- Pre-Hospital Treatment and First Aid
- Outpatient management
- Hospital Management of Burns
- Indications for Admission
- Primary Survey and Resuscitation
- Secondary Survey
- Fluid Resuscitation
- Infection control
- Surgical Treatment
- Escharotomy
- Wound management
- Pain Control
- Nutrition
- Long-term management (Rehabilitation/Reconstruction)
Pre-Hospital Treatment and First Aid
- Pre-hospital treatment (emergency)
- Assume inhalation injury or CO poisoning and give 100% oxygen
- Assess need for intubation
- IV access and give IV fluids if possible
- Assume as trauma patient and assess for other injuries
- First aid for flame burns
- The goal is to remove from flame source and stop the burning process
- Remove involved clothing (synthetic fibers e.g. nylon, polyester, raynon burn rapidly and melt into skin, continuing to burn)
- Douse with running water for 20 minutes (beware of hypothermia in infants, young children, and adults >25% TBSA)
- Cover burns with cling wrap to prevent moisture loss
- Cover with clean, dry towel to prevent hypothermia
- First aid for chemical burns
- Dust off if powder
- Douse with running water
- Do not neutralize (can generate heat)
- First aid for electrical burns
- Survey the scene to ensure no further danger to the rescuer
- Turn off source of power or remove the victim from the source
- Assess whether CPR is required
Outpatient management
Outpatient management is reserved for burns that cover <10% BSA (<5% in children and elderly) and no third-degree burns. Treatment involves disinfection, dressing, and pain management. Inpatient observation overnight is recommended for patients with comorbidities that make healing difficult e.g. diabetes
- Treatment of first-degree burns
- Non-adherent dressing
- NSAIDS
- Treatment of second-degree burns
- Cleaning
- Do not deroof, but can lance tense blisters
- Topical agents: Silver-sulfadiazine or Triple cream ointment (for facial burns)
- Dressing (should be changed daily)
- NSAIDS
- Treatment if fever or worsening of erythema or pain (cellulitis)
- PO antistaphylococcal penicillin e.g. flucloxacillin or 1st gen cephalosporin e.g. cephalexin
Hospital Management of Burns
Management of burns takes place in 3 stages:
| Stage | Timeline |
|---|---|
| Primary survey and resuscitation | Onset of injury to completion of fluid resuscitation |
| Acute phase | Beginning of diuresis to near completion of wound closure |
| Long-term management (rehabilitation/reconstruction) | From major wound closure to return of individual’s optimal level of physical and psychosocial adjustment |
- Resuscitation
- Prevention of shock
- Prevention of respiratory distress
- Detection and prevention of concomitant injury
- Wound assessment and initial wound care
- Acute phase
- Wound care and closure
- Blood Transfusion
- Pain control
- Antimicrobial therapy
- Nutritional support
- Prevention or treatment of complications including infections
- Rehabilitation/Reconstruction
- Prevention of scarring and contractures
- Physical, occupational and vocational rehabilitation
- Functional and cosmetic reconstruction
- Psychological reconstruction
Indications for Admission
- Indications for admission
- Partial thickness burns > 10-15% in teens and adults
- Partial thickness burns > 5-10% in children and elderly
- Full-thickness burns > 2%
- Partial thickness and Full-thickness burns involving the face, hands, perineum, or feet; cross a major joint; or circumferential
- Significant electrical burns
- Significant chemical burns
- Inhalation injury
- Other criteria
- Patient with significant comorbidities e.g. Diabetes, Renal Failure
- Patients with concomitant trauma e.g. Fracture
- Very young (< 5 years) or very old (>55 years)
- Psychiatric patients where wound care may be a challege
- Non-compliant patients
- Patients with suspected or known history of drug abuse
- Patients who may not be safe at home (suspected abuse)
Primary Survey and Resuscitation
- Airway and Breathing with C-spine control
- Upper airway injury (above the glottis). Patients who have inhaled smoke or superheated air (leading to laryngeal edema) may have respiratory compromise and require early endotracheal or nasotracheal injury intubation. Delayed intubation→ difficult because of swelling. If delayed → emergency cricothyroidotomy
- Lower airway injury (below the glottis). Assess for expectoration of sputum with carbonaceous particles. Fiberoptic Bronchoscopy to look for damage to the respiratory tract
- Circumferential burns around the neck and chest: Escharotomy
- Carbon monoxide poisoning: early intubation with supplemental 100% oxygen. Nasal cannula OR NRB (Smoke exposure. To displace CO)
- Keep the neck in line with the spine without movement
- Circulation
- Establish venous access points: For obtaining labs and fluid resuscitation (16 G needles to get the fluids in as quick as possible)
- **Fluid resuscitation with RL (**in adults with >20% TBSA or children with > 15 % TBSA; RL buffers acidosis). 1/2 volume of resuscitation fluid is given in the first 8 hours, and the remaining half over the next 16 hours. RL is preferred over hypertonic saline/human albumin/colloid resuscitation.
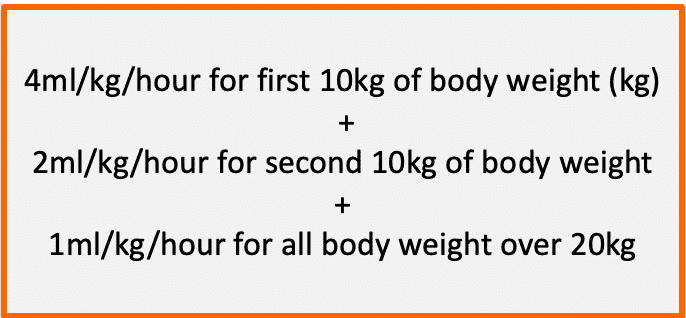
- Children: 24H of RL (3mL x TBSA X weight in kg) → 24H of maintenance D5RL (4 -2 – 1 rule for maintenance requirements)
- Adults: 24H of RL calculated by ATLS/Parkland recommendations
- Disability
- Evaluate for possibility head injury and spinal cord injury
- Check AVPU
- Check pupillary response to light
- Exposure
- Expose and assess total body surface area
- Remove jewelery, rings, amultes, and necklaces
- Use warmers and blankets to prevent heat loss, and cover all burns as soon as possible
- Adjuncts
- Labs: CBC, BMP, GXM, Carboxyhemoglobin, CXR (Respiratory burns), EKG, Cardiac Enzymes (Electrical burns)
- Foley catheter: Get Urinary sample for myoglobin, measure urine output (0.5 – 1mL/kg in adults, 1mL/kg in paeds)
- NG tube: decompressing the GI tract since >20% BSA can develop ileus
- Pulse oximetry (respiratory burns or exposure to fire CO can have falsely elevated O2 sat. Get carboxyhemoglobin level and subtract)
- CO oximetry
- Tetanus toxoid
- Remove jewelery
- Investigations
- CBC with differenital, RBS, U/E/Cs (possibility of myoglobinemia), GXM, Toxicology screen, Septic screen (blood culture, urine culture),
- Electrical burns: EKG, Cardiac enzymes, urine myoglobin, CT head if LOC
- Respiratory burns: Carboxyhemoglobin, CXR, ABGs, Cardiac enzymes, EKG
- Any other tests depending on co-existing injuries
Secondary Survey
- Patient History
- Demographic data: name, age, sex, address
- Past medical history
- Medications
- Allergies
- Tetanus immunisation
- Social situation: school, work and family
- Accident History
- Where did it happen?
- When did it happen?
- How did it happen?
- Who was involved?
- Has treatment been given elsewhere? (fluids, antibiotics)
- Head to toe examination
- Musculoskeletal: lacerations, bruises, abrasions, loose/absent teeth, swellings, deformities, pain and tenderness
- Respiratory: cyanosis, bilateral air entry
- Neurological: power, tone, reflexes and sensation in all limbs, cranial nerves
- Cardiovascular: heart sounds, jugular venous pressure
- Gastrointestinal: organomegaly, bowel sounds
Fluid Resuscitation
Fluid resuscitation can save the life of a burn victim. Formulas can be used to calculate additional fluid needed for burn patients. Maintenance fluid can be added to this volume if necessary. Burns > 15%TBSA (children) and 20%TBSA (adults) will need formal resuscitation because of third spacing. A large burn causes generalised oedema as fluid is forced to move from the circulation into subcutaneous tissue. This can lead to hypovolemic shock and death.
Calculating fluid resuscitation
Generally, 2-4 ml per %TBSA per kg are used depending on the patient’s conditions. Maximum %TBSA used for the formula is 50%. Crystalloids (Ringers Lactate or Harman’s > Normal saline) are preferred. Colloids are not useful for the first 8 hours since they will leak into subcutaneous tissue and cause more oedema. 2nd and 3rd-degree burns have some level of edema and will also require resuscitation. Adequate resuscitation should be matched with a urine output of 1 – 1.5 ml/kg and an adequate MAP. Paediatric patients should also receive dextrose containing crystalloids at their calculated maintenance rate due to a risk of hypoglycaemia.
If a patient arrives 24 hours since burn, immediate resuscitation period has passed and the patient is at risk of dehydration. Crystalloid fluids can be started (500ml for adults, 20ml/kg for children). The formulas can be used to calculate the amount of fluid required, and the response monitored via vital signs and urine output.
Formulas for calculating fluid resuscitation
| Formula | Calculation |
|---|---|
| Parkland formula for adults | V = (% area burn) x (kg weight) x (4 ml/kg) |
| ATLS recommendation for adults | V = (% area burn) x (kg weight) x (2ml/kg) |
| ATLS recommendation for paediatrics | V = (% area burn) x (kg weight) x (3ml/kg) |
| ATLS recommendation for electrical burns | V = (% area burn) x (kg weight) x (4ml/kg) |
- Administration
- 1/2 volume over the first 8 hours
- 1/2 volume over the remaining 16 hours
Infection control
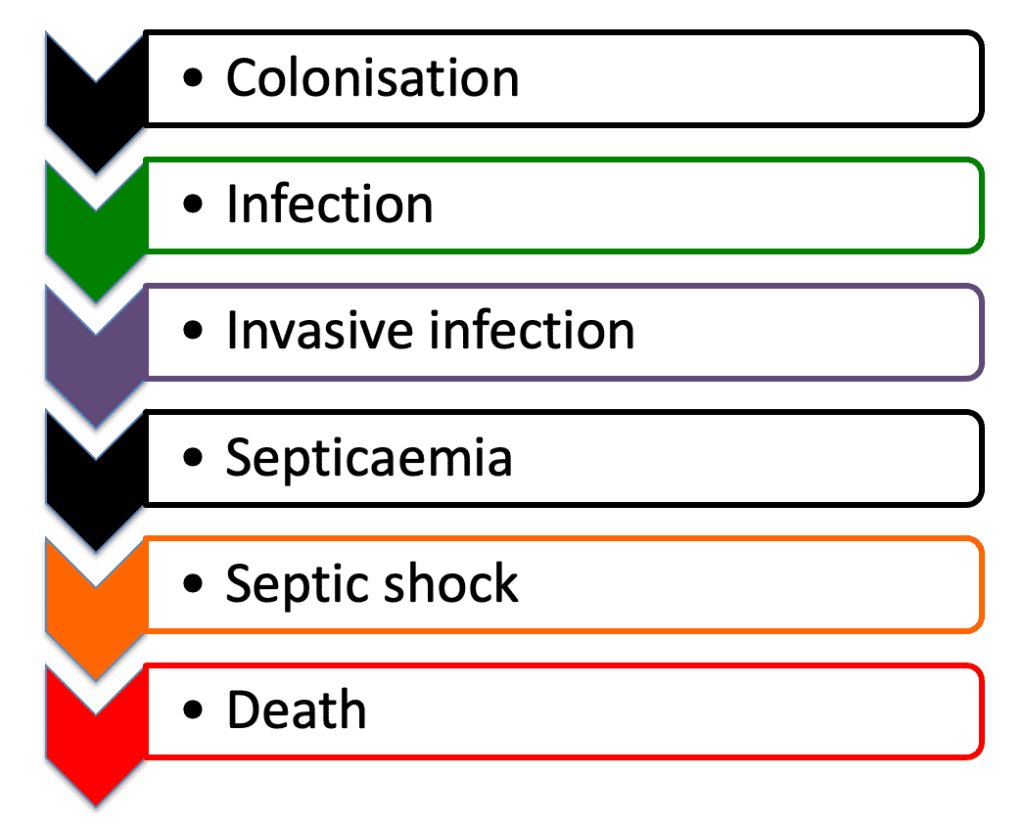
Burns wounds are initially sterile but can become contaminated within a few hours. An infected burn wound has 10^5 microorganisms per gram of tissue. Good hygiene is practical, safe and more cost-effective than prescribing antibiotics for burn wounds
| Term | Description |
|---|---|
| Colonisation | Colonisation by bacteria (mostly staphylococci) in the first 48 hours. Other microbes colonise the wound at about 5 – 7 days |
| Infection | The burn wound changes appearance. There might be erythema or increased pain |
| Invasive infection | Pathogens are present in enough concentration to cause suppuration and invasion of unburned tissue. Can appear as progressive black patches. |
| Septicaemia | Circulating bacteria in the bloodstream can trigger sepsis, or septic shock. Antibiotics should be started immediately. |
| Septic shock | This is an emergency. The patient is critically unwell and is unable to maintain their circulation. |
- Signs and symptoms of infection
- Dressing soiled, stained or smelly (a green staining indicates colonisation or infection by pseudomonas)
- Cellulitis wound (erythema, warmth, tenderness)
- Patchy black areas of necrosis (invasive infection)
- Extensive slough (invasive necrosis)
- Wound swab, culture and biopsy can identify the pathogenic organism
- High fever (39 C) + pallor, shivering, tachycardia, tachypnoea, lymphadenopathy, inability to tolerate feeds, abdominal distension, thrombocytopenia, hyperlgycemia
- Cough, sputum, and breathlessness (pneumonia)
- Dysuria, frequency (urinary tract infection)
- Consequences of infection
- Delayed or non-healing wounds
- Hypertrophic scars and contractures
- Pain and suffering
- Higher cost due to longer stay and medications
- Death
- Infection control
- Be aware of signs and symptoms
- General infection prevention and control measures
- Treat infection as soon as they occur with local application of antimicrobials, cleaning the wound, and surgical debridement
- Reserve antibiotics for patients with signs and symptoms of infection
- Supply a nutrition-rich diet to promote healing
- Treatment of an infected wound
- Remove dressing and clean with antibacterial solution e.g. Betadine using aseptic technique
- Surgical debridement for invasive infection
- Topical antimicrobial and clean dressings




Surgical Treatment
Early surgery improves outcomes of burn patients. Early excision and grafting (within 1 week) is beneficial for deep partial thickness and full thickness burns. Burns that do not heal within three weeks should be treated surgically e.g. deep burns, over joints and special areas, and infected burns. Treating a burn wound conservatively could lead to weight loss, contractures and infection (sepsis).
Surgery for burn wounds
| Term | Description |
|---|---|
| Debridement | Removal of dead or infected tissue. Dead tissue hosts bacteria and needs to be removed. Debridement can be performed through tangential or fascial excision |
| Tangential excision | Shaving layers of the burn until bleeding tissue is reached. The bleeding tissue can take a skin graft |
| Fascial excision | Removing the whole of subcutaneous tissue down to muscle fascia. Fascia can take a skin graft. |
Skin grafting
| Term | Description |
|---|---|
| Skin grafting | Skin is harvested using skin graft knife or dermatome |
| Meshing | Meshing inserts fenestrations into the graft. This increases the surface area as the graft can be stretched and expanded. It also allows blood to leak preventing hematoma from forming below the graft. The downside is that mesh grafts have a cosmetic downside. |
| Donor site | Usually the upper thigh and back (thick skin that heals quickly) but any area of non-burned skin can be used in extensive burns. |
| Dressing | The graft is immobilised for 48 hours with the joints splinted. The skin graft can be dressed with a non-adherent layer (vaseline gauze, absorbent wool or a firm bandage). |
- When to graft?
- Early excision of burns is better than waiting for the wound to form granulation tissue
- Clean and bright red granulation tissue without overlying slough is more likely to take graft
- Chronic wounds have thick granulation tissue that is colonised by bacteria and are not suitable for grafting
- Indications for blood trasnfusion
- Transfusion is restricted to Hb concentrations of 7-8 g/dL in patients without other indications for blood transfusion e.g. ongoing bleeding
- Techniques to reduce blood loss
- Timing of surgery: excise the burn wound within a few days to reduce bleedingAdrenaline solution: 1ml of 1:1000 adrenaline to 1 litre of saline. Injected under the area of burn to be excised to the donor sites. Gauze swabs can also be soaked in the solution and applied on the wound to reduce bleeding.Tourniquets applied to an extremity to reduce bleeding



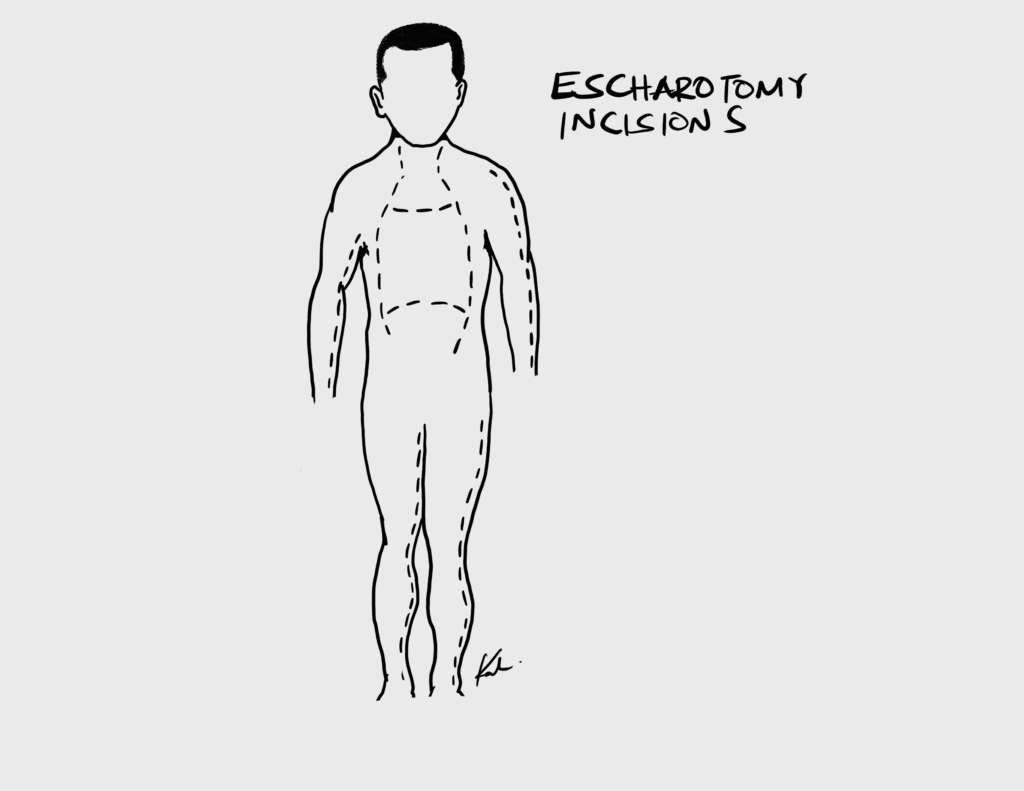
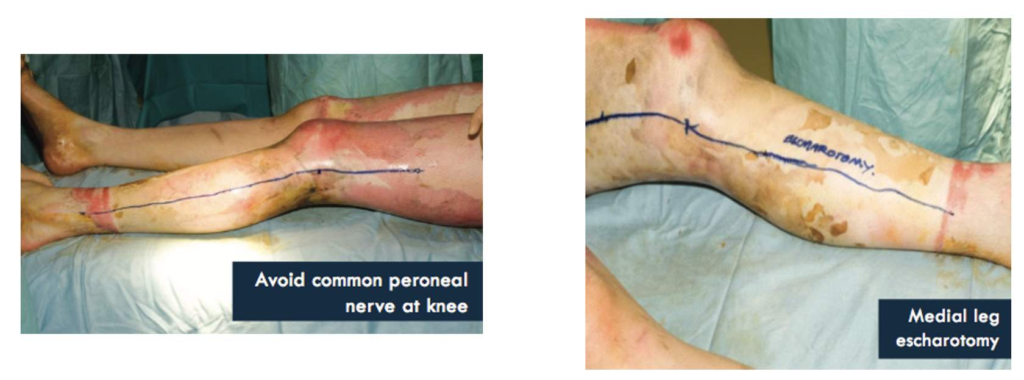
Escharotomy
An eschar is thickened burn tissue. Escharotomy can be performed within 8 hours or when there is clinical compromise of circulation or ventilation. This can be done during debridement for burns in the chest, and upper and lower extremities to prevent compartment syndrome. Fasciotomy is performed if compartment syndrome develops. A scalpel or cutting diathermy can be used. The patient’s perfusion and ventilatory status should be monitored in case escharotomy needs to be deepened due to further oedema
Escharotomy incisions
| Location | Incision |
|---|---|
| Upper limb | Mid-lateral on each side. Anterior to elbow medially to avoid the ulnar nerve. Caution to avoid the median nerve in the antecubital fossa. |
| Hand | Midline in the digits. Release muscle compartment if tight |
| Lower limb | Posterior to the ankle medially to avoid the saphenous vein. Caution to avoid the posterior tibial vessels. |
| Chest | Down the chest lateral to the nipples. Across the chest below the clavicle. Across the chest at the level of the xiphisternum. Cross-hatched to allow for expansion fo the chest |
| General rules | Extend the wound beyond the deep burn. Diathermy any significant bleeding vessels. Apply haemostatic dressing and elevate the limb post-op |

Wound management
Wounds should be cleaned and small blisters kept (acts as biological dressing). Topical agents including silver sulfadiazine and mafenide acetate, and dressing can be used. Exposure method is used for facial and perineal burns where dressing is difficult to apply but healing is good. It is nurse-intensive compared to closed method.
Topical agents
| Topical Agent | Characteristics |
|---|---|
| Silver sulfadiazine (1%) | Bacteriostatic. Can cause neutropenia and thrombocytopenia. Poor tissue penetration. Ineffective against pseudomonas |
| Mafenide acetate | Painful on application. Can cause metabolic acidosis since it functions as a carbonic anhydrase inhibitor. Deep tissue penetration. Effective against pseudomonas |
| Silver nitrate (0.5%) | Bacteriorstatic. Poor deep tissue penetration. Ineffective against Pseudomonas; Brown staining of skin is common. Methemoglobinemia may rarely occur. |
| Povidone Iodine (8.5%) | Antibacterial and antifungal. Useful for minor wound infections. |
- Principles of managing burn wounds
- Analgesia and anxiolysis before dressing e.g. ketamine, midazolam or tramadol + distraction
- Clean the wound
- 2 layers of dressing can be used: and inner layer (non-adherent e.g. paraffin gauze) and outer layer (thick and absorbent e.g. wool and a firm bandage).
- Change dressing every day at first then as needed e.g. when bandages are soiled or wet
- Elevate the limbs to prevent and control oedema
- Position in anti-deformity positions
- Allow full joint movement, especially in the hands i.e. by using individual finger dressings
- Treatment for 2nd and 3rd degree burns with no eschar present
- 1% Silver sulphadiazine
- 0.5% silver nitrate cream
- Early excision and grafting
- Treatment for burns with eschar
- Mafenide acetate
- Escharectomy during debridement
- Treatment for burns to the face
- Triple antibiotic ointment – Neosporin (bacitracin, neomycin, polymixin B)
- Options for wound coverage
- Autografts (split-thickness and full-thickness)
- Acellular dermal matrix (Alloderm, Xenoderm)
- Engineered synthetic dermal substitutes (integra)
Pain Control
A combination of pharmacological and non-pharmacological techniques can be used to control pain e.g. ketamine + distraction while changing dressing. Give adequate analgesia when wounds are being changes. Preventing pain encourages activity in the future. There is also background pain so analgesia should be given regularly during the day.
- Pain control
- First and second degree burns that are treated as outpatient: discharge with NSAIDs
- Severe burns: IV opiates (morphine, fentanyl, oxycodone). Transition to oral opiates then NSAIDs
- Multimodal analgesia (use of several drugs in combination)
- Non pharmacological strategies e.g. distraction, relaxation tapes, visualisation, guided imagery, meditation, music, comfortable positioning, and timing of dressing.
Nutrition
Burn patients are catabolic. Very early enteral feeding is recommended. An NG tube is indicated for all patients with burns > 15% TBSA. TPN can be given using a central line if enteral feeding is not tolerated. Weight should be monitored regularly. If a patient loses > 10% pre-morbid body weight they are at risk of complications.
- Calculating nutritional requirment
- Indirect Calorimetry (IC) is the gold standard for assessing nutritional requirement
- Other formulas: Harris-Benedict, Curreri, Ireton-jones, and Toronto can be used to calculate nutritional requirments. Their disadvantage is that the underfeed in the early periods of highest energy use and overfeed in the later periods
- Sutherland formula
- Children: 60 kcal/ kg + 35 kcal %TBSA
- Adults: 20 kcal/ kg + 70 kcal %TBSA
- 1.5- 2g/ kg of protein per day
- Protein 20% of energy requirements
Long-term management (Rehabilitation/Reconstruction)
Rehabilitation starts as soon as possible and can continue for years. Positioning, splinting and rehabilitation are important, even for relatively small burns which can develop serious contractures. Mobilise patients when they are awake and use splints when they are asleep.
- Risk factors for contracture formation
- Burn across a joint
- Burn depth (≥ third degree)
- Risk factors for hypertrophic scars
- Scars that result from healing by secondary intention
- Scars which are subject to tension in two dimensions after primary closure
- N.B: affect the young, rather than the elderly, and females more than males. The anterior chest, shoulders and deltoid regions are particularly predisposed
- Prevention of contractures
- Early excision and grafting
- Early splinting in extension (anti-contracture positioning)
- Infection control to prevent full-thickness skin loss
- Physiotherapy
- Pressure garments
- Scar massage
- Reporting a contracture
- Location and joint involved
- Joint position (extension, flexion, adduction etc.)
- Degree of contracture
- Fixed or flexible contracture (caused by bony or Soft tissue changes respectively)
- Active wounds over the contracture
- Managing scars
- Moisturiser e.g. coconut oil to keep the scar hydrated
- Compression therapy using pressure garments to reduce the height of scars
- Silicone tape to reduce the height of scar
- Reconstructive surgery
Burn sites and contracture
| Site | Contracture | Anti-contracture position |
|---|---|---|
| Face | Inability to open or close mouth and inability to close eyes fully | Regular change of expression and stretching or use of a padded tube |
| Anterior neck | Neck flexion contracture | Neck extension. Pillow roll behind the neck and head tilted back if sitted |
| Posterior neck | Neck extension and other movements | Sitting with head in flexion. Lying with pillows behind the head |
| Axilla or anterior and posterior axillary fold | Limited abduction | Lying and sitting with arms abducted to 90 degrees, figure of 8 bandaging, or strapping to stretch across chest |
| Back of hands | MCP hyperextension, IP flexion, adduction of thumb, flexed wrist | Wrist 30 – 40 degrees extended, MCPs 60 – 70 degrees flexion, IP joints in extension, thumb mid-palmar radial abduction |
| Palm of hand | Fingers adducted and flexed, palm pulled inward | Wrist hyperextended, minimal MCP flexion, fingers extended and abducted |
| Groin | Hip flexion, hip adduction | Lie prone or supine with legs extended, limit sitting and side lying |
| Back of knee | Knee flexion | Legs extended in lying and sitting |
| Feet | Complex | Ankles at 90 degrees, encourage sitting with feet flat on floor as long as oedema is not present |




