuberous ligament |
| Posterior | Distal sacrum |
Measurments of the pelvic outlet
| Measurement | Estimation |
|---|---|
| Sub-pubic angle | A wide angle of 90 – 100 is favourable |
| A-P diameter (13.5 cm) | Distance from the pubic symphysis to the lower body of the pubic symphysis |
| Interuberous diameter | Fit a closed fist between the ischial tuberosities of the perineum |
Contracted Pelvis
A contracted pelvis is rarely discovered in clincial practice. Anatomically, it is defined if any of its major diameters is shorted by 0.5 cm or more.
Thomas dictum: if sum of bispinous diameter and posterior sagittal diameter of the outlet is < 15 cm , then the pelvis is likely contracted
Diagnostic criteria
| Contracted pelvis | Definition |
|---|---|
| Contracted inlet | Obstetric conjugate < 10 cm; Diagonal conjugate < 11.5 cm |
| Contracted mid-pelvis | Inter-ischial diameter < 8 cm |
| Contracted outlet | Intertuberous diameter < 8 cm |
Grossly abnormal pelvic types
| Pelvis | Description |
|---|---|
| Rachitic pelvis | Pelvic deformity due to childhood rickets |
| Robert’s pelvis | Bilateral absence of pelvic alae |
| Naegele’s pelvis | Unilateral absence of a pelvic ala |
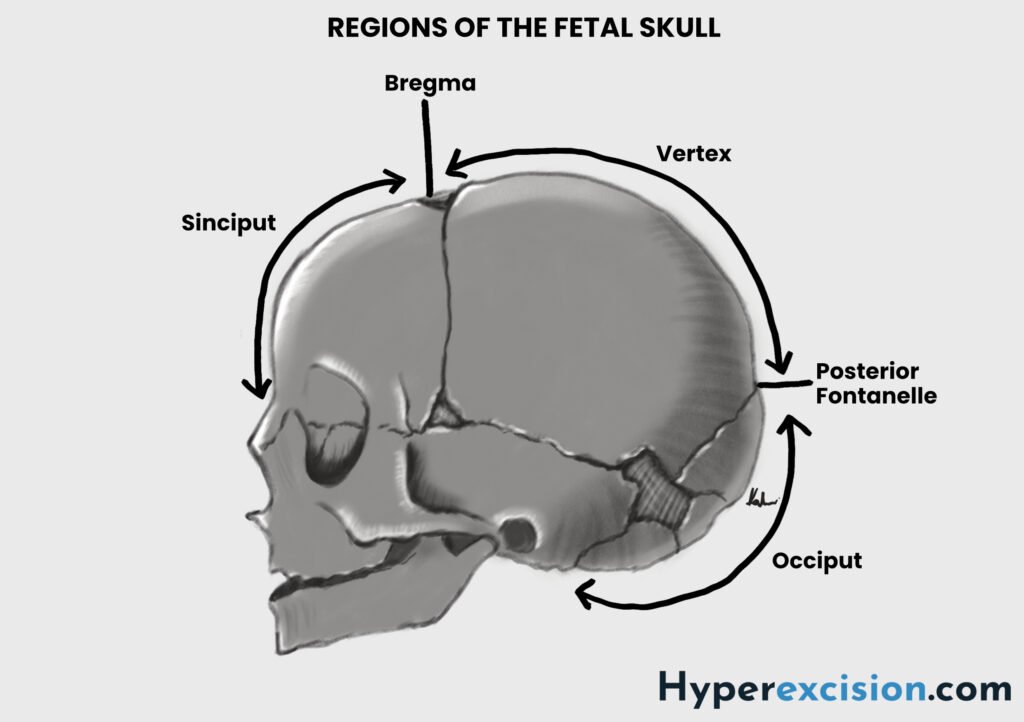
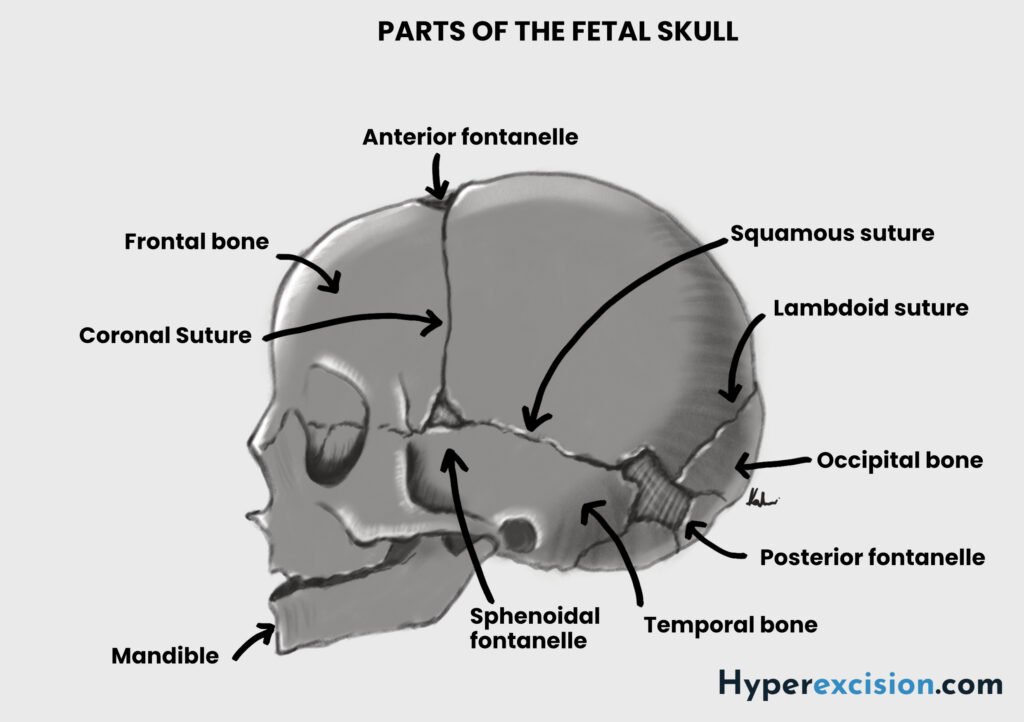
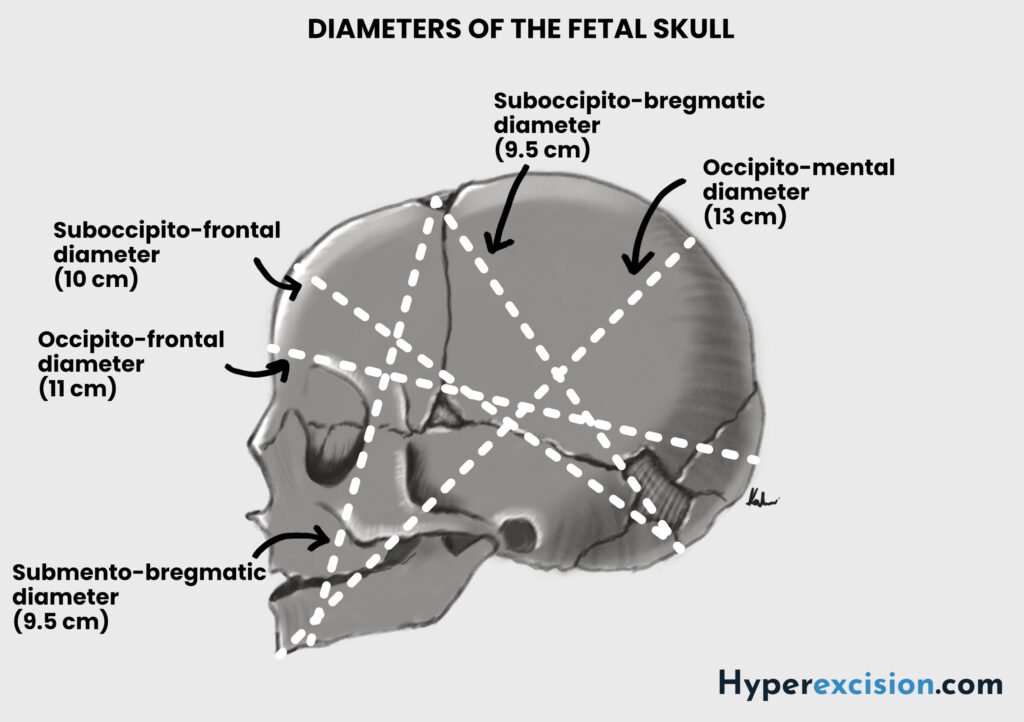
Diameters of the Fetal Skull
The fetal skull is ovoid in shape and is composed of sutures which allows the bones to move together and overlap. The parietal bones usually slide ever the frontal and occipital bone, a process known as moulding, which reduces the diameters of the fetal head and encourages progres through the pelvis while protecting the underlying brain. Severe moulding or moulding in early labour can be a sign of obstructed labour due to cephalopelvic disproportion or malposition (failure of the head to rotate).
Transverse diameters of the fetal skull
| Diameter | Measurement | Nota bene |
|---|---|---|
| Biparietal | 9.5. cm | Engagement occurs when biparietal diameter passes the pelvic inlet i.e. it is at 0 station. Moulding can reduce biparietal diameter slightly (~ 0.5 cm) as the parietal bones overlap |
| Bitemporal | 8 cm | Narrower than biparietal diameter |
| Bimastoid | 7.5 cm | Smallest transverse diameter |
Longitudinal diameters of the fetal skull
| Diameter | Measurment | Attitude | Nota bene |
|---|---|---|---|
| Suboccipito-bregmatic | 9.5 cm | Well flexed | Smallest presenting diameter in a fully flexed vertex presentation |
| Occipito-frontal | 11.5. cm | Deflexed (Military presentaiton) | Increased risk of obstructed labour |
| Mento-vertical | 13.0 cm | Extended (Brow-presentation) | Incompatible with pelvic inlet. Requires caesarean delivery |
| Submento-bregmatic | 9.5. cm | Hyperextended (Face-presentation) | Face-presentation can deliver vaginally when the chin is anterior (mento-anterior) since this is the smallest diameter. Most meto-posterior presentations convert to mentum anterior |
Cephalopelvic disporporion
Cephalopelvic disproportion occurs when the fetal head is too large to pass through the maternal pelvis due to a mismatch between fetal size and pelvic dimensions. It is usually diagnosed intrapartum when labour fails to progress despite adequate uterine contractions. It can lead to obstructed labour. Cephalopelvic disporpotion occurs either at the pelvic inlet or at the mid-cavity. Soft-tissues are involved once the the fetus enters the outlet.
- Causes of cephalopalvic disproportion
- Maternal-fetal size disproportion (relatively large baby to a relatively smaller mother)
- Macrosomia
- Hydrocephalus
- Contracted pelvis e.g. rickets, malnutrition
- Pelvic deformity from trauma
- Soft tissue abnormalities e.g. fibroids, mullerian anomalies
- Predisposing conditions: polio, tuberculosis, rickets, osteomyelitis, scoliosis
- Absolute signs of cephalopelvic disproportion
- Arrest of labour with adequate contractions
- Severe caput evidenced by grade III moulding
- Asynclitism characterized by lateral flexion of the fetal head and poor progress
- Obviously small pelvis and poor progress
- Overriding of fetal head over the pubic symphysis
- Relative signs of cephalopelvic disproportion
- Moderate caput or moulding
- Poor application of the fetal head against teh cervix
- High fetal head in the presence of a pelvis that is not obviously contracted
- Negative Munro-Kerr maneuver (fetal head appears fixed when attempts are made to push it up or down)
- Features that are suspicious for CPD at the level of the inlet
- Floating fetal head at term in primigravida (engagement should happen before labor in primigravida)
- Deflexed head (occipitoposterior or brow presentation)
- Methods for evaluating for CPD at the level of the inlet
- 2 fingers above the pubic symphysis and other hand on the head. Try to push the head down into the inlet.
- Muller-Munro-Kerr Method – 2 fingers at the ischial spines and one finger over the head at symphisis. Try to push the head into the inlet and feel the station at zero.
- Engagement of the head with CPD
- Head enters the pelvis with exaggerated asynclytism ( some “tilt” is normal)
- This is because the super-subparietal diameter (~ 8.5 cm) is smaller than the biparietal diameter
- Anterior asynclitism: common in multiparous women due to lax abdominal wall.
- Posterior asynclitism: common in primigravida
- Management of cephalopelvic disproportion
- Trial of labour for mild CPD at the level of inlet (if there is no other indication for caesarean delivery)
- Caesarean delivery for mid-pelvis CPD
- Complications of labor with contracted pelvis or CPD
- Malpresentation (Occipitoposterio position)
- Malposition (Transverse and oblique lies)
- Early rupture of membranes (deflexed head causes loose hanging bag of membranes which can rupture early)
- Increaed risk of cord prolapse
- Slow cervical dilatation (due to decreased stretch of the lower uterine segment – Ferguson reflex)
- Arrest of labor and prolonged labor (Deep transverse arrest – CPD at the level of the ischial spine or mid-pelvis)
- Arrest of dilatation
- Arrest of descent
- Increased need for operative delivery and maternal injury
- Fetal injury and asphyxia

