Overview
Macular degeneration is the most common cause of permanent visual loss in the elderly. It is AKA age-related macular degeneration (AMD). It is a chronic condition that leads to progressive ventral visual loss. The macula is essential for central vision. Degeneration therefore leads to visual disruption causing distortion (metamorphopsia) and loss of central vision (central scotomas).
Its etiology is unknown. It typically presents as an older patient with blurry vision and dark spots that worsen over time. All patients with AMD receive regular followup with optometry. No effective surgical or medical treatment currently exists for dry AMD.
| Type of AMD | Features | Frequency | Progession of symptoms |
|---|---|---|---|
| Dry (geographic) AMD | Associated with drusen (yellow cholesterol-based debris) between the RPE and choroid | 80% | Slowly progressive |
| Wet (exudative) AMD | Associated with neovascularization of the choroid, leading to hemorrhage, ischemia, and scarring. It is more severe and progressive | 10-15% | Rapidly progressive (over days or weeks) |
- Important relevant anatomy:
- Bruch’s membrane
- Innermost layer of the choroid located beneath the retina
- Retinal pigment epithelium
- Located in the retina beneath the photoreceptors next to the choroid (Bruch’s membrane)
- Bruch’s membrane
- Risk factors
- Age (esp. 60+)
- Hypertension
- Obesity
- Elevated cholesterol
- Caucasian
- Smoking
- UV exposure
- Signs and symptoms
- Blurred central vision
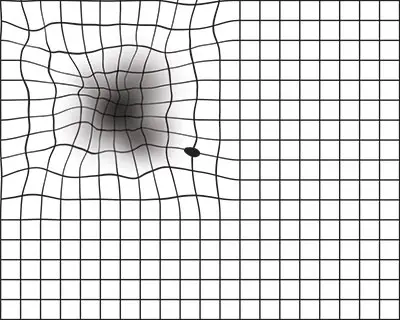
- Metamorphopsia (distorted vision)
- Dramatic decrease in visual acuity (affects the ability to read and distinguish faces)
- Decreased contrast sensitivity
- Investigations
- Ophthalmoscopy (indirect and dilated): for definitive diagnosis and differentiation (wet or dry AMD)
- Snellen chart
- Reduced visual acuity compared to the previous test
- Amsler grid
- Distortion
- Fluorescein angiography: performed in suspected wet AMD to visualize abnormal blood vessels
- Areas of bleeding (bright spots) around the macula
Dry Macular Degeneration
This is as a result of the accumulation of drusen. Drusen is yellow extracellular material that forms between Bruch’s membrane and retinal pigment epithelium (RPE). It results in gradual loss of vision. There is no specific treatment. Vitamins and antioxidant supplements may prevent it.
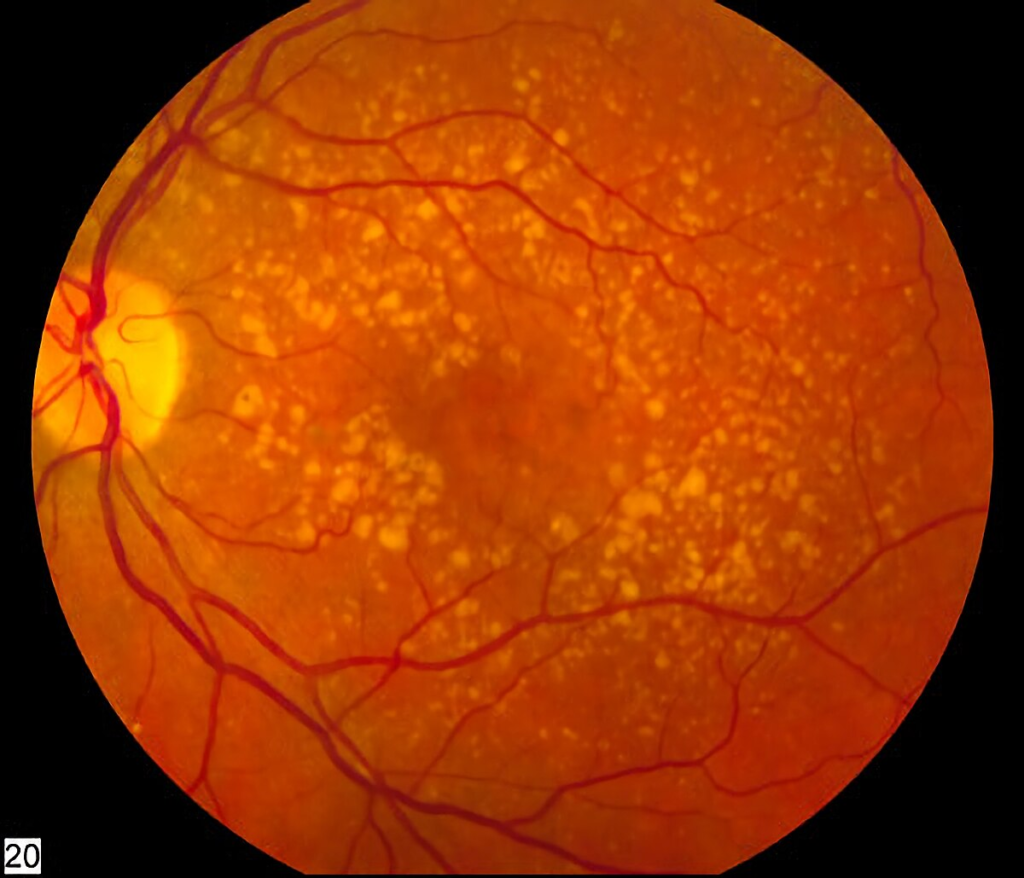
Drusen is a common finding. The presence of drusen is not pathognomonic for AMD. However, the more drusen the more likely the patient will develop AMD.
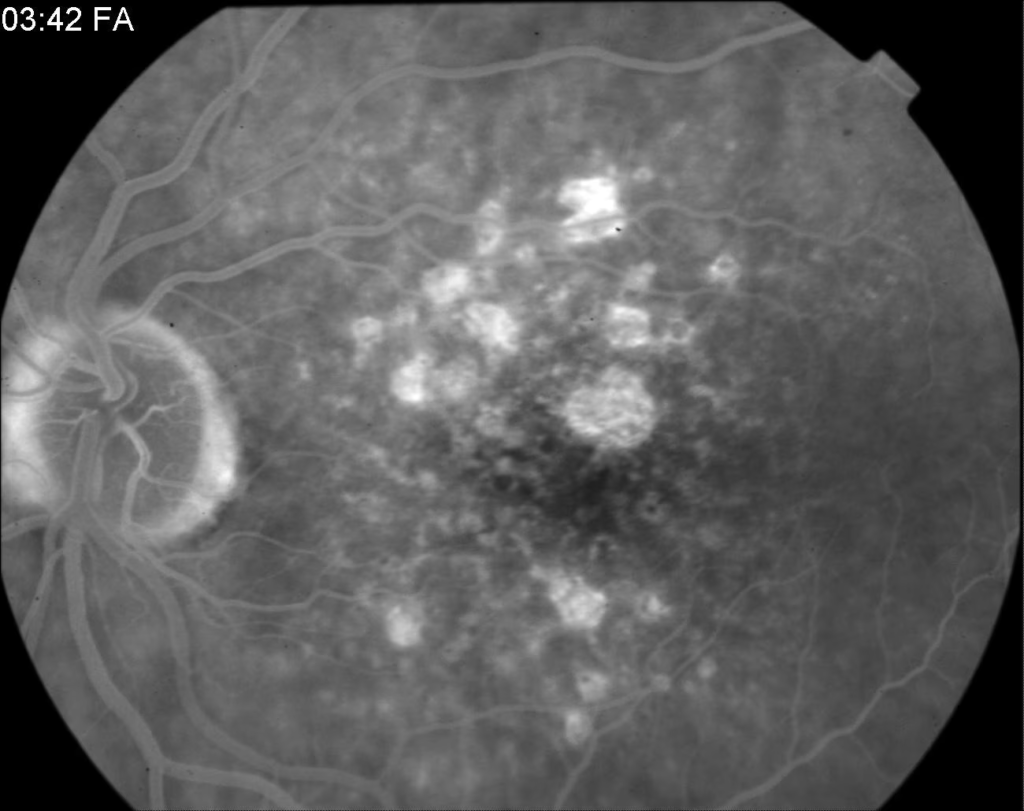
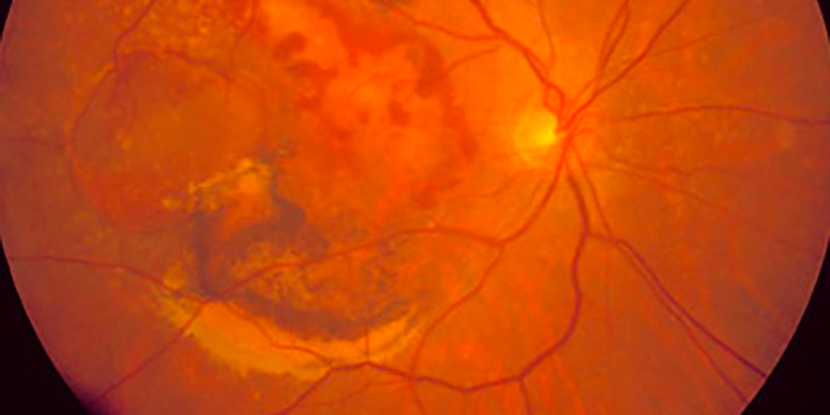
Wet Macular Degeneration
This is caused by a break in Bruch’s membrane. Blood vessels form beneath the retina which later leak and cause haemorrhage. It can progress rapidly to vision loss. Treatments include laser therapy and anti-VEGF medication (e.g. ranibizumab).
- Treatment summary
- Dry AMD
- Refer to an optometrist to facilitate care and improve quality of life
- Oral vitamins and anti-oxidants: slows progression
- Wet AMD
- Photodynamic therapy (PDT): lasers are used to coagulate abnormal vessels and slow the progression
- Anti-VEGF agents (Bevacizumab, Ranibizumab, Pegaptinib, Zivaflibercept): administered intravitreally q2-4 weeks to antagonize angiogenesis
- Oral vitamins and anti-oxidants: slows progression
- Dry AMD
- How can you improve the safety and Quality of Life for patients with AMD?
- Keep the home brightly lit
- Take precautions with stairs
- Use cane/walker for walking
- Use objects with larger symbols
- Use magnification devices
- Use colour-coded medicine bottles
- At home care
- Disability/ADA counselling if they are still working
- Talking glucometer for patients with Diabetes