Ectopic Pregnancy
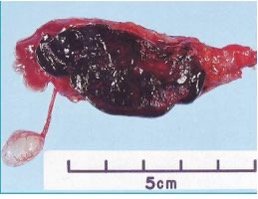
An ectopic pregnancy occurs when the embryo implants somewhere other than the endometrial cavity (95% in the fallopian tubes of which 70% occur in the tubal ampulla). A clinical triad of abdominal pain, vaginal bleeding and a pelvic mass are seen in ectopic pregnancy. For any woman of reproductive age who presents with pelvic pain and a positive pregnancy test, ectopic pregnancy should be suspected until proven otherwise. The main differential is miscarriage, although any other condition causing early pregnancy bleeding can be suspected. A b-hCG > 3500 IU/ml and no intrauterine pregnancy visualized on transvaginal ultrasound carries a high possibility for ectopic pregnancy. Treatment can be expectant, medical, or surgical depending on clinical status. Patients with ectopic pregnancy should be followed up with serial ultrasounds and B-hCG levels until undetectable the levels are undetectable.
Ectopic pregnancy occurs in 2% of all pregnancies. Following an ectopic pregnancy, 70% of women can go on to have an intrauterine pregnancy. The risk of recurrence is around 10 – 20%, hence the need for early scan in subsequent pregnancy to confirm the location.
- Sites of ectopic implantation
- Fallopian tubes (95%)
- Ampulla (70%)
- Isthmus (25%, most common site of rupture)
- Fimrbial (17%)
- Interstitial (2%, earliest to rupture)
- Other sites (<5%)
- Cervix
- Ovary (< 1%, historically used Spielberg criteria – 1878)
- Caesarean section scar
- Cornua or cornual interstitium
- Extrauterine (peritoneal cavity)
- Heterotopic (ectopic pregnancy + intrauterine pregnancy)
- Fallopian tubes (95%)
- Risk factors for ectopic pregnancy
- Pelvic inflammatory disease: especially Chlamydia trachomatis – tubal scarring, loss of cilia and hydrosalpinx
- Previous ectopic pregnancy: due to peritubal adhesions and strictures ****
- History of pelvic or tubal surgery: due to peritubal adhesions and strictures causing mechanical obstruction
- Smoking: causes ciliary dysfunction and reduced tubal motility
- Recurrent pregnancy loss: congenital or acquired (Asherman’s) abnormalities may impair embryo migration.
- Progesterone-releasing IUD (Progestasert) and Progesterone only pill: reduce tubal motility and ciliary action. Progesterone only pills are not as effective at suppressing ovulation as combined oral contraceptive pills. They also suppress endometrial proliferation making implantation in the uterus less likely.
- Assisted conception
- Endometriosis
- Signs and symptoms of ectopic pregnancy
- Amenorrhea and vaginal bleeding
- Lower abdominal pain/cramping
- Adnexal tenderness and/or mass
- Occasionally cervical motion tenderness
- Early signs of pregnancy (nausea, vomiting, breast tenderness)
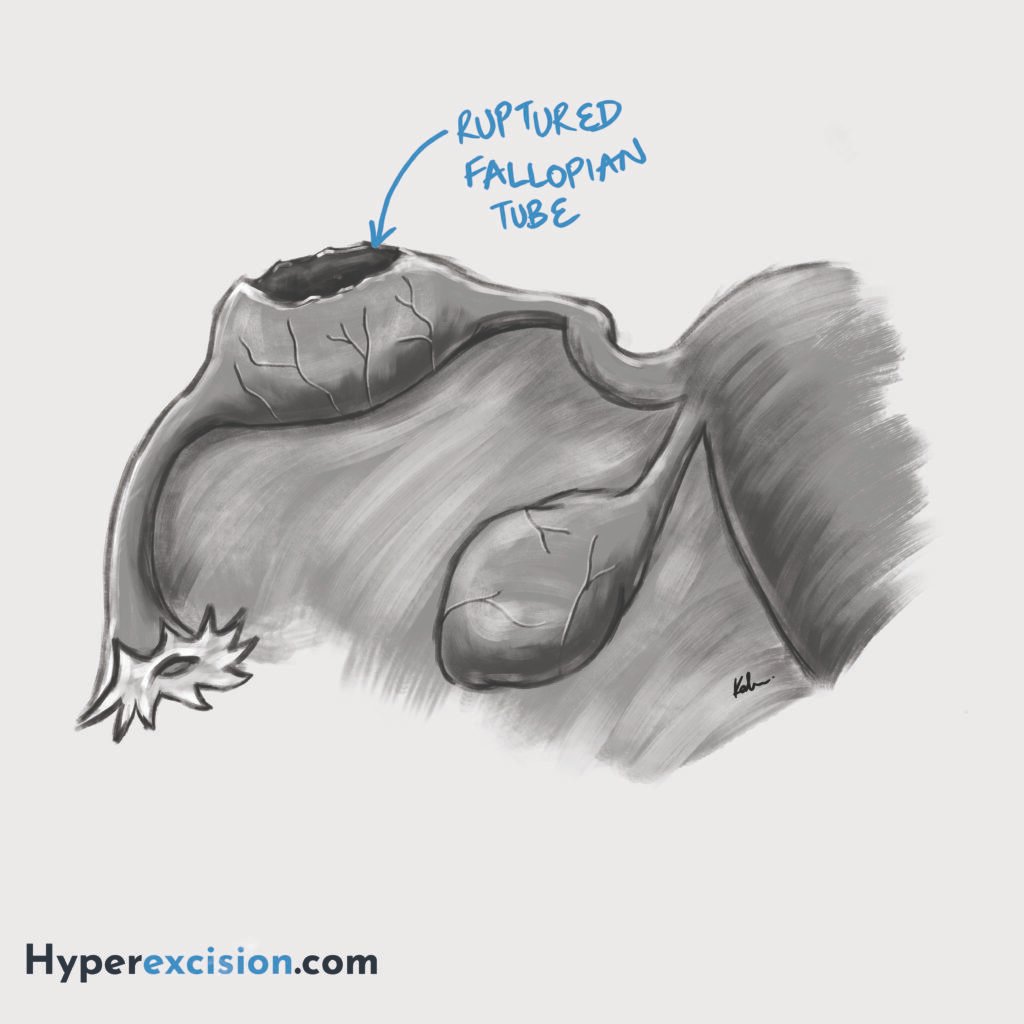
- Signs and symptoms of ruptured ectopic pregnancy
- Vaginal bleeding
- Unilateral severe lower abdominal pain
- Guarding and rigidity (peritonitis)
- Hypovolemic shock (tachycardia, hypotension)
- Blood on paracentesis and culdocentesis: if the concern for intra-abdominal bleeding is high and ultrasound cannot be performed
- Investigations
- Cervical os on speculum exam: variable
- Qualitative B-hCG: positive
- Quantitative B-hCG: Usually ow for the gestational age. Repeat 48 hours later (should double every 48 hours in normal pregnancy).
- < 5 mIU/mL excludes ectopic
- 1500 IU shoudl visualize intrauterine or ectopic pregnancy
- Rise > 66% indicates intrautterine pregnancy
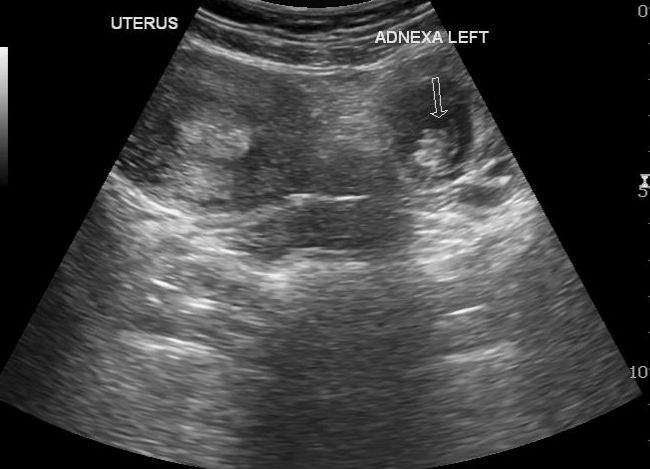
- Transvaginal ultrasound (TVUS):
- No intrauterine pregnancy detected (in the setting of B-hCG > 3500 IU/ml)
- “Ring of fire” sign in the adnexa on colour doppler (peripheral hyperechoic ring surrounding an adnexal mass on ultrasound). Represents hypervascularity of trophoblastic tissue. This sign can also be seen with a corpus luteum cyst.
- What does the treatment of ectopic pregnancy depend on?
- Size of the embryo
- B-hCG levels
- Status of the patient (hemodynamic stability and comorbidities)
- Desire for fertility preservation
- Treatment of ectopic pregnancy
- Methotrexate: B-hCG <5000 mIU/mL, size <3.5cm and hemodynamically stable
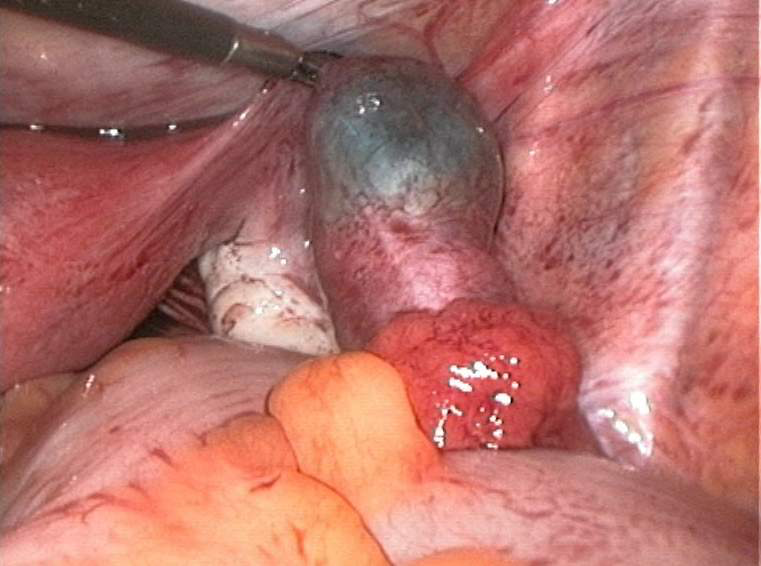
- Laparotomy or Laparoscopy
- Unilateral salpingectomy: for severely damaged or ruptured tubes, healthy contralateral tube, complete family, or reccurent ectopic or size > 5cm
- Unilateral salpingotomy: Increases the risk of residual trophoblast and bleeding. Suitable for those with contralateral tube disease and desire for future pregnancy
- Follow-up with repeat B-hCG
- RhoGAM (Anti-D) for rhesus negative mother (if needed)
- Indications for surgical management
- B-hCG >5,000 mIU/mL or
- Hemodynamically unstable or
- Ongoing rupture/intraperitoneal bleeding or
- Contraindication to Methotrexate (MTX)
Weight-based methotrexate for ectopic pregnancy
A standard regimen is a single doe of 50g/m2 body surface area. Patient who receive methotrexxate have serial B-hCG levels monitored. Additional doses may be given if levels fail to decline. If
- Indications for medical management of ectopic pregnancies (methotrexate)
- Hemodynamically stable
- Unruptured mass ≤ 3.5 cm
- B-hCG < 5,000 mIU/mL
- Gestational age < 5 weeks
- No fetal cardiac activity
- No contraindications to methotrexate
- Absolute contraindications to methotrexate
- Intrauterine pregnancy
- immunodeficiency
- Moderate to severe anemia, leukopenia, or thrombocytopenia
- Sensitivity to MTX
- Active pulmonary disease, hepatic dysfunction or renal dysfunction
- Active PUD
- Breastfeeding
- Ruptured ectopic pregnancy
- Hemodynamically unstable patient
- Inability to participate in follow-up
- Relative contraindications to methotrexate
- Embryonic cardiac activity detected by transvaginal US
- High initial hCG concentration (> 5000)
- Ectopic pregnancy > 4cm in size as imaged by transvaginal ultrasound
- Refusal to accept blood transfusion
- Refusal or lack of follow-up care



