Staphylococci
- Describe the general characteristics of Staphylococci.
- Gram positive
- Spherical
- Usually arranged in grape- like irregular clusters
- All produce catalase
- Common inhabitants of the skin and mucous membranes
- Non- sporing
- Non- motile (no flagella)
- May be capsulated
- Grow in high concentration salt media
- Classify Staphylococci according to coagulase production.
- Coagulase positive: S.aureus
- Coagulase negative: S.epidermidis, S.saprophyticus, S.haemolyticus
- Classify Staphylococci according to pathogenicity.
- Common pathogen: S.aureus
- Opportunistic pathogens: S.epidermidis, S.saprophyticus
- Non- pathogens: S.hominis
- Briefly describe the pathogenesis of Staphyloccoci infections.
- Cocci get access to damaged skin, mucosal or tissue site→ Colonise by adhering to cells or extracellular matrix→ Evade the host’s immune defense mechanisms and multiply→ Cause tissue damage
- What are the characteristics of Staphylococcus aureus
- Reservoir
- Skin
- Colonizes nares, ears, pharynx, axilla, hands, groin and perineum
- Biology
- Gram-positive cocci
- Arranged in grape-like clusters
- Catalase positive
- DNAse positive
- Coagulase positive
- Characteristic gold-yellow colonies
- Beta-hemolytic
- Mannitol fermenter on MSA
- Reservoir
- List common sites of staphylococcal infection
- Skin: Cellulitis, Impetigo, Abscess, Foliculitis, furuncle, carbuncle
- Heart: Acute bacterial endocarditis
- Lungs: Pneumonia
- Joints: Septic arthritis
- Bones: Osteomyelitis
- Describe the Virulence factors and resistance of Staphylococcus aureus.
- Capsular polysaccharide: anti- phagocytic
- Teichoic acid: bind fibronectin in host cells, acts as a surface adhesin.
- Lipoteichoic acids: induce septic shock by inducing cytokines, IL-1 and TNF from macrophages
- Proteins: Clumping factor A, Clumping factor B, plasmin sensitive protein, surface proteins G and H, protein A, Modified Penicillin Binding Proteins
- Protein A: binds Fc portion of IgG at complement binding sie→ prevents complement activation
- Enzymes: Catalase, reductase, staphylokinase, staphyloxanthin, Coagulase, Hemolysins (a,b,y), Hyaluronidase, Lipase, penicillinase, leucocidin, fibrinolysin, chemotaxis inhibitory protein, Beta- lactamase, Novel penicillin- binding protein
- Toxins: Toxic Shock Syndrome Toxin-1, Heat-stable enterotoxin B, Exfoliative/ epidermolytic Toxin, a-toxin
- Biofilm formation: colonisation and persistence on prosthetic devices
- Classify clinical conditions associated with Staphylococcus aureus giving two examples of each.
- Pyogenic disasese
- Localised: Impetigo, Folliculitis, Carbuncles, Furuncles, Mastitis, Surgical infections, Cellulitis or Fasciitis
- Systemic: Discitis, Endocarditis, Pneumonia, Osteomyelitis, Septic Arthritis, Epidural Arthritis (DEPOSTE)
- Toxigenic diseases: Toxic Shock Syndrome, Staphylococcal Scalded Skin Syndrome (Ritter’s disease), Food poisoning
- Pyogenic disasese
Choose one clinical condition associated with Staphylococcus aureus and discuss its pathogenesis, clinical manifestations, laboratory diagnosis and antimicrobial treatment.
| Clinical condition | Pathogenesis | Clinical manifestations |
|---|---|---|
| 1. Toxic Shock Syndrome | Females using tampons, individuals with wounds, patients with nasal packaging, TSST-1 brings MHC-II and TCR in close proximity causing massive release of IL-2, and IFN-y | Fever, hypotension, erythematous skin rash, shock, organ failure |
| 2. Food poisoning | Ingestion of heat-stable enterotoxin B, causes massive release of IL-1 and IL-2 which stimulates the enteric nervous system→ activating vomiting centre in the brain | Prominently vomiting, watery non- bloody diarrhoea |
| 3. Staphylococcal Scalded Skin Syndrome (Ritter’s disease) | Skin-skin contact or fomites, Exfoliatin cleaves desmoglein from epidermis casuing epithelial cells to slough off | Bright red flush, blisters, desquamation of the epidermis |
- Diagnosis: Pus, tissue exudates, sputum, blood, feces, vomit, food remains, nasal swabs, Gram positive cocci arranges in cluseters, singles or pairs, Golden yellow colonies, Beta hemolytic on BA and CBA, Facultative anerove, rouns, smooth, raised glistening coloies, Catalase positive, coagulase positive, DNAse positive, API staph, Automated methods i.e. VITEK, 16S or 23S RNA PCR, mecA gene for methicillin resistance, PVL gene for PCR, Phage typing for epidemiological purpose
- Treatment: Isoxazosyl penicillin, clindamycin, Vancomycin, Linezolid, Macrolides, Cephalosporins, Fusidic acid, Flucloxacillin, Daptomycin, Mupirocin
- Describe the pathophysiology and clinical features of SSSS (Ritter’s disease).
- Pathophysiology: Exfoliative toxin A and B cleave desmoglein-1 in the granular layer of the epidermis, Disruption of keratinocyte attachment
- Clinical features: Widespread sloughing of epidermal skin, Positive Nikolsky sign, No mucosal involvement, Cracking and crusting, Signs of shock (hypotension, tachycardia), Diffuse or localized erythema, often beginning periorally, Skin tenderness, Fever, malaise, irritability
- Regarding Toxic Shock Syndrome, describe the following:
- Etiology
- Staphylococcal TSS: High-absorbency tampons, prolonged tampons, cups, sponges, Nasal packing, postpartum or postabortion infections, postsurgical wound packing
- Streptococcal TSS: Invasive and nonivasive GAS infection
- Pathophysiology
- Superantigen production (TSST)
- Superantigen mediated T-cell activation (directly connects MHC II on APC to TCR on T cells forming a bridge outside the normal binding site) → non-specific T cell activation → rapid activation of excessive numbers of T cells → Massive cytokine release (IL-1, IL-6, TNF) → Systemic inflammatory response syndrome (SIRS) which consists of generalized endothelial disruption, capillary leak syndrome, generalized edema, intravascular hypovolemia, organ dysfunction and DIC
- Clinical features
- Prodrome: Flue-like symptoms, dermal rash, strawberry tongue, nonpurulent conjuctivitis, oropharyngeal hyperemia
- Shock and end-organ dysfunction: tachychardia, tahypnea, high fever, altered mental status → hypotension, delayed capillary filling, end organ failure, mucosal ulteration
- Etiology
- Describe the Laboratory diagnosis of Staphylococcus aureus infection.
- Specimen: pus, tissue exudate, sputum, urine, blood, faeces/ vomit, food remains, nasal swabs
- Microscopy: Gram positive clusters in singles or in pairs
- Culture: Golden yellow colonies, Beta hemolytic on BA and CBA
- NAAT: for MSSA and MRSA
- Biochemical tests: Catalase positive, coagulase positive, DNAse positive, API staph, 16s/ 23s RNA PCR, mecA gene, Phage typing
- molecular probes or mass spectrometry
- What is the Treatment, Prevention and Control for Staphylococcus aureus infection?
- Treatment:
- Methicillin- susceptible S.aureus: Isoxazolyl penicillin (e.g. oxacilin) or Clindamycin
- Methicillin- resistant S.aureus: Vancomycin or Linezolid
- Localized infection: incision and drainage
- Prevention and control:
- In hospitals: proper wound cleaning, antiseptic use, aseptic catheter use
- Hygiene and cleansing
- Bacterial colonisation of carriers with local antiseptics eg. nasal mupirocin and chlorhexidine soap for MRSA carriers
- Treatment:
- Why is the tube coagulase test done after performing a slide coagulase test?
- Staphylococci produce 2 coagulase:
- Free coagulase – converts fibrinogen to fibrin by activating a coagulase-reacting factor present in plasma
- Bound coagulase (clumping factor) – slide test, converts fibrinogen to fibrin without requiring a coagulase reacting factor
- Tube test is always performed when the results of slide test is not clear or when the slide test is negative and Staphylococcus has been isolated from a serious infection – required to detect MRSA
- Staphylococci produce 2 coagulase:
- Regarding Staphylococcus epidermidis, briefly describe the following:
- General characteristics.
- Gram positive
- Grape-like cluster arrangement
- White raised colonies
- Catalase positive
- Coagulase negative
- Novobiocin sensitive
- Mannitol non-fermenter
- Epidemiology
- Ubiquitous (no geographic or seasonal limitation)
- Normal flora on skin and mucosal surfaces
- Can survive on dry surfaces for long periods
- Person-person spread via direct contact or contaminated fomites
- Most infections are from the individual’s own organisms
- Patients at risk when foreign objects are present
- Hospital personnel are a major reservoir for antibiotic- resistant strains
- Virulence factors and resistance
- Urease
- Adherent biofilm production – synthesis of extracellular polysccharide matrix (glycocalyx)
- Protects from host defense and antibiotics
- Facilitates colonization of surfaces of prosthetics and IV catheters (Device-associated infection)
- Diseases caused
- Foreign body infections
- Prosthetic devices (heart valves, orthopedic implants) ; subacute endocardits, UTI
- IV catheters (frequent contaminant of blood cultures)
- Peritonitis in dialysis patients
- CSF shunt infections
- Neonatal sepsis
- Foreign body infections
- Diagnosis
- Similar to S.aureus infection
- Treatment, prevention and control
- Isoxazolyl Penicillin (Oxacillin or other penicillinase-resistant penicillin) or Clindamycin
- Vancomycin or Daptomycin (for methicillin resistant strains)
- Removal of foreign body
- Promp treatment of endocarditis or shunt infection in order to prevent further tissue damage or immune complex formation
- General characteristics.
Regarding Staphylococcus saprophyticus, briefly describe the following:
- Reservoir
- Natural flora of the female genital tract and perinuem
- Infrequently on skin, or in the intestines
- General characteristics
- Gram positive coccus
- Grape-like clusters
- Catalase positive
- Coagulase negative
- Novobiocin resistant
- Virulence factors and resistance
- Urease producer
- Lipase
- Disease caused
- UTIs in seually active
- Opportunistic in immunosuppressed: strong association with foreign bodies eg. IV catheters
- Treatment
- 1st generation cephalosporin (e.g. cephalexin)
- Amoxicillin-clavulanate
- Fluoroquinoone (e.g. ciprofloxacin)
- Nutrofurantoin
- TMP-SMX
Streptococci
- List the at-risk population, virulence factors, clinical conditions and laboratory diagnosis of Streptoccocus pneumonia
- At-risk population: asplenics, immunocompromised, adults 65 years or older, children less than 2 years of age
- Virulence factors: Capsule, IgA protease, Pneumolysin, Autolysin, neuraminidiase, surface protein adhesins
- Clinical conditions: Pneumococcal pneumonia, Otitis media, Sinusitis, Pharyngitis, Meningitis, Septicemia and bacteremia, conjunctivitis, osteomyelitis (vertebral), overwhelming post-splenectomy infections (OPSI)
- Laboratory diagnosis
- Specimen: Sputum, pus, blood, CSF, ear and eye exudates
- Antigen detection
- Culture: CBA in CO2 enriched atmosphere, 35-37*C, <1mm diameter, grey white or colourless, dry or shiny and usually irregular outline, alpha hemolytic on BA, Draughtsman appearance on BA
- Gram smear: Gram-positive cocci, capsulated, non-motile, elongated (lancet-shaped) diplococcus, may form short chains
- Biochemical identification: Catalase negative, Optochin sensitive, Bile solube, CAMP negative, API STREP combines these biochemical tests into a strip
- Serology: Quellung reaction, ELISA, Sertotyping
- Antimicrobial susceptibility: penicillin
- Treatment: Vancomycin and ceftriaxone,
- Prevention: Capsular polysaccharide vacicine (pneumovax), pneumococcal conjugate vaccine (prevnar)
- List the virulence factors, clinical conditions and laboratory diagnosis of Streptococcus pyogenes
- Virulence factors
- Toxins: Erythrogenic exotoxin A, Streptolysin O, Streptolysisn S, Streprococcal pyrogenic exotoxin
- Enzymes: DNAse, Streptokinase, Hyaluronidase, C5a peptidase, Serine protease
- Protetins: Protein D (fibronectin-binding adherence to epithelium), M protein (prevent C3b opsonisation)
- Hyaluronic acid capsule
- Lipoteichoid acid
- Lab diagnosis
- Specimen: Throat swab, pus, high vaginal swab, blood
- Microscopy: Gram positive cocci in chains
- Serology: Group A antigen via agglutination using Group A antibodies, ASOT (throat-associated), **Anti-DNAse B (**pyoderma-associated diseases)
- Culture: grey, white or colourless, dry shiny, irregular outline colonis on BA, Beta hemolytic
- Gram smear: Gram positive non-motile coccy,
- Biochemical identification: Catalase negative, Bacitracin sensitive, PYR positive, CAMP negative
- Treatment: Penicillin V, Amoxicillin, Oral cephalosporins or Macrollides, resistant to tetracyclins, IV penicillin and clindamycin for systemic infections, Vancomycin, daptomycin, linezolid
- Virulence factors
- Classify the diseases caused by Streptococcus pyogenes giving examples under each.
- Pyogenic: pharyngitis, meningitis, pneumnia, skin and soft tissue infections: cellulitis, necrotizing fasciitis, pyomyositis, impetigo, erysipelas), Invasive: puerperal sepsis, acute bacterial endocarditis, necrotizing fascitis
- Toxigenic: Scarlet fever, Toxic shock-like syndrome,
- Immune mediated: Acute rheumatic fever, poststreptococcal glomerulonephritis
- What is the ASOT test? What are its indications and significant titers?
- Microbe: Streptococcus pyogenes
- Principle: Latex agglutination – ASO latex particles coated with Streptolysin O agglutinate on contact with serum containing ASO antibodies
- Significant titres: >200 IU/ml (200-3500)
- Indications: Investigation of post-streptococcal disease, particularly rheumatic fever, which occurs 2 – 3 weeks or more after streptococcal pharyngitis when it is not possible to isolate Streptococcus pyogenes in culture
- Causes of false positive: Rheumatoid Arthritis, Tuberculosis, Pneumococcal pneumonia, Gonorrhoea, Hepatitis, Lipaemic or bacterially contaminated serum
- Other immunological complications associated with strep pyogenes: Poststreptococcal glomerulonephritis
- Outline the laboratory diagnosis of streptococcal infections (5)
- Specimen: Throat/ nose swab, pus, blood, high vaginal swab, CSF, sputum, urine
- Microscopy: Gram-positive cocci arranged in chains, non-motile , may appear in chains or singly
- Culture: aerobic and anerobic culture, 35-37*C, BA – <1mm diameter, grey white or colourless, dry or shiny and usually irregular outline
- Biochemical tests
- Serology: Strep serotyping, ASOT, Anti-DNAse B
- Molecular: NAAT
Regarding Streptococcus pneumoniae
- Describe 4 virulence factors that allow it cause disease
- Capsule: anti-phagocytic
- IgA protease: cleaves IgA→ bacteria is not bound to mucin
- Pneumolysin: intracellular membrane-damaging toxin that forms transmembrane pore leading to lysis
- Autolysin: breaks peptide cross-linking of peptidoglycans leading to cell lysis and release of pneumolysin. Also provokes an inflammatory response.
- Neuraminidase: release of cell wall components leading to inflammation.
- Surface protein adhesins: adherence to epithelial cells
- Describe 5 lab features of Streptococcus pneumoniae
- Culture: CBA in CO2 enriched atmosphere, 35-37*C, <1mm diameter, grey white or colourless, dry or shiny and usually irregular outline, alpha hemolytic on BA, Draughtsman appearance on BA
- Gram smear: Gram-positive cocci, capsulated, non-motile, elongated (lancet-shaped) diplococcus, may form short chains
- Biochemical identification: Catalase negative, Optochin sensitive, Bile soluble, CAMP negative, API STREP combines these biochemical tests into a strip
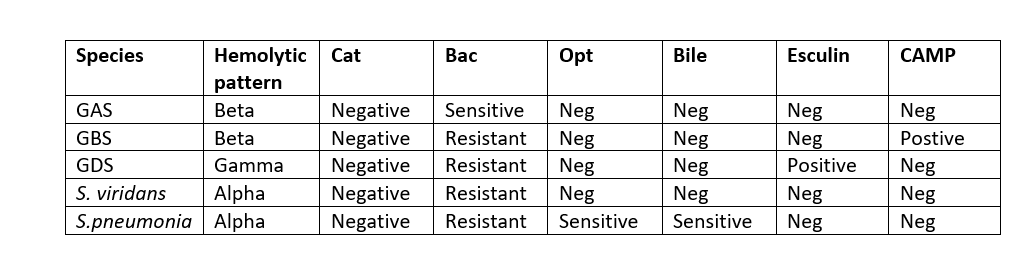
Describe the difference between Streptococcus pyogenes and Streptococcus pneumoniae regarding their lab features
| Feature | S.pyogenes | S.pneumoniae |
|---|---|---|
| Catalase test | Negative | Positive |
| Hemolysis on blood agar | Beta | Alpha |
| Bile solubility | No | Yes |
| Optochin sensitive | No | Yes |
| Bacitracin sensitive | Yes | No |
- Describe the morphological characteristics of Streptococcus viridans and give 3 examples of the organisms under this group.
- Small, gram-positive cocci usually arranged in chains or clusters
- Alpha-hemolytic, some gamma
- Facultative anaerobe
- Optochin- resistant
- Bile-insoluble
- Made up of 5 groups:
- Anginosus group: S. anginosus, S.constellatus, S.intermedius
- Mitis group: S.mitis, S.mitior, S.oralis
- Mutans group: S.mutns, S.sobrinus
- Salivarius group: S.salivarius
- Sanguinis group: S.sanguis, S,parasanguis, S.crista
Regarding S. Mutans, S. mitis, S. sanguinis, describe the following:
- Reservoir
- Oropharynx
- Biology and culture
- Viridans (green group) streptococci
- Gram positive
- Chain-like arrangement
- Facultative anaerobe
- Catalase negative
- Alpha haemolysis
- Optochinpresistant
- Bile-insolube
- Virulence factors and resistance
- Dextran
- Facilitated binding to fibrin-platelet aggregates on damaged hear tvalves
- Biofilm
- Dental plaque formation by S.mutans and S.mitis
- Dextran
- Diseases caused
- Dental caries, bacteremia: S.mutans
- Subacute bacterial endocarditis, sepsis in neutrpenic patients, pneumonia, meningitis: S.mitis– bind to platelets and fibrins
- Dental caries: S. sanguinis
- Antibiotics of choice
- Penicillin
- 3rd Gen cephalosporin (e.g. ceftriaxone)
- Macrolide (patients with penicillin allergy)
Regarding Streptococcus agalacticae, describe the following:
- Reservoir
- Lower gastrointestinal tract
- Female genital tract
- Biology and culture
- Gram positive cocci
- Chain like arrangement
- Catalase negative
- Beta haemolytic colonies on blood agar
- Lancefield group B
- Facultative anerobe
- CAMP factor (enlarges hemolysis area in a culture formed by S.aureus)
- Bacitracin resistance
- Hippurate positive
- Pyrrolidonyl arylamidase (PYR) negative
- Virulence and Resistance
- Polysaccharide capsule with sialic acid: prevents C3 deposition
- Peptidase: inactivates C5a
- Hemolysins eg. Camp factor that lyses sheep or bovine RBCs pre-treated with beta toxin of S.aureus
- Hyaluronidase
- Adhesins: surface proteins which bind human IgA
- Diseases caused
- Neonatal meningitis and pneumonia
- Neonatal sepsis
- Infections in adults:
- Puerperal infection of the mother
- Primary bacteremia
- Pneumonia
- Endocarditis
- Arthritis, osteomyelitis
- Recurrent GBS infection
- Drugs of choice
- Neonates: ampicillin+ aminoglycosides initially, then move to Penicillin-G
- Adults: Penicillin-G, add gentamycin for endocarditis
Regarding Streptococcus gallolyticus, describe the following: **
- Reservoir
- Gastrointestinal tract
- Biology and culture
- Gram positive coccus
- Chain-like arrangement
- Catalase negative
- Beta haemolytic or gamma hemolytic
- Lancefield group B
- Facultative anerobe
- Growth in bile
- Not 6.5% NaCl
- Virulence factors and Resistance
- Capsule
- Pili
- Binds to collagen allowing attachment and colonization of host cells
- Diseases caused
- Bacteremia
- Endocarditis
- Colorectal carcinoma
- Drug of choice
- Penicillin (e.g. IV penicillin G)
- 3rd generation cephalosporin (e.g. IV ceftriaxone) PLUS gentamicin
Regarding Streptococcus anginosus, describe the following: **
- Reservoir
- Oropharynx, gastrointestinal, and female genital tract
- Biology and culture
- Gram positive cocci
- Small colonies
- Catalase negative
- Beta haemolytic
- Lancefield group E, F, G and L
- Facultative anerobe
- Nonmotile
- Virulence factors and resistance
- Group F antigen
- Diseases caused
- Soft tissue infections
- Cellulitis
- Necrotizing fasciitis
- Abscesses
- Brain abscess
- Abdominal abscess
- Oropharyngeal abscess
- Septicemia
- Soft tissue infections
- Drug of choice
- Penicillin
- Ampicillin
- 3rd gen cephalosporins
Regarding Enterococcus faecalis and Enterococcus faecium, describe the following: **
- Reservoir
- Gastrointestinal tract
- Biology and culture
- Gram positive cocci
- Diplococci, chain-like arrangement (short chains)
- Alpha hemolytic and gamma hemolytic
- Lancefield group D
- Facultative anerobe
- Pyrrolidonyl arylamidase (PYR) positive
- Growth in bile (hydrolyse esculin in the presence of 40% bile salts) and 6.5% NaCl (higher resilience than streptococci)
- Diseases caused
- Leading cause of nosocomial infections
- May be triggered by GI/ GU procedures
- UTI
- Cholecystitis
- Subacute endocarditis
- Vancomycin-resisant enterococcys (VRE): nosocomial infection
- Drug of choice
- Synergistic combination of an aminoglycoside and a cell wall-active antibiotic eg. ampicillin, vancomycin
- Vancomycin (patients with penicillin allergy)
- Linezolid, tigecycline, dalfopristin, daptomycin: for Vancomycin/ ampicillin resistant Enterococci
Regarding Peptostreptococcus anaerobius and Peptostreptococcus magnus, describe the following: **
- Reservoir
- Mucocutaneous surfaces: mouth, upper respiratory tract, GIT
- Biology and virulence
- Gram positive cocci
- Chain-like arrangement
- Variable hemolysis
- Strict anerobe
- Diseases caused
- Opportunistic pathogen:
- Lung abscess
- Wound infection (soft tissue, bone)
- Brain abscess
- Puerperal sepsis
- Pelvic infection in women: endometritis, pelvic abscess
- Septicemia
- Opportunistic pathogen:
- Antibiotic of choice
- Penicillin
- Metronidazole
- Clindamycin



