Overview
The severity of burns can be assessed by determining the size, depth, site, inhalation injuries, and other injuries.
Size (Extent)
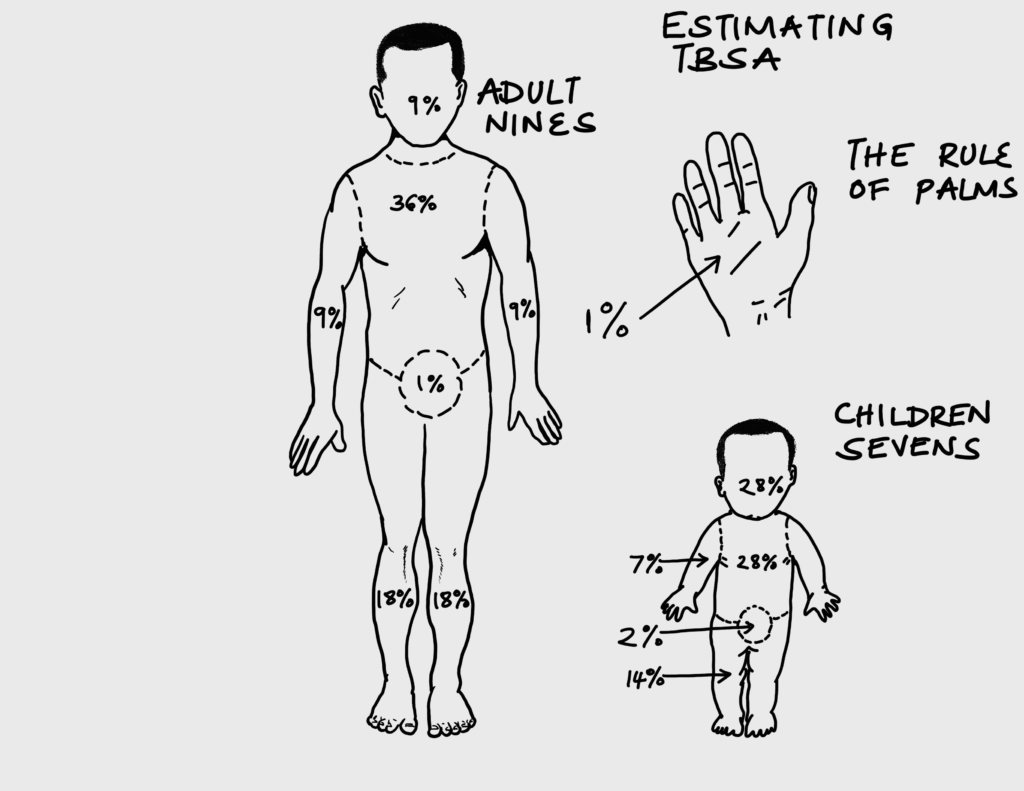
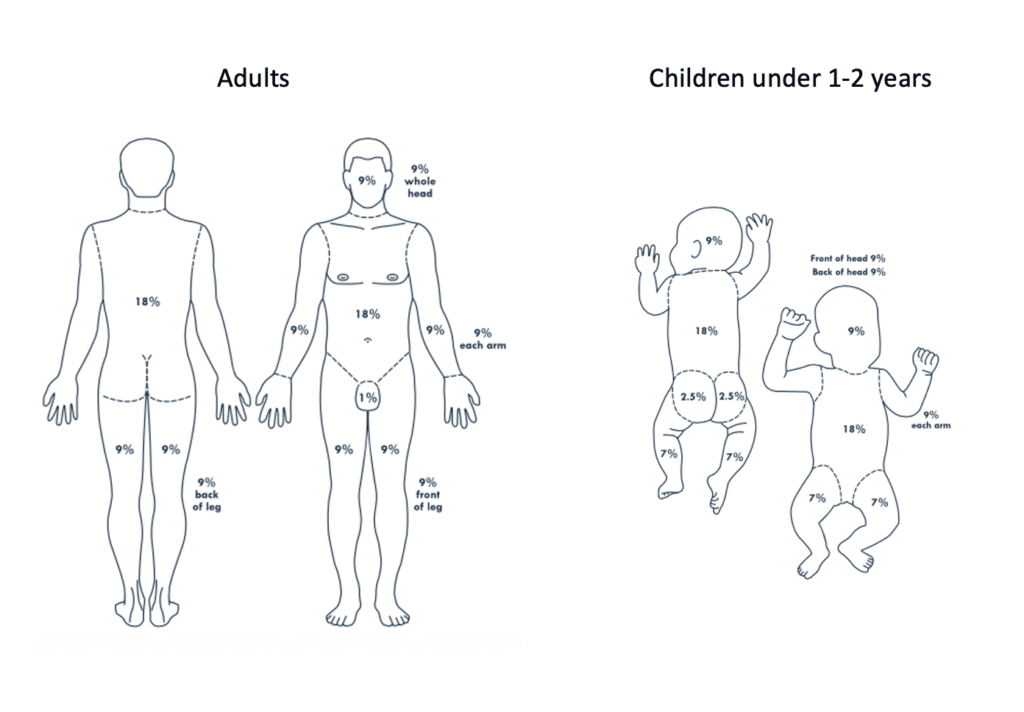
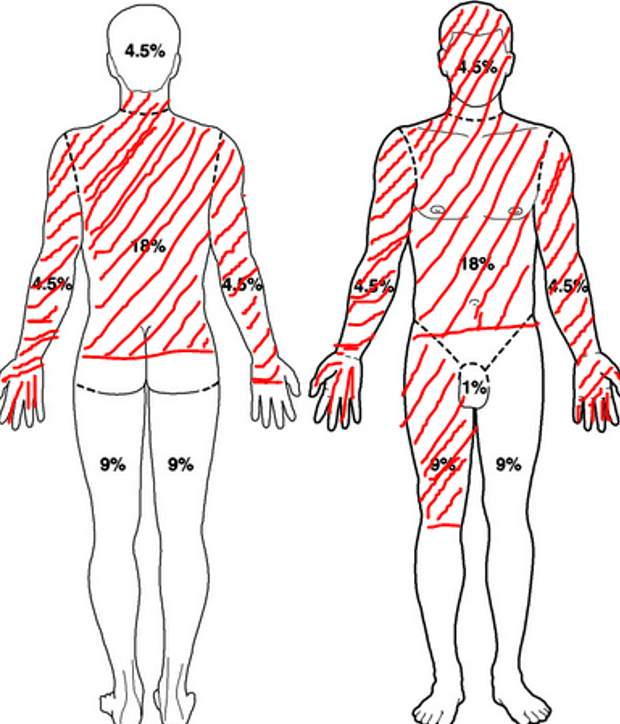
The seize of a burn is estimated as a percentage (%) of total body surface area (TBSA). Knowing the size of the burn helps to determine if formal fluid resuscitation is required. The extent is generally given as a range e.g. 5 – 7% TBSA (rather than 4.6%). It is important to estimate the size of burn as accurately as possible in younger patients.
| Method of estimating extent | Description |
|---|---|
| Rule of palms | The area of the patient’s palm with fingers closed in roughly 1% |
| Rule of 9s | Divides the body into regions each of which is 9% or multiples of 9. Differs from adults to children. |
| Lund and Browder | Calculates the %TBSA according to age. The area of burn is drawn as precisely as possible on the figure during examination and the age is used to calculate each body area. Superficial burns can be differentiated from deep burns. |
| 100% minus non-burned area | Used for extensive burns. Calculate the unburned area and subtract from 100% |
| Airway burn | Represents 10% |
Rule of 9s
| Body part | Percentage in adults | Percentage in small children |
|---|---|---|
| Entire head and neck | 9% | 18% |
| Entire left arm | 9% | 9 |
| Entire right arm | 9% | 9 |
| Chest front and back | 18% | 9 |
| Abdomen front and back | 18% | 9 |
| Entire left leg | 18% | 14 |
| Entire right leg | 18% | 14 |
| Perineum | 1% | 1 |
Depth
Factors that determine the depth of burn include the mechanism, temperature, duration of contact, and thickness of skin. Burn depth is categorised by which layer of skin is damaged. Burns that take more than 2-3 weeks to heal have a higher incidence of hypertrophic scarring and infection. Deep dermal and full thickness burns almost always need skin grafting. The more superficial the burn, the faster it heals and the less likely there will be scarring or infection.
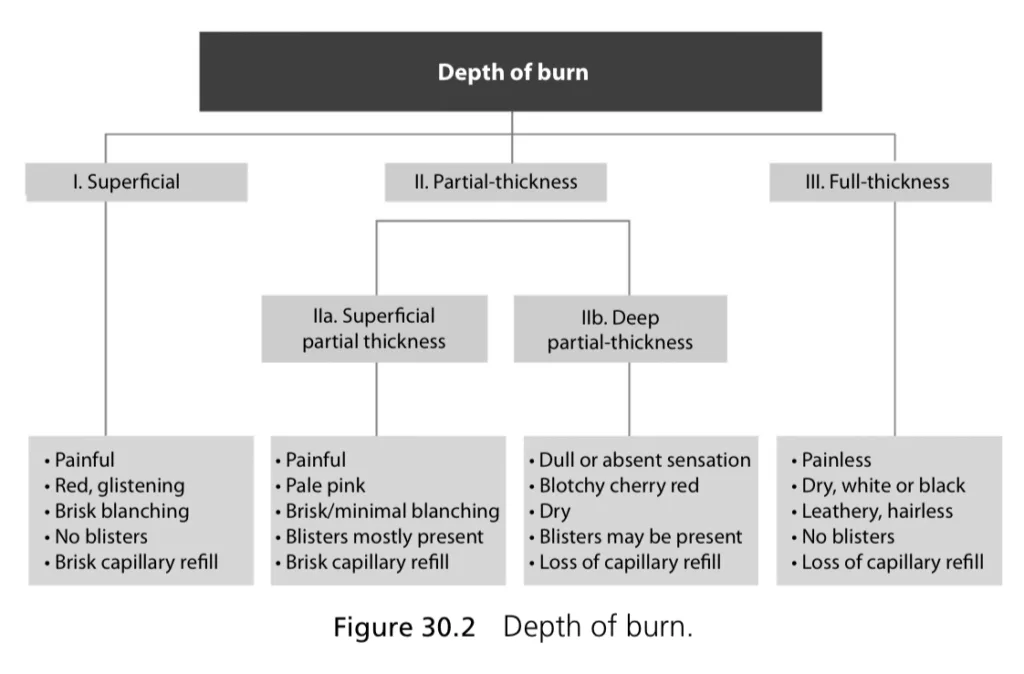
| Severity | Depth | Extent | Appearance | Skin texture | Pain | Sensation | Capilary refill | Healing |
|---|---|---|---|---|---|---|---|---|
| First-degree | Superficial (epidermal) | Epidermis | Red, glistening | Normal; blanches w/pressure | Yes | Present | Present | Yes, 1 – 2 weeks |
| Second-degree Superficial | Superficial partial-thickness (superficial dermal) | Superficial dermis | Pale pink (+/- blister) | Edematous; feels moist; minimal blanching | Yes | Present | Present | Yes, 1-2 weeks |
| Deep second-degree | Deep partial thickness (deep dermal) | Deep Reticular dermis | Pale pink | Dry | Possible | Possible | Possible | Usually 3 – 6 weeks |
| Third-degree | Full-thickness | Epidermis and dermis | Pale, white or black (+/- Eschar) | Dry and Leathery; Does not blanch with pressure | No | Absent | Absent | Very slow. No spontaneous healing |
| Fourth-degree | Subdermal | Damage to muscles, tendons, bones | Pale | Variable | No | Absent | Absent | No spontaneous healing |




Site
The site of burns determines management in terms of nature and urgency of interventions. Burn sites should be carefully recording when assessing a patient so that appropriate treatment plans can be drawn.
| Site of burn | Description |
|---|---|
| Circumferential | Swelling in circumferential burns may lead to airway obstruction in the neck, impaired ventilation (excursion) in the chest/abdomen and compartment syndrome in limbs. Surgical decompression (escharotomy or fasciotomy) is crucial |
| Hand | Function is quickly lost when oedema causes stiffness. It is important to elevate and splint the hand in the acute stage. Deep burns should be debrided and grafted. |
| Back | Skin on the back is thick and is able to heal with conservative treatment. |
| Chest | Full thickness extensive burns to the chest need an escharotomy due to reduced chest excursions |
| Axilla | Axillary skin has a high risk of contracture is healing is delayed or there is inadequate splinting or therapy. It is also difficult to nurse and dress axillary wounds. |
| Neck | Neck burns can swell and cause airway obstruction. Consider intubation. Extensive burns to the neck and anterior axillary area are prone to contracture. Positioning with arms abducted and neck extended is required. |
| Extremity (arm and leg) | Leg burns risk contracture at the knee and foot. Patient should be positioned with legs extended. Lower limb injuries need splinting and physiotherapy. |
| Toes | Burns on the toes can cause extension contractures which make wearing shoes difficult. |
| Face | Facial burns risk eye damage. Areas around the mouth are prone to contracture so keep the mouth mobile. Encourage oral stretches and splinting. Facial swelling can develop over 24 hours and cause airway obstruction. Prolonged healing can lead to deformity, ectropion, exposure keratitis, microstomia, and nasal or ear deformities. |
| Perineum | Burns around the urethra can cause urinary retention and obstetric issues due to contracture. They have a high risk of infection due to soiling |
| Eyes | Blindness can occur, especially after chemical burns. Should be irrigated well with clean water for at least 1 hour. Ointment can be used to prevent drying and referred to an ophthalmologist. |
| Joints | Deep burns over joints pose a significant risk of contractures |
Inhalational Injuries
Refers to damage to the respiratory system. Ask if there was smoke at the scene of injury. Patients with inhalation injuries should be observed for 24 hours for the development of airway problems.
Types of inhalation injury
| Type | Description |
|---|---|
| Thermal | Injures the upper airway |
| Chemical (bronchopneumonitis) | Chemical irritation from particles in smoke, which cause inflammations |
| Systemic poisoning | Tissue hypoxia from carbon monoxide poisoning, or inability to use oxygen from carbon monoxide and cyanide poisoning |
- History
- Was there smoke at the scene?
- Have they been coughing or gasping?
- Has there been decreased level of consciousness or agitation?
- Signs and symptoms that indicate respiratory compromise
- History of being trapped in a room with superheated air or smoke
- Flash burns
- Burns to the palate or nasal mucosa
- Burns to the lower face or neck
- Soot present around the mouth or nares
- Greyish or blackish sputum (Sooty sputum)
- Singed nasal hairs
- Stridor, hoarseness, dyspnea, or persistent hypoxia
- Drowsiness or confusion (due to carbon monoxide poisoning)
- Full-thickness, circumferential burns to the chest wall
Other Injuries
A rapid assessment in a structured approach needs to be carried out in all burn patients. A primary survey and secondary survey is carried out in patients with additional trauma. In multiple trauma, burn injury should be fully assessed ONLY when steps A to E have been completed. Some other injuries that can cause early death include cervical spine injury, airway obstruction, inadequate ventilation, circulatory collapse or head injury.
Classification of burns according to severity
- Minor burn injury
- Second degree burn of <15% TBSA in adults or <10% in children
- Third degree burn <2% TBSA not involving special areas (eyes, ears, face, hands, feet, perineum)
- Excludes electrical burns, inhalation injury, concurrent trauma, all poor risk patients (extremes of age, concurrent illness)
- Moderate, uncomplicated burn injury
- Second degree burn of 15-25% TBSA in adults or 10-20% in children
- Third degree burn <10% TBSA not involving special areas (eyes, ears, face, hands, feet, perineum)
- Excludes electrical burns, inhalation injury, concurrent trauma, all poor risk patients (extremes of age, concurrent illness)
- Major burn injury
- Second degree burn of >25% TBSA in adults or >20% in children
- Third degree burn >10% TBSA
- Burns involving special care areas (eyes, ears, face, hands, feet, perineum)
- All electrical burns, inhalation injury, concurrent trauma, all poor risk patients (extremes of age, concurrent illness)




