- Presenting Complaints
- Overview of Physical Examination
- Mental Status Examination (Higher Functions)
- Cranial Nerve Examination
- Olfactory Nerve (CN I)
- Vision (CN II)
- Eye Movements (CN III, IV and VI)
- Facial Sensation and Muscles of Mastication (CN V)
- Facial Expression (CN VII)
- Hearing (CN VIII)
- Vestibular Function (CN VIII)
- Palatal movement (CN IX and X) and Dysarthria (CN IX, X, and XII)
- Head Rotation and Shoulder Elevation (CN XI)
- Tongue movements (CN XII)
- Examination of the Limbs
- Meningism
- Demonstrations
- Demonstrations
Presenting Complaints
- Headache
- SOCRATES
- Is it different from usualy headaches? (A “worst-ever”headache should be taken very seriously…)
- Acute or chronic?
- Onset? (sudden or gradual)
- Unilateral or bilateral?
- Associated symptoms? (Aura in migraines, Neck stiffness?)
- Worse on waking? (raised ICP)
- Decreased consciosuness?
- Muscle weakness
- Onset?
- Muscle groups affected?
- Associated loss of sensation?
- Associated shooting pain?
- Associated urinary or fecal incontinence?
- Associated loss of balance?
- Visual disturbance (blurring, diplopia, photophobia, vision loss)
- Speed of onset?
- Preceding symptoms?
- Eye pain?
- Dizziness
- Illusions of surroundings moving? (verigo)
- Hearing loss/tinnitus?
- Loss of consciousness?
- Does it occur with change in position?
- Speech disturbance
- Difficulty in expression, articulation or comprehension?
- Onset?
- Dysphagia
- To solids and/or liquids?
- Intermittent or constant?
- Associated pain? (odynophagia)
- Associated difficuly in coordination?
- Convulsions/Involuntary movements
- Frequency?
- Duration?
- Onset?
- Preceding aura? (pre-ictal)
- Was there loss of consciousness?
- Was there tongue biting?
- Was there incontinence?
- Was there residual weakness/confusion post-ictal?
- Is there a family history?
- Abnormal sensation
- “Pins and needles”? (Paraesthesiae)
- Pain?
- Odd sensation?
- Over which part of the body? (Distribution)
- Onset?
- Associated weakness?
- Tremor
- Rapid or slow?
- Is it present at rest?
- Is it worse on deliberate movement?
- Is the patient taking B-agonists?
- Does the patient have thyroid problems? (neck swelling, palpitations, sweating, unintentional weight loss e.t.c.)
- Is there a family History?
- Associated fasciculations?
- Trauma risk factors
- Did the patient ****hit their head?
- Raised intracranial pressure signs and symptoms
- Early morning projectile vomiting?
- Headache that gets worse in the morning, or on moving up and down?
- Tinnitus
- Meningism
- Fever
- Photophobia
- Neck stiffness
- Rash
- Giant cell arteritis signs and symptoms
- Pain in temporal region?
- Jaw claudication?
- Pain on swallowing?
- Blurred vision?
- Senses
- Change in smell, taste, or hearing? (consider an ENT diseae)
Overview of Physical Examination
The following questions should be answered when performing a neurological examination:
- Is the neurological problem primary or secondary?
- Does the neurological disorder affect the CNS, PNS or both?
- Which specific parts of the CNS and/or PNS is involved?
Note that specific examination exist form many neurological conditions including stroke, neuro-oncology, multiple sclerosis, ataxia e.t.c. This is out of scope but these can be used to examine their respective patient populations as appropriate
Mental Status Examination (Higher Functions)
Assessment of the mental status notes deficits in level of consciousness (arousal), attention and concentration, memory (immediate, recent, and remote), language, speech, visual (spatial perception), executive functioning, mood and thought content, praxis (ability to generate voluntary motor activity) and calculations
GCS Score
Vision (4 eyes)
| Eye opening | Score |
|---|---|
| Spontaneously | 4 |
| To verbal command | 3 |
| To pain | 2 |
| No response | 1 |
| Not testable | NT |
Motor response (Inline 6)
| Motor response | Score |
|---|---|
| Obeys command | 6 |
| Localizes to pain | 5 |
| Flexion withdrawal | 4 |
| Abnormal flexion (decorticate) | 3 |
| Abnormal extension (decerebrate) | 2 |
| No response | 1 |
| Not testable | NT |
Verbal response (Jackson 5)
| Verbal response | Score |
|---|---|
| Oriented and converses | 5 |
| Disoriented and converses | 4 |
| Inappropriate words | 3 |
| Incomprehensible sounds | 2 |
| No response | 1 |
| Not testable | NT |
Abbreviated Mental Test Score (AMTS)
Each question is 1 point. A score < 6 is significant for dementia or delirium
- How old are you?
- What time is it? (to the nearest hour)
- What Year is it?
- Where are we?
- I want you to remember this address: 42 West Register Street. Ask to recall later on in test
- Do you know who I am? Do you know who that is [point to nurse/family member]
- Do you know who the president is?
- What is your date of birth?
- Can you tell me when [a memorable date] happened?
- Can you count down from 20 to 1?
Mini Mental State Exam (MMSE)
The MMSE is marked out of 30 and is used to assess cognitive impairment (screening tool for dementia, especially Alzheimer’s)
| Score | Interpretation |
|---|---|
| ≥ 25 | Normal |
| 21 – 24 | Mild impairment |
| 10 – 20 | Moderate impairment |
| < 10 | Severe impairment |
- Orientation to time (5)
- Ask for the year? month? day of the week? time?
- Orientation to place (5)
- Ask for the continent? country? county? hospital? floor/ward?
- Registration (3)
- Name three unrelated objects clearly and slowly, then ask the patient to name all of them. Repeat until patient learn them all and note the number of trials.
- Attention and calculation (5)
- Count backwards from 100 by sevens (stop after five answers at 65)
- Alternatively, spell WORLD backwards (D-L-R-O-W)
- Recall (3)
- Recall the three objects mentioned before
- Language and praxis (2 + 1 + 3 + 1+ 1 + 1 = 9)
- Show the patient 2 simple objects (wristwatch, pencil, and ask them to name them) – 2 points
- “Repeat the phrase “No ifs, ands or buts.” – 1 point
- “Take the paper in your right hand, fold it in half, and put it on the floor.” – 3 points
- “Please read this and do what it says” (Written instruction says “close your eyes) – 1 point
- “Make up and write a sentence about anything.” (Must contain a noun and a verb) – 1 point
- “Please draw this picture” (A picture of 2 intersecting pentagons, all 10 angles must be present and the pentagons should intersect) – 1 point
- Interpretation
- Severity
- 25 = normal
- 24-30 = no cognitive impairment
- 18-23 = mild cognitive impairment
- 0-17 = severe cognitive impairment
- Single Cutoff
- <24 = abnormal
- Range
- <21 = increase odds of dementia
- 25 = decreased odds of dementia
- Education
- 21 = abnormal for 8th grade
- <23 = abnormal for high school education
- <24 = abnormal for college education
- Severity
Cranial Nerve Examination
Olfactory Nerve (CN I)
Ask the patient if they notice smells in the morning (bread, tea, eggs), smells that others do, or if they think their sense of smell is poor. Also ask if they have a blocked nose to save further testing. Also ask for taste as taste is likely to be impaired is smell is impaired.
- Clinical method
- Test one nostril at a time using common scents e.g. soap, spice, or food.
- Don’s use noxious smells like alcohol swab or ammonia
- If there are any defects, look in the nostril for polyps, foreign bodies, or infection
Vision (CN II)
- Basic questions
- Glasses or contact lenses?
- Any other problems with vision?
- Inspection
- Inspect for swelling, erythema, ptosis e.t.c.
Visual acuity
- Clinical method
- Place a hand-held visual acuity card about 30 cm from the patient’s right eye while the left eye is covered. The patient should wear their standard corrective lenses
- Start with the lowest line (20/20) and move up until you reach a line where most items are read correctly
- Repeat for the left eye
Visual fields
- Visual inattention: tests the extremities of the visual fields with both eyes open
- Visual field defects: tests the four quadrants for each eye separately (cover your opposite eye to compare you visual fields)
- Assess the size of the blind spot
Pupillary light reflex
Shining a light should constrict both pupils simultaneously
| Sign | Nota bene |
|---|---|
| Miosis | Iatrogenic (pilocarpine), Horner’s or Holmes-Adie pupil (unilateral), Opiate overdose or stroke or bilateral Horner’s (Bilateral) |
| Mydriasis | Iatrogenic (Tropicamide), fear or anger, stroke, anticholinergic overdose |
| Fixed oval pupil | Glaucoma |
| Grossly irregular pupil | Adhesions secondary to iritis |
| Relative afferent pupillary defect (Marcus-Gunn pupil) | Multiple sclerosis, massive retinal detachment |
| Horner’s syndrome | Normal light response, ipsilateral ptosis and miosis |
| CN III palsy | Down and out eyes, mydriasis not responding to direct or afferent light |
Accommodation reflex
| Sign | Possible causes |
|---|---|
| Argyll-Robertson Pupils | Diabetes Mellitus, Syphilis |
Fundoscopic exam
| Sign | Possible causes |
|---|---|
| Papilloedema | Raised ICP (do not do Lumbar puncture), mass lesion, malignant hypertension, multiple sclerosis |
| Optic atrophy | abnormally pale, small disc |
| Cupping | Glaucoma, ischaemia of the optic nerve |
| Inspection of the vessels | Normal arc? Tortuous? Hemorrhage |
| Inspection of the retina | Cotton wool spots? Exudates? |
Diabetic eye changes on fundoscopy
| Classification | Features |
|---|---|
| Background retinopathy | Hard exudates, Dot hemorrhages |
| Proliferative retinopathy | Scarring (photo-coagulation scars), Neovascularization |
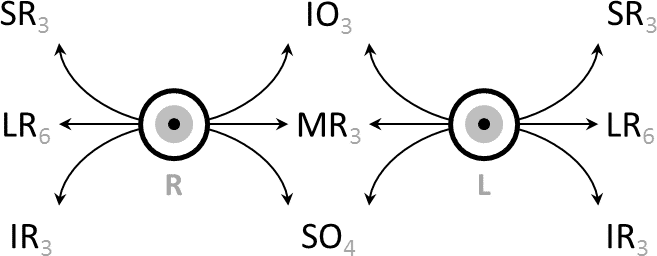
Eye Movements (CN III, IV and VI)
- Clinical method (CN III, IV and VI)
- Ask the patient if they have ever experienced double vision
- Ask the patient to follow your finger in a H pattern to test eye movements
- Make sure they avoid moving their head and watch for smoothness and range of their eye movements.
- Observe for nystagmus by keeping your fingers at the far right or left
- Clinical method for abducens nerve (CN VI)
- Ask the patient if they have ever experienced double vision
- Ask the patient to look directly far to the left and directly far to the right
- Abducens palsy: Trouble looking laterally (Abducting the eyes)
- Clinical method for trochlear nerve (CN IV)
- Ask the patient if they have ever experience double vision
- Ask the patient to look directly downwards, far to the left and far to the right
- CN IV palsies are subtle and hard to detect. They often presents with other palsies
Facial Sensation and Muscles of Mastication (CN V)
- Sensory function
- Touch on forehead: Ophthalmic region
- Touch on cheek bone: Maxillary region
- Touch on chin or lateral to mouth: Mandibular region
- Motor function
- Clench jaw: feel temporalis and masseter contracting
- Open jaw against resistance and close jaw against resistance
- Move jaw from side to side: tests the pterygoids
- Jaw jerk reflex
- Power – assess ****if you notice signs of wasting
- Corneal reflex (CN V and CN VII)
- The patient should close their eyes when their cornea is touched with a cotton wool
- Tests the ophthalmic branch of CN V (afferent) and zygomatic branch of CN VII (efferent)
Facial Expression (CN VII)
- Inspection
- Facial symmetry. If there is asymmetry, the mouth deviateds towards the affected nerve
- Nasolabial folds
- Frontal creases
- Raised eyebrows
- Clinical method
- Frown or lift eyebrows: Temporal nerve
- Close eyes tightly: Orbicularis Occuli muscles
- Smile with lips closes
- Smile while showing teeth
- Blow out cheeks, then check that air does not come out when you apply pressure to the cheeks
- Test Chorda Tympani branch
- Dry the patients tongue and apply sucrose on the tips and sides. Ask if they taste it before and after returning their tongue inside their mouth
- Test for sweet, sour, bitter, and salty gustation
- Test deep petrosal nerve
- Ask the patient if they have dry mouth or dry eyes
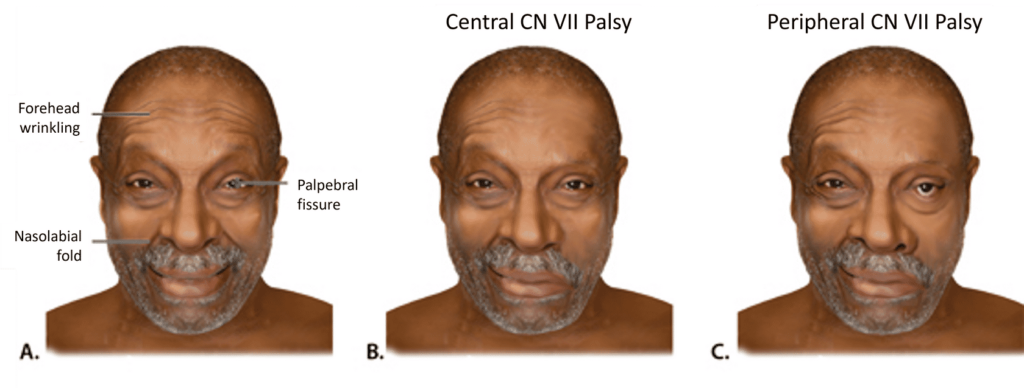
Hearing (CN VIII)
- Clinical method
- Whisper to the patient’s ears and ask them to repeat (hold your hand up as a sound screen and ask them to repeat a few numbers while rhythmically tapping the opposite ear to keep it from contributing)
- Alternatively you can hold your fingers a few centimetres from their ear and rub them softly together
- Perform Weber’s and Rinne’s test. Pluck the tuning fork or hit it on your hand.
- Rinne’s test
- Rinne’s positive: Sensorineural Deafness
- Rinne’s negative: Conduction Deafness
- Weber’s test
- Centralized weber: No hearing loss, bilateral conductive hearing loss, bilateral sensorineural hearing loss
- Lateralized weber: Ipsilateral conductive hearing loss, Contralateral Sensorineural hearing loss
Vestibular Function (CN VIII)
Peripheral vestibular function can be assessed by observing the patient’s gait and balance as well as the appearance of spontaneous and/or elicited nystagmus
Palatal movement (CN IX and X) and Dysarthria (CN IX, X, and XII)
- Clinical method (CN IX)
- Ask the patient if they have a dry mouth: Parotids are innervated by the Glossopharyngeal nerve
- Test taste on the posterior 1/3 of the tongue: same procedure as that for testing the Chorda Tympani
- Test gag reflex: Put a spatula on the lateral side of the pharynx
- Clinical method (motor)
- Ask the patient to say “Ahhhh” and observe whether the two sides of the palate move fully and symmetrically
- Clinical method (swallowing)
- Ask the patient to swallow water if available
- Clinical method (speech)
- Ask the patient to repeat a sentence
- Nasal sound: Vagus nerve defect as the soft palate cannot be raised, thus sound waves are transmitted through the nasal cavity
Head Rotation and Shoulder Elevation (CN XI)
- Clinical method
- Rotate head against resistance: SCM. Remember to palpate the SCM
- Raise shoulders against resistance: Trapezius
Tongue movements (CN XII)
- Clinical method
- Power: push the tongue against the left and right cheek while you push against it from outside
- Deviation of the tongue while protruded: the tongue deviates to the weaker side
- Ipsilateral deviation in a LMN lesion
- Contralateral deviation in an UMN lesion
Examination of the Limbs
The patterns of signs observed while examining the limb is more important than a single sign. Examination of the cranial nerves should be performed with neurological examination of the limbs as part of a complete neurological exam
- A useful acronym – Going to postpone reflexes constitutes stupidity
- Gait
- Tone
- Power
- Reflexes
- Coordination
- Sensation
UMN vs LMN lesions
| UMN | LMN | |
|---|---|---|
| Inspection | Spastic posture | Fasciculations (initial 2 – 3 weeks), wasting |
| Tone | Increased tone +/- clonus | Decreased tone |
| Power | Weakness, Pyramidal pattern if cortical UMN lesion | Weakness, Distribution in nerve root, nerve or muscle groupR |
| Reflexes | Hyperreflexia, Extensor plantars | Hyporeflexia, Flexor plantars |
Inspection
- Inspection of the surroundings
- EKG monitor (Autonomic problems)
- Oxygen, Intravenous Infusions (IV Ig)
- Wheelchair, Mobility aids
Signs
| Sign | Nota bene |
|---|---|
| Bulk | Assess according to muscle groups (extensors, flexors, abductors, adductors) |
| Asymmetry, Deformity or Abnormal posture (dystonia) | |
| Writer’s cramp | muscles of the hand and forearm cramp when the patient tries to write |
| Torticollis (Wry neck) | ****Painful contraction of SCM |
| Retrocollis | Head tilts backwards |
| Antecollis | Head tilts forwards |
| Resting tremor | Parkinsons |
| Intention tremor | Cerebellar dysfunction |
| Proximal wasting | Deltoid, supraspinatus and infraspinatus |
| Distal wasting | 1st dorsal interosseus |
| Fasciculation | Anterior deltoid margin and 1st dorsal interosseous |
| Pronator drift | UMN weakness |
| Pseudoathetosis | ****Proprioceptor loss |
| Dysmetria | Cerebellar lesion |
| Myoclonus | Encephalitis, Trauma, Hypoxia, Toxic or metabolic encephalopathies, Degenerative diseases (CJD), Epilepsy syndromes (Juvenile myoclonic epilepsy, Lennox-Gastaut syndrome) |
| Tics | Tourette’s syndrome |
Gait
- Clinical method
- Observe the patients casual gait (preferably with the patient unaware of being observed)
- Ask the patient walk toward you while walking on the heels, then walk away from you on tiptoes
- Ask the patient to walk in tandem (placing one foot directly in front of the other as if walking on a tight rope)
| Gait | Nota bene |
|---|---|
| Delayed initiation | Parkinson |
| Loss of arm swing | Early Parkinson |
| Festination | Parkinson |
| Scissoring | UMN lesion (due to spasticity) |
| Waddling | Proximal muscle weakness |
| Foot drop | LMN lesion (L4, L5, or peronela nerve) |
| Heel-to-Toe walking | Test for Ataxia |
| Romberg’s | Loss of proprioception |
Tone
- Clinical method
- Ask the patient to voluntarily relax their muscles before testing tone. The muscles should not be floppy or flaccid
- Test shoulder, elbow, wrist, and supinator catch
- Hypotonia: often subtle and difficult to distinguish. Indicates an LMN lesion
- Hypertonia: UMN lesion
- “Pastry-roll” each leg: Tests ankle mobility
- Heel lifts off bed when the knee is lifted suddenly: Increased tone
- Ankle clonus (> 5 beats, Tested with knee bent)
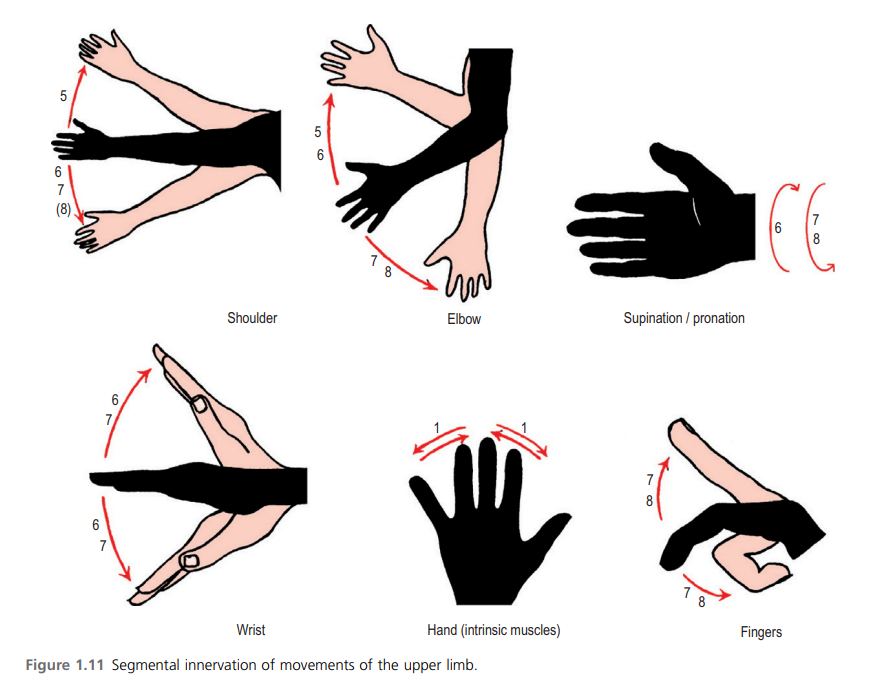
Power
- Clinical method
- Start proximally
- First ask the patient to hold their arms out in front to test any major weaknesses.
- Hand drifts downwards and pronates in UMN lesion.
- Describe in terms of proximal vs distal and unilateral vs bilateral
Movement and nerve roots for the upper limb
| Movement | Muscle | Root | Nerve |
|---|---|---|---|
| Shoulder abduction | Deltoid | C5 | Axillary |
| Elbow flexion | Biceps | C5, C6 | Musculocutaneous |
| Elbow extension | Triceps | C7 | Radial |
| Wrist flexion | Flexor carpi radialis and ulnaris | C8 | Median and Ulnar nerve |
| Wrist extension | Extensor carpi radialis and ulnaris | C7 | Radial and posterior interosseous nerve |
| Finger abduction | Dorsal interossei and abductor digiti minimi | T1 | Ulnar |
| Thumb abduction | Abductor pollicis brevis | C8 | Median |
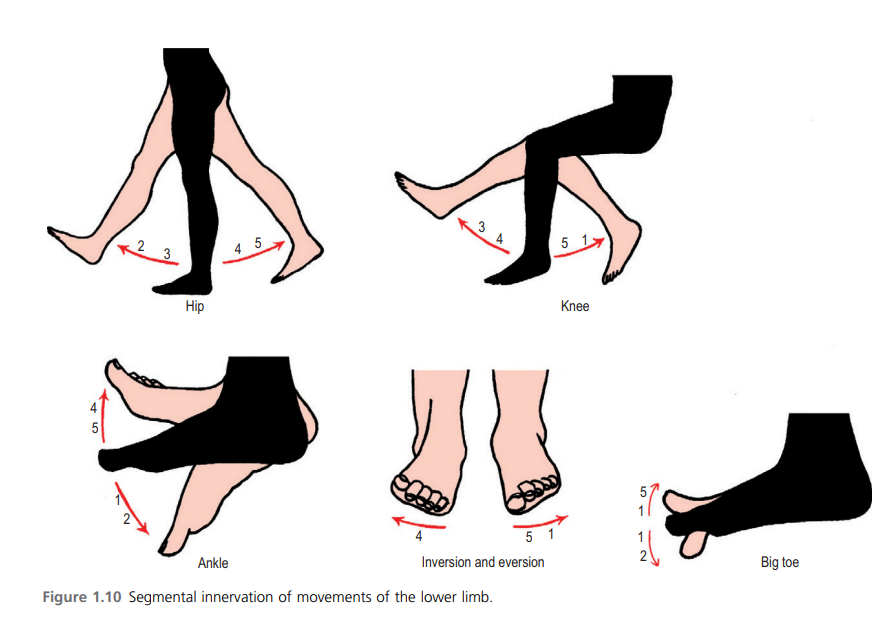
Movement and nerve roots for the lower limb
| Movement | Muscle | Root | Nerve |
|---|---|---|---|
| Hip Flexion | Iliopsoas | L1, L2 | Femoral |
| Hip Extension | Gluteus Maximus | L5, S1 | Inferior Gluteal |
| Knee Extension | Quadriceps | L3, L4 | Femoral |
| Knee Flexion | Hamstring | S1 | Sciatic |
| Ankle Dorsiflexion | Tibialis anterior | L4 | Deep Peroneal |
| Ankle plantarflexion | Gastrocnemius | S1, S2 | Tibial |
| Big Toe Extension | Extensor Hallucis Longus | L5 | Deep Peroneal |
Grading power using the MRC power scale
| Points | Finding |
|---|---|
| 0 | No movement (total paralysis) |
| 1 | Flicker or trace contraction (palpable or visible) |
| 2 | Movement with gravity but not against |
| 3 | Movement against gravity but not resistance |
| 4 | Active movement against some resistance. (4-) active movement against slight resistance (4) active movement against moderate resistance (4+) active movement against near total resistance |
| 5 | Normal power against full resistance |
| NT | Not testable |
Reflexes
- Clinical method
- Hold hammer at the end and let if fall in a fluid movement
- Reinforce by asking the patient to clench their teeth or reinforce with Jendrassik manoeuvre if necessary (Patient locks finger and pulls)
- Remember to look at the muscle belly when testing
Reflexes and their nerve roots for the upper limb
| Reflex | Root | Nerve |
|---|---|---|
| Biceps | C5, C6 | Musculocutaneous |
| Supinator | C6, C7 | Radial |
| Triceps | C7, C8 | Radial |
Reflexes and their nerve roots for the lower limb
| Reflex | Root | Nerve |
|---|---|---|
| Knee | L3, L4 | Femoral |
| Ankle | S1, S2 | Sciatic |
| Plantar | Extensor in UMN lesion, Flexor (normal) or absent |
Grading reflexes
| Grade | Finding |
|---|---|
| 0 | absent |
| 1 | reduced (hypoactive) |
| 2 | normal |
| 3 | increased (hyperactive) |
| 4 | clonus |
Signs
| Sign | Description |
|---|---|
| Hoffman sign | Present when a downward flicking of the middle finger at the DIP joint elicits involuntary flexion of the neighbouring fingers. Indicates UMN dysfunction in the corticospinal tracts |
| Babinski sig | Present when stroking the lateral sole of the foot from posterior to anterior with a sharp edge causes an upgoing big toe and finning of the toes |
Coordination and Cerebellar Testing
- DANISH for cerebellar signs
- Dysdiadochokinesia
- Ataxia
- Nystagmus
- Intention tremor
- Slurred speech
- Hypotonia
- Clinical method (upper limb)
- Finger tapping: ask the patient to make a fist with the right hand, extend the thumb and index finger and tap the tip of the index finger on the tip of the thumb as quickly as possible
- Finger-nose test: look for dysmetria and intention tremor
- Rapid alternating hand movements: look for dysdiadochokinesia
- Clinical method (lower limb)
- Omit this test if the lower limb is week
- Heel-shin test: Look for dysmetria and intentional tremor
- Tap feet on floor or end of bed: look for dysdiadochokinesia
Sensation
- Clinical method
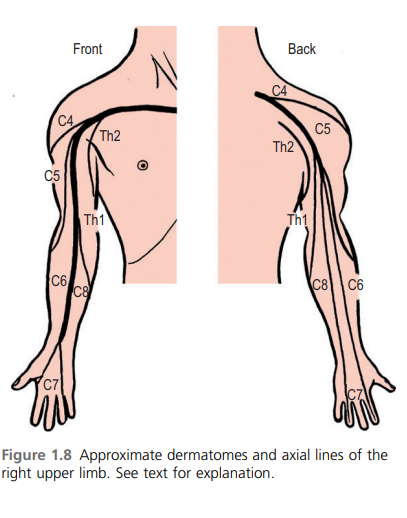
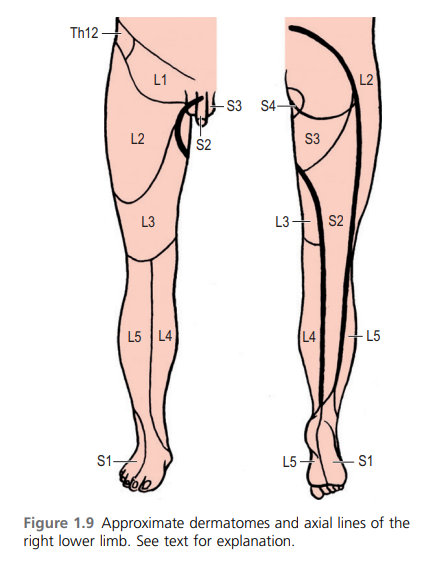
- Test distally to proximally looking for glove (peripheral neuropathy) or dermatomal (nerve root) loss of sensation. Ask the patient to close their eyes and look for extinction.
- Light touch: Spinothalamic pathway
- Wisp of cotton: dorsal columns, to refine deficit if it is detected
- Pin prick and temperature: spinothalamic columns, to refine deficit if it is detected
- Tuning fork vibration: Dorsal columns, to refine deficit if it is detected
- Proprioception: Dorsal columns, to refine deficit if it is detected
Signs
| Sign | Description |
|---|---|
| Stereognosis | Ability to identify the shape and form of a 3-D object |
| Graphesthesia | Ability to recognize symbols or letters or numbers written on the skin by touch |
Meningism
Meningism is inflammation or irritation of the meninges which leads to increased resistance to passive flexion of the neck or extension of the leg. The patient may lie with their hips flexed to ease symptoms.
- Differentials for meningism
- Meningitis
- Subarachnoid hemorrhage
- UTI
- Pneumonia
- Clinical method
- Neck stiffness: Place your hands on either side of the patient’s head supporting the occiput. Flex the head gently until the chin touches their chest and hold for 10 seconds. If the neck cannot be passively flexed or spasm are felt neck stiffness is present
- Brudzinski sign: Flexion of the hip and knees in response to neck flexion
- Kernig sign: Flex one of the patient’s legs to 90 degrees at both the hip and knee with the left hand feeling over the hamstring. Positive when extension is resisted by spasms of the hamstrings.
- These signs are absent with local causes of neck stiffness e.g. cervical spine disease or raised ICP.




