Epiglottis
Epiglottitis is an acute inflammation (commonly infectious) of the supraglottic region involving the epiglottis, vallecula, arytenoids, and aryepiglottic folds. It may also be referred to as supraglottitis as it may affect supraglottic structures mostly. The most common cause is infectious – bacterial. Viral agents do not cause epiglottitis but can allow bacterial superinfection. The most important step in treatment is securing the airway.
This is a life threatening condition that can quickly progress to asphyxia and respiratory distress. It is most commonly diagnosed in children but adults can be affected as well.
- Risk factors for developing epiglottitis
- Diabetes mellitus
- Alcohol abuse
- Hyposplenia
- Autoimmune diseases
- Immunosuppression
- Infectious causes (bacteria)
- Haemophilus influenzae – most common
- Haemophilus parainfluenzae
- Streptococcus pneumoniae
- Streptococcus pyogenes
- Staphylococcus aureus
- *Pseudomonas aeruginosa **
- Candida species*
- Mycobacterium tuberculosis*
- Non-infectious causes
- Thermal causes – smoking, burns
- Caustic ingestion
- Foreign body ingestion
- Direct extension of infection from other adjacent head and neck regions, such as dental infection, tonsillitis and skin cellulitis.
- Pathophysiology
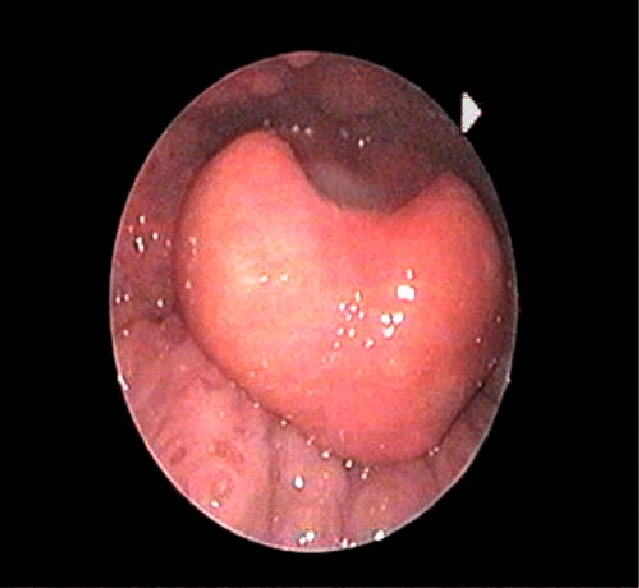
- The underlying mechanism is the resultant edema of the epiglottis and surrounding structures following inflammation. This edema causes airway obstruction.
- In children, symptoms present earlier as the epiglottic cartilage is more pliable creating a ball-valve effect where an edematous epiglottis closes over the larynx on inspiration causing symptoms.
- In adults the laryngeal cartilages have matured as such are stiffer hence can withstand the edema. Only once inflammation spreads to surrounding structures do symptoms manifest.
- Patient History
- History of previous URTI
- Signs and symptoms
- High fever
- Muffled voice – ‘Hot Potato’ voice
- Drooling
- Dysphagia
- Distress
- Anxiety
- Physical examination
- Seated in a tripod position or sniffing position
- Retractions
- Tachypnea
- Cyanosis (poor prognosis)
- Stridor – late finding
- Cervical lymphadenopathy
- Toxic appearance
- Fever
- Severe pain on gentle palpation over the larynx or hyoid bone
- Investigations
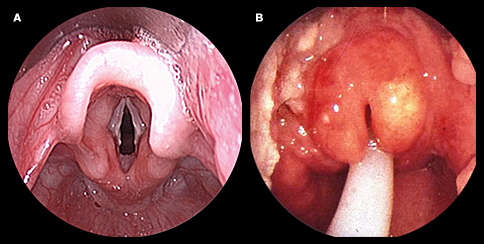
- Nasopharyngoscopy/laryngoscopy – the airway should be secured before performing this
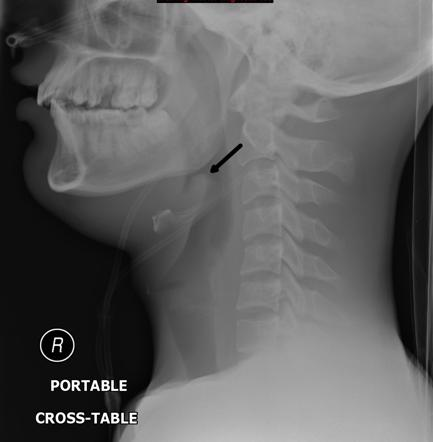
- Lateral neck radiography – the findings include swollen epiglottis (a thumb sign), thickened aryepiglottic folds, and obliteration of the vallecula (vallecula sign)
- Chest radiograph – may show pneumonia
- Bedside ultrasonography
- Microbiological studies – blood and epiglottic cultures
- Differentials
- Acute angioedema
- Airway obstruction
- Bacterial laryngotracheobronchitis
- Caustic ingestion
- Thermal injury from liquids or hot air (burns)
- Foreign body aspiration
- Laryngeal diphtheria
- Laryngitis
- Laryngotracheal bronchopneumonitis
- Peritonsillar abscess
- Retropharyngeal abscess
- Sepsis
- Treatment
- The most important aspect of management is managing the airway by: Intubation, Tracheostomy, Cricothyrotomy Ideally, the airway should be secured in the operating room where a laryngoscope is used to directly view the larynx and swabs for culture can be collected.
- Once the airway is secure initiate:
- IV steroids – to reduce the swelling
- IV antibiotics – at first empirical (ceftriaxone, cefuroxime) once culture and sensitivity results are back a more fitting regimen can be started.
- Analgesia
- Oxygen supplementation
- Complications
- Cervical adenitis
- Empyema
- Epiglottic abscess
- Meningitis
- Pneumonia
- Pneumothorax
- Sepsis
- Septic arthritis
- Septic shock
- Vocal cord granuloma
- Ludwig angina-type submental infection
NOTE:
For patients who present in severe distress i.e respiratory distress, airway compromise on examination, stridor, inability to swallow, drooling, sitting erect, and deterioration within 8-12 hours should not undergo any tests before securing the airway (intubation, tracheostomy etc)
Do not examine the throat with a tongue blade or a flexible laryngoscope, as it may result in the loss of the airway.