Overview
- Differentials for a pelvic mass
- Full bladder (urinary retention)
- Ovary
- Functional cyst
- Benign neoplasm
- Malignant neoplasm
- Endometrioma
- Metastatic ovarian tumor
- Uterus
- Pregnancy
- Fibroids
- Fallopian tube
- Tubo-ovarian abscess
- Ectopic pregnancy
- Fallopian tube carcinoma
- GIT
- Appendix abscess
- Diverticualr absces
- Colorectal Ca
| Benign mass | Malignant mass | |
|---|---|---|
| Size | < 8cm | > 8cm |
| Consistency | Cystic | Solid or mixed |
| Solid component | None | Nodular, Papilary |
| Sepatations | None or single | Multilocular, thick |
| Doppler | Negative | Positive |
| Laterality | Unilateral | Bilateral (50% of tumors) |
| Associated Fx | Calcification | Ascites, Peritoneal mets, LAN |
Guidelines for referring a pelvic mass for further workup
- Premenopausal (< 50 yoa)
- Ascites
- Evidence of abdominal or distant mets
- Elevated CA-125 level (> 200 U/mL)
- OVA1 score ≥ 5.0
- Postmenopausal (≥ 50 yoa)
- Ascites
- Evidence of abdominal or distant mets
- Nodular or fixed mass
- Elevated CA-125 level (> 200 U/mL)
- OVA1 score ≥ 4.4
Ovarian Cysts
Ovarian cysts consist of 75% of ovarian masses. They are cysts that arise in the ovary typically d/t normal ovarian stimulation (apart from theca lutein cysts which occur d/t excess hCG stimulation). Majority of cysts are functional. Pathophysiology of functional cysts depends on the type of cyst. Commonly asymptomatic and found incidentally on routine pelvic exam or on sonography. An ovarian mass in a post-menopausal woman is a major RED FLAG!
Cysts are very common. Most common in women of reproductive age. Diagnosis has increased over the past several years.
- Risk factors
- Smoking
- Progestin-only contraceptive (LNG-IUS – Mirena)
- Tamoxifen use
- Hx of previous cysts
- Signs and symptoms
- Lower abdominal pain
- Dull
- Vague
- Dyspareunia
- Urinary urgency
- Tenesmus
- Lower abdominal pain
- Investigations
- hCG level: r/o ectopic pregnancy
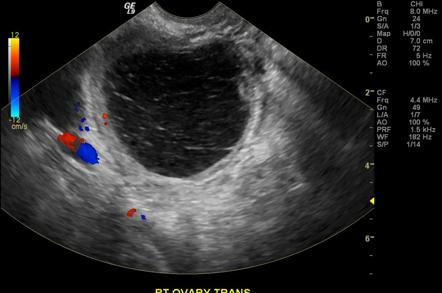
- Sonography (TAS or TVS):
- Thin walled
- Anechoid (filled with fluid)
- Echogenic material (clot in hemorrhagic cyst)
- Flow around margin of cysts in doppler (”Ring of fire” – corups luteum cyst)
- CBC: r/o infection
- UA: r/o UTI
- Endocervical swabs: r/o Gonorrhoea, Chlamydia (TOA, PID)
- CA-125 level: in older pts to r/o ovarian ca
- Treatment
- Asymptomatic cysts can be managed expectantly (no immediate intervention needed)
- F/u sonography in 6-8 weeks (expect regression)
- Laparoscopic evaluations
- Indications for laparoscopic evaluation
- Cyst > 7cm
- Pt taking COCs
- Complications
- Ovarian torsion: Hx of sharp, unilateral pain of sudden onset in lower abdomen. Accompanied by N/V, Fever
- Ovarian cyst rupture: Hx of sharp unilateral pain of sudden onset in lower abdomen. Accompanied by peritoneal sx, distension.
- How do COCs change the risk of functional ovarian cysts?
- Reduce
Follicular cysts
Follicular cysts occur d/t failure of the follicle to rupture at the culmination of the follicular stage (day 14) of the menstrual cycle. Fluid collects in the follicular antrum and expands. Size may vary from 3-8 cm. Classicaly asymptomatic.
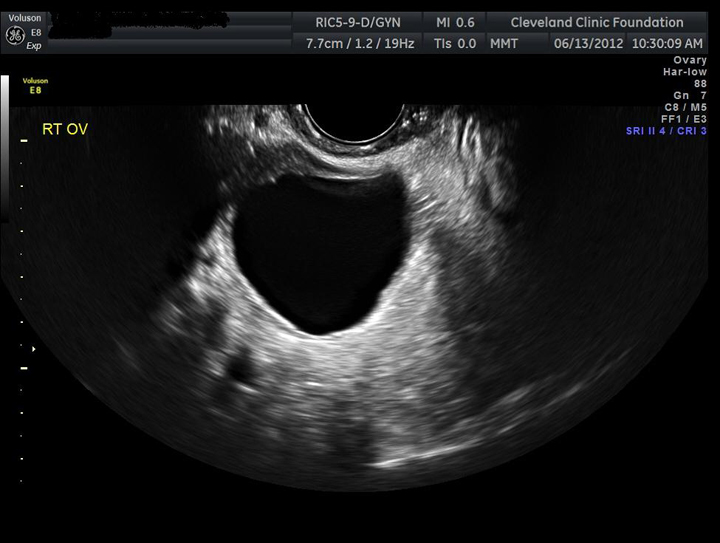

Corpus luteum cyst
Corups luteum cysts occurs when the corpus luteum fails to involute at the end of the luteal phase (day 28). Surrounding vessels at the antrum bleed into the persistent corpus lutuem. May rupture and bleed into the peritoneum.
- Signs and symptoms
- Delayed menstruation
- Dull lower quadrant pain
- Hypotension
- Peritoneal Sx
- Rebound tenderness
- Guarding
- Distension.
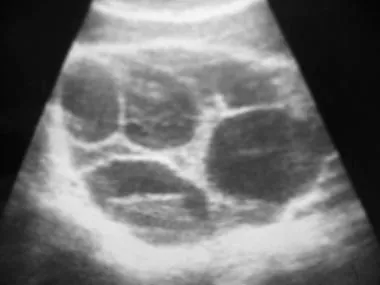
Theca lutein cyst
Theca lutein cysts are bilateral cysts caused by excess hCG stimulation of the theca interna. Often multiple cysts form multiple follicles.
- Associations Anything that increases hCG
- Chlomiphene for IVF
- Gestational trophoblastic disease
- Multiple gestation
- Diabetes mellitus
- Polycystic Ovarian Syndrome (PCOS)

Primary Ovarian neoplasms
Ovarian cancer is the 5th leading cause of cancer death in women. 9th leading cause of cancer in women. 1 in 70 women develop ovarian cancer in their lifetime. 1 in 95 will die from ovarian cancer. Average age at diagnosis is 61 years; 2/3 are > 55 yoa. Hereditary cancers occur earlier (BRA mutation). Higher incidence in whites. Germ cell tumors have a higher prevalence in black and asians.
| Tumor | Tumor marker |
|---|---|
| Epithelial | CA-125 |
| Dysgerminoma | LDH |
| Endodermal sinus tumor | AFP |
| Choriocarcinoma | hCG |
| Embryonal carcinoma* | AFP + hCG |
Staging ovarian cancer by surgical laparotomy
| Dx | 5-year survival | ||
|---|---|---|---|
| Stage I | Confined to ovaries | 28% | 92% |
| IA | 1 ovary | ||
| IB | 2 ovary | ||
| IC | 1/2 + Capsule rupture/Tumor at suface/Malignant ascites | ||
| Stage II | 1/2 ovaries + pelvic extension | 8% | 70% |
| IIA | Uterus/Tubes | ||
| IIB | Other pelvic organs | ||
| IIC | A/B with Malignant ascites | ||
| Stage III | 1/2 ovaries + Peritoneal Mets/Regional LNs | 50% | 39% |
| IIIA | Micro peritoneal mets | ||
| IIIB | Macro < 2cm peritoneal mets | ||
| IIIC | Macro > 2cm peritoneal mets/ regional LNs mets | ||
| Stage IV | Distant mets beyond peritoneal cavity | 13% | 17% |
- Signs and symptoms
- Asymptomatic until advanced
- Lower abdominal pain
- Vague
- Abdominal distension
- Bloating
- Early satiety
- Pelvic pressure
- Increased frequency and urgency (also common in menopause)
- “Sister Mary Joseph Nodule”
- Metastasis to umbilicus
- Sister Mary Joseph (1856-1939) noticed that a lot of patient w/ umbilical mass scheduled for surgery had poorer outcome
- Metastasis to umbilicus
- Meigs Syndrome
- Ovarian tumor
- Ascites
- Right hydrothorax (d/t to large diameter of right sided transdiaphragmatic lymphatic channels)
- Physical exam finding
- Solid, fixed, irregular pelvic mass
- Investigation
- Pelvic ultrasound (TAS or TVS)
- Multiple septations
- Cystic and solid components (papillary etc.)
- Larger than cysts (> 7cm)
- Neovascularization
- CA-125 titres: particularly in an older woman to r/o ovarian CT
- Abdominopelvic CT: for treatment planning
- Surgical laparotomy for staging and Tx
- Pelvic ultrasound (TAS or TVS)
- Treatment of ≤ Stage IB
- Surgical laparotomy
- Peritoneal washings or aspiration of free ascitic fluid
- Palpation of peritoneal surfaces
- Extrafascial hysterectomy and BSO (Unilateral SO can be done for young women w/cancer confined to one ovary)
- Peritoneal biopsy
- Pelvic and infrarenal para-aortic lymphadenectomy
- Surgical laparotomy
- Treatment of ≥ stage IC
- Chemotherapy: ≥ stage IC
- Carboplatin and Paclitaxel (Platinum based, 20% recurrence within 5 years)
- Bleomycin, Etoposide, Cisplatin (for stromal tumors in kids)
- Chemotherapy: ≥ stage IC
- Treatment of Ovarian cancer w/hydronephrosis
- Dialysis
- Nephrostomy tubes
- Follow-up treatment
- Regular pelvic exam for 5 years
- q3mos for 2 years
- then q4-6 mos for 3months
- then q1y thereafter.
- CA-125 titres at each visit
- Abdominopelvic CT ascites (or suspicion of recurrence)
- Regular pelvic exam for 5 years

Ovarian epithelial tumors (65-70%)
Derived from the ovarian surface epithelium. Slow growing and usually advanced at diagnosis. 65-70% of total ovarian tumors, but 90% of total ovarian cancers. Increased risk in women who carry a BRCA mutation. Most commonly diagnosed at stage IIIC.
Serous: Serous cystadenoma, Serous cystadenocarcinoma
Mucinous: Mucinous cystadenoma, Mucinous cystadenocarcinoma
Others: Endometriod carcinoma, Clear cell carcinoma, Brenner tumor
Ovarian germ cell tumor (15-20%)
Derived from cell destined to become eggs. Most common ovarian neoplasm in females < 20 yoa. Rapid growing and usually stage I at diagnosis. Less than 5% of total ovarian cancer.
Teratomas: Immature teratoma, Mature teratoma, Monodermal teratoma
Others: Dysgerminoma, Endodermal sinus tumor, Choriocarcinoma, Embryonal carcinoma, Polyembryoma
Sex-cord/Stromal tumors (5-10%)
Derived from hormone producing cells in the interstitium of the ovary. Variable age of onset. Hormone production may cause Sx not seen in other tumors. Make up less than 5% of total ovarian cancers.
Sex-cord/Stromal tumor: Granulosa-theca tumor, Sertoli-Leydig tumor, Fibroma

