Overview
Gonorrhoeal and chlamydial infection cannot be differentiated on physical examination
Gonorrhoea vs Chlamydia
| Gonorrhoea | Chlamydia | |
|---|---|---|
| Symptoms | Asymptomatic, itching or burning | Asymptomatic, itching or burning |
| Physical exam | Mucupurulent discharge, cervicitis, motion tenderness | Mucupurulent discharge, cervicitis, motion tenderness |
| Investigations | NAAT | NAAT |
| Treatment | Azithromycin or Doxicycline | Ceftriaxone + azithromycin |

Gonorrhoeal Infection
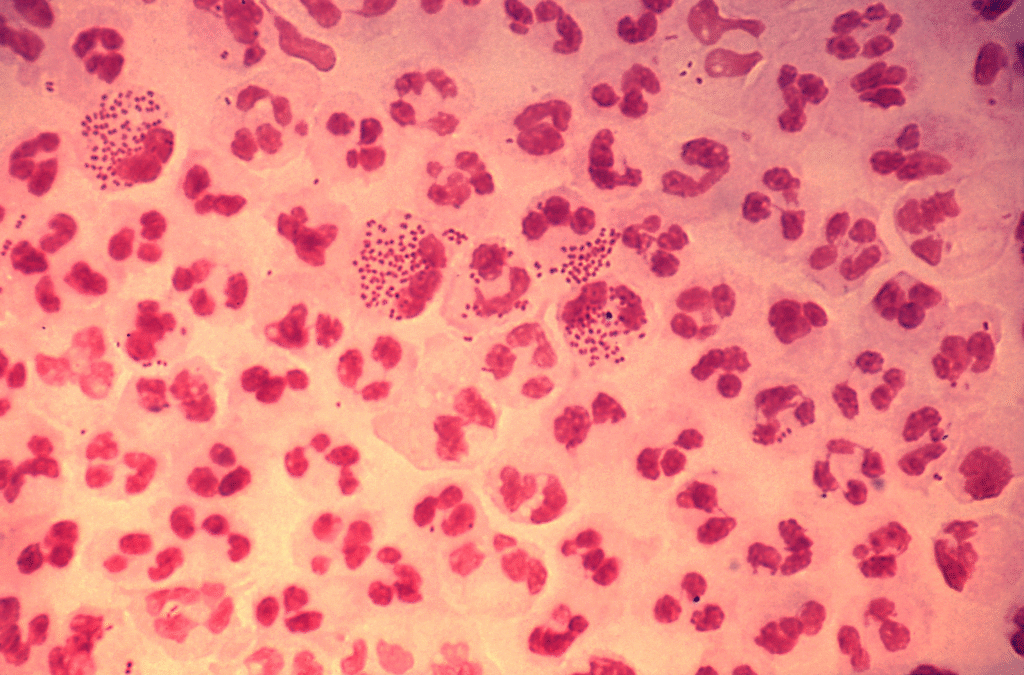
Neisseria gonorrhoea is a gram negative coccobacillus that has a propensity to infect the columnar or transitional epithelium at the endocervix and urethra. It may also infect the Bartholin and/or Skene’s glands. Most cases of gonorrheal urethritis/cervicitis are asymptomatic, especially in women. Women with risk factors should be screened regularly for infection.
- Risk factors
- < 25 years old
- Presence of other STIs e.g. HIV, syphillis, hepatitis
- History of gonorrhoeal infection
- New or multiple sex partners
- Unprotected sex
- Commercial sex work
- Drug use
- SIgns and symptoms
- Profuse, odorless, white-yellow vaginal or urethral discharge
- Dysuria
- Lower abdominal pain
- Cervicitis – Hyperemic, edematous endocervical tissue
- Bartholin cyst
- Investigation
- Nucleic Acid Amplification Test for gonorrhea and chlamydia: sample first-void urine or cervical/vaginal discharge (can also get rectal or pharyngeal swabs if there is receptive oral or pharyngeal sex respectively). NAAT is highly sensitive and specific
- Culture and sensitivity: for antimicrobial resistance
- Test for other STIs
- Treatment
- Single-dose Ceftriaxone and Azithromycin: Azithromycin is added to cover chlamydia and avoid antimicrobial resistance for Neisseria gonorrhoea)
- Refer sexual partners for treatment or Expedited partner treatment (EPT – the patient gives the prescription to the partner)
- Abstinence until the patient and sexual partners are treated
- Complications of gonorrheal infection
- DIsseminated gonococcal infection (joint pain, septic arthritis commonly in the knee, conjunctivitis)
- Pelvic inflammatory disease in women
- Acute epididymitis in males
- Ophtalmia neonataorum (bilateral conjunctivitis with purulent discharge)
Chlamydial Infection
Chlamydia trachomatis is a gram-negative ovoid non-motile obligate intracellular. It is the 2nd most common non-viral STI after trichomoniasis. All women < 25 years of age and those with high risk should be screened yearly for chlamydia.
- Risk factors
- < 25 years old
- Presence of other STIs e.g. HIV, syphillis, hepatitis
- History of gonorrhoeal infection
- New or multiple sex partners
- Unprotected sex
- Commercial sex work
- Drug use
- Signs and symptoms
- Mucopurulent discharge
- Dysuria
- Lower abdominal pain
- Cervicitis – Hyperemic, edematous endocervical tissue
- Investigations
- Nucleic Acid Amplification Test for gonorrhea and chlamydia: sample first-void urine or cervical/vaginal discharge (can also get rectal or pharyngeal swabs if there is receptive oral or pharyngeal sex respectively). NAAT is highly sensitive and specific
- Culture and sensitivity: for antimicrobial resistance
- Test for other STIs
- Treatment
- Single-dose Azithromycin can be used alone if gonorrhoea and trichomoniasis is negative
- Doxycycline 12 hourly for 7 days for anorectal chlamydia
- Refer sexual partners for treatment or Expedited partner treatment
- Abstinence until the patient and sexual partners are treated
- Complications of chlamydia
- Reactive arthritis: dysuria, monoarthritis of large joints, conjunctivitis/uveitis (can’t see, can’t pee, can’t climb a tree)
- Pelvic inflammatory disease in women + Fitz-hugh curtis syndrome
- Acute epididymitis in men
- Congenital chlamydia (bilateral conjunctivitis with water to purulent discharge 5 – 14 days after birth)

