Pelvic Floor Fistula (Overview)
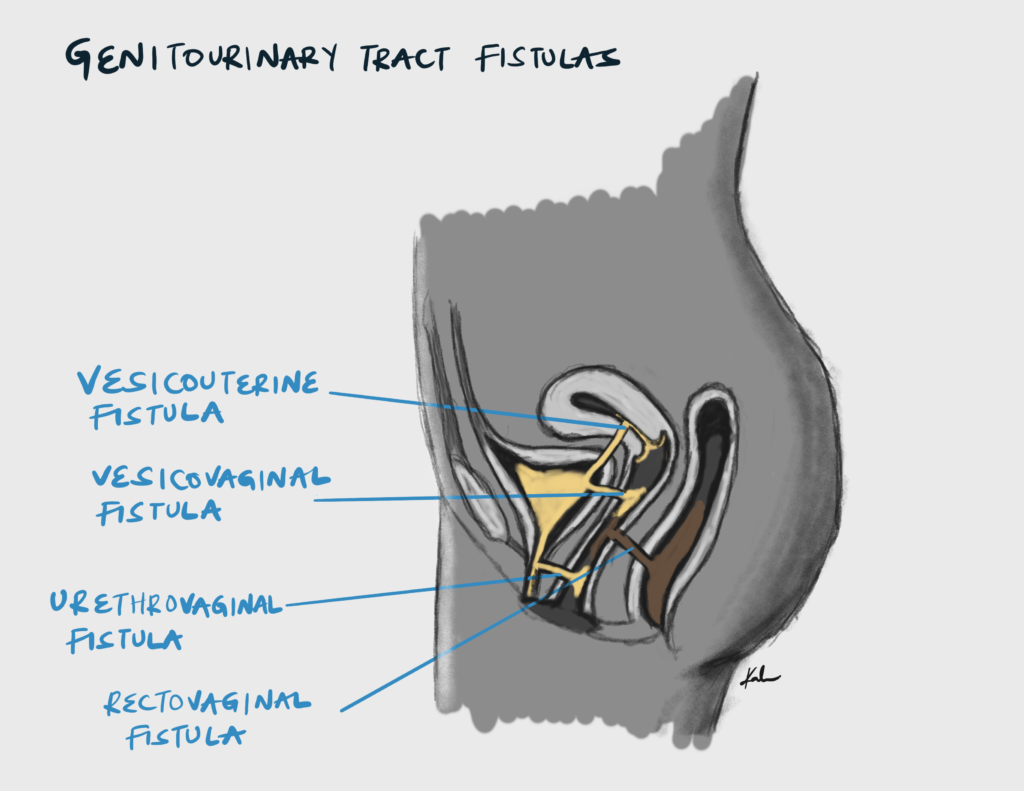
Pelvic floor fistulas are abnormal connections between two epithelialized surfaces within the pelvis. There are mainly two types, rectrovaginal fistula (RVF) and vesicovaginal fistula (VVF). Surgery is the primary treatment for fistula. Despite successful closure of fistulas, persistent urinary incontinence can result (15 – 55% of women suffer from persistent urinary incontinence after surgery)
The lifetime prevalence of vaginal fistulas is 3 per 1000 woment of reproductive age. Ethiopia has the larges number of women currently exhibiting symptoms of vaginal fistulas.
Causes of pelvic floor fistulas
| Classification | Causes |
|---|---|
| Congenital | Hypospadias (similar symptoms to fistula), ectopic ureter, cloacal perineal defect, imperforate anus with transcaginal rupture defect of the colorectal tract |
| Acquired causes | |
| Obstetric | Prolonged or obstructed labour, operative vaginal delivery complication e.g. midline episiotmy |
| Iatrogenic (as a complication of) | Caesarean delivery, uterine rupture repair, total abdominal hysterectomy, other pelvic surgeries |
| Traumatic | Pelvic crush or impalement, sexual violence-related, female genital mutilation |
| Inflammatory or Infectious | Crohn’s disease, tuberculosis, schistosomiasis, amoebiasis, lymphogranuloma |
| Cancer | Malignant disease in the pelvis, radiation therapy |
- Common causes of pelvic floor fistula
- Obstetric trauma
- Iatrogenic injury during surgery
- Radiation
- Inflammatory bowel disease e.g. Crohn’s disease
- Trauma
- Maignancy
Obstetric Fistula
An obstetric fistula is an abnormal opening between the woman’s genital tract and the urinary tract or rectum. It is commonly a result of neglected or prolonged obstructed labor. Constant pressure of the fetal head against pelvic organs causes tissue necrosis resultin in fistula.
67.6% of women with fistula-related symptoms encountered the problem soon after delivery (suggesting obstetric fistula).
- Risk factors for obstetric fistula The 3 delays
- First delay: delayed decision to seek care
- Low socio-economic status
- Early marriage
- Illiteracy and lack of formal education
- Low social status
- Harmful traditional practices e.g. FGM
- Inadequate family planning +/- short inter-delivery interval
- Labor onset at home
- Second delay: delayed arrival at the health facility
- Poor road conditions
- Poor transportation
- Poor communication
- Insecurity
- Third delay: delayed access to adequate care
- Insufficient skilled staff
- Lack of emergency obstetric services (e.g. C-section)
- First delay: delayed decision to seek care
- Causes of obstetric fistula
- Prolonged and Obstructed labour (MCC)
- Instrumental delivery
- Caesarean Section (with or without hysterectomy)
- Defibulation in women who have had FGM
- Symphysiotomy
- Episiotomy
- Types of obstetric fistula
- VesicovaginalVesiouterineVesicocervicalUreterouterineUreterocervicalUreterovaginalUrethrovaginalRectovaginal
- Patient history
- History of female genital mutilation
- History stillbirth, cephalopelvic disproportion or obstructed labour
- Operative vaginal delivery – episiotomy, symphysiotomy or destructive surgery
- Caeserean section
The obstetric labour injury complex
| Complication | Description |
|---|---|
| Fistula | Vesico-vaginal fistula, Urethrovaginal fistula, Recto-vaginal fistula, Ureteric fistula |
| Vaginal stenosis | Due to healing by fibrosis |
| Nerve damage | Foot drop and paraesthesia caused by compression of the lumbosacral plexus and peroneal nerve damage due to prolonged squatting |
| Dyspareunia | Due to vaginal scarring and stenosis |
| Damage to the cervix | Causing incompetence and stenosis which can lead to hematometra |
| Renal damage | Due to pyelonephritis and hydronephrosis caused by obstructing strictures and stones. Can ultimately lead to renal failure |
| Urine dermatitis | Urine phosphates and nitrates cause chronic excoriation of the vulva |
| Bladder stones | Women with obstetric fistula tend to reduce water intake or insert clothes in the vagina. these practices promote stone formation |
| Socio-economic consequences | Depression, divorce or separation, malnutrition, ostracization |
- Pathogenesis of obstetric fistula in obstructed labor
- During obstructed labour there is prolonged pressure exerted on the anterior vaginal wall and bladder neck by the foetal head and posterior pubic symphysis
- This causes ischemia and reduced venous outlfow ultimately causing pressure necrosis
- After delivery the necrotic tissue sloughs off leaving a direct communication between the genital tract (uterus, cervix, vagina) and the urinary tract (ureters, bladder, urethra), and/or the rectum.
- Ischemia can also involve other pelvic tissue resulting in a spectrum of injuries known as the obstetric labour injury complex
Waaldijik Classification of Vesico-vaginal fistula (VVF)
| Classification | Description | |
|---|---|---|
| Type I | Simple VVF | Fistula ≥ 5 cm from the external urethral opening and < 4cm in size (small). Does not involve the closing mechanism. Has excellent prognosis since the urethra and bladder neck are intact |
| Type II | Complex VVF with urethral involvement | Fistula involving the closing mechanism (< 5 cm from the external urethral orifice) |
| Type II A | Without (sub)total involvement of the urethra | |
| Type II A (a) | Without a circumferential defect | |
| Type II A (b) | With a circumferential defect | |
| Type II B | With sub(total) involvement of the urethra | |
| Type II B (a) | Without a circumferential defect | |
| Type II B (b) | With a circumferential defect | |
| Type III | Ureterovaginal and Urethro vaginal fistula | |
| Type IV | Rectovaginal fistula |
NOTE:
- Circumferential defect = complete separation of the urethra from the bladder.
- Note there are other classification systems such as Goh’s system.
Clinical Features
- Signs and symptoms of vesicovaginal fistula (VVF)
- Urinary incontinence
- With movement
- Constant leakage
- Irritation dermatitis (from crystallization of urin on the vulva, buttocks, thighs, legs and dorsal feet). May be with or without ulceration
- Cyclical hematuria (Youssef’s syndrome/triad)
- Menouria: menstrual-like cyclical bleeding via the urinary tract
- Amenorrhoea: absence of menstrual bleeding from teh uterus (40% of women with fistula have amenorrhoea commonly due to nutritional issues or asherman syndrome, or stenosis of internal cervical os)
- Urinary incontinence
- Urinary incontinence
- Signs and symptoms of rectovaginal fistula (RVF)
- Fecal and flatus incontinence
- “Bubbles” or frank fetal material in the vagina
- Signs and symptoms
- Urinary incontinence
- Constant leak
- Not dependent on activity
- Onset directly after labour and delivery
- Fecal incontinence
- Other problems with mobility and walking
- Urinary incontinence
Evaluation
- Patient history
- Onset, duration, frequncy and severity of urinary or fecal incontinence
- Vaginal discharge, odor, infections, pain or sexual dysfunction
- Previous treatments or interventions for the fistula or related conditions e.g. antibiotics, anti-inflammatories, hormones, catheters, pessaries, surgery
- How the condition impacts the patient’s life
- Physical examination
- Inspection of external genitalia and perineum (signs of incontinence, wet perineum, skin inflammation and ulceration, scarring or prolapse)
- Digital examination to palpate fistula defect
- Speculum examination for signs of fistula opnings, discharge, bleeding or massess
- Bimanual examination for signs of enlargment, tenderness, mobility and massess
- Digital rectal examination for fistula openings, sphincter tone, fecal impaction or massess (place a tampon in the vagina to prevent cross contamination)
- Neurological examination of pelvic floor muscles and nerves for signs of weakness spasms, reflexes or sensation
- Investigations
- Double dye test: pack the vagina with sterile gauze and give methylene blue dye intravesical via foley catheter and through oral route for pyridium
- Instillation of methylene blue into the bladder: identifies vesicovaginal fistula
- Methyleneblue crosses from the bladder and into the vagina staining the gauze blue
- PO Phenazopydidine (Pyridium): identifies ureterovaginal fistula. 10% of VVFs have ureteral involvement
- Pyridium crosses the uterus into the vagina staining the tampon orange
- Instillation of methylene blue into the bladder: identifies vesicovaginal fistula
- 3 swab test: pack the vagina with 3 separate gauzes and fill the bladder with methylene blue die
- Vesicovaginal fistula: discoloration of the uppermost swab
- Urethrovaginal fistula: discoloration of the bottom-most swab
- CT KUBor IV pyelographyCystoscopyRetrograde pyelogram
- Retrograde pyelography is the most definitive test to diagnose a ureterovaginal fistula
- Urinalysis and culture: to rule out concurrent UTI
- U/E/C: evaluate kidney function
- Double dye test: pack the vagina with sterile gauze and give methylene blue dye intravesical via foley catheter and through oral route for pyridium
- Complications of pelvic floor fistuals
- Infection
Management
Surgical repair of pelvic floor fistula is primarily performed by specialized fistula surgerons.
- Pre-operative consideration for obstetric fistula
- Delay fistula repair for 3 months post-injury to allow sloughing of necrotic tissue and complete healing of surrounding tissues
- Small fistulas < 2 cm in mid-vagina exhibit a high likelihood of spontaneous colsure
- Early placement of foley catheter increaes the probability of spontaneous closure of small fistulas within days to weeks after injury by diverting urine away from the fistula tract. This can be left in place for 10-14 days in at risk women
- Prevention
- Educate communities on the cultural, social and physiological factors that increase the incidence of obstetric fistulas such a delaying child bearing and improving nutrition.
- Improve the social status of women by promoting education for young girls.
- Ensuring their is easy access to health facilities which are well equipped and staffed with professionals.
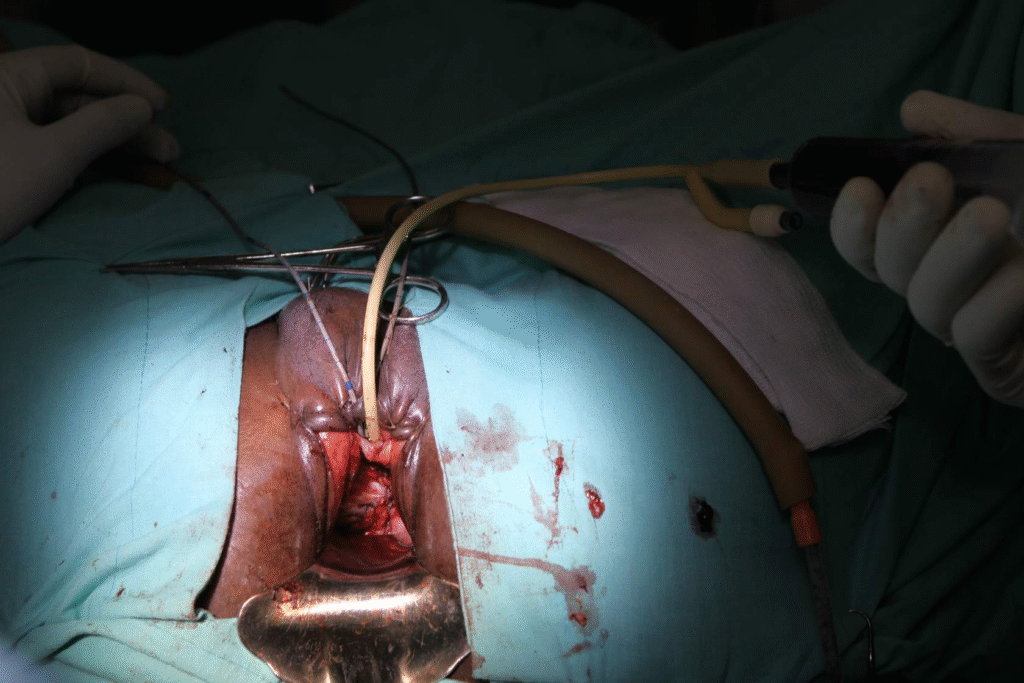
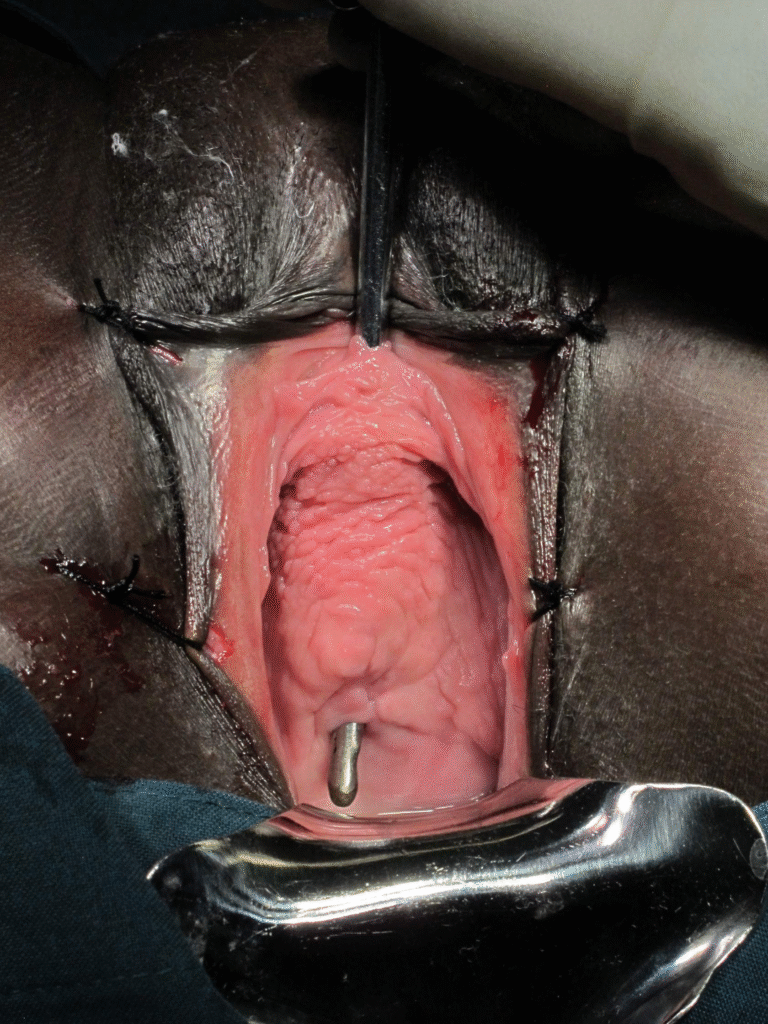
Gallery