Overview
Diabetic retinopathy is the breakdown of retinal vasculature due to persistent hyperglycemia. It usually occurs in patients with poorly controlled diabetes. All patients with a new diagnosis of T2DM should be referred to an ophthalmologist for baseline evaluation. The best treatment for diabetic retinopathy is primary prevention (healthy diet, exercise, and anti-hyperglycemic medications)
Diabetes is the leading cause of new-onset blindness in adults aged 20-65 years. It affects up to 80% of patients who have had diabetes for 10 years or more. 40% of patients with T2DM will have retinal changes consistent with diabetic retinopathy. 20% of patients will have visual changes as the presenting symptoms of T2DM. Retinopathy begins to present in patients with T1DM from about 3 years after the diagnosis.
- Apart from diabetic retinopathy, what other ocular pathologies are patients with diabetes at risk of?
- Cataracts (early age)
- Thrombosis of the retinal artery
- Glaucoma (Neovascular Glaucoma)
- Changing refractive errors (due to lens tumescence)
- Corneal epithelial defects (can have neurotrophic ulcers)
- Basic pathophysiology of diabetic retinopathy
- Pericyte degeneration
- Pericytes are cells that wrap capillary vessels in the eye
- Their degeneration leads to the formation of microaneurysms which then rupture leading to haemorrhages
- Pericyte degeneration
- Management of patients with diabetes retinopathy
- Monitor Blood Pressure and Lipids
- HbA1C between 6-7% is ideal for long-term monitoring
- Encourage the patient to stop smoking (since smoking reduces retinal oxygenation thus up-regulating VEGF)
- Avoid prescribing Thiazolidinediones (e.g. Rosiglitazone) for T2DM
- When should a patient with Diabetes be referred to an ophthalmologist?
- ALL New diagnosis of T2DM (for initial examination) then q1year thereafter
- ALL T1DM patients 5 years after onset or roughly around puberty. Then q1year thereafter
- ALL diabetics with acute change in vision
- ALL diabetics with a sudden drop in acuity
Classification of Diabetic Retinopathy
There are two types of diabetic retinopathy; proliferative and non-proliferative.
Non-proliferative diabetic retinopathy (NPDR)
- This is the most common form of diabetic retinopathy (95%)
- It is so common in diabetics that it is often called “background retinopathy”
- Fundoscopy findings
- Microaneurysms (earliest sign)
- “Dot-and-blot haemorrhages”: damaged capillaries→ leakage of fluid seen as small dots of blood in the eye
- Cotton-wool spots: nerve infarctions due to the occlusion of precapillary arterioles which are visualised as bright fluffy spots on the retina
- Also seen in hypertension
- Hard exudates and macular oedema
- Macular swelling
- Yellow exudates of fatty lipids
- This can lead to blindness
 Background Retinopathy. Early diabetic changes are seen in the eye.
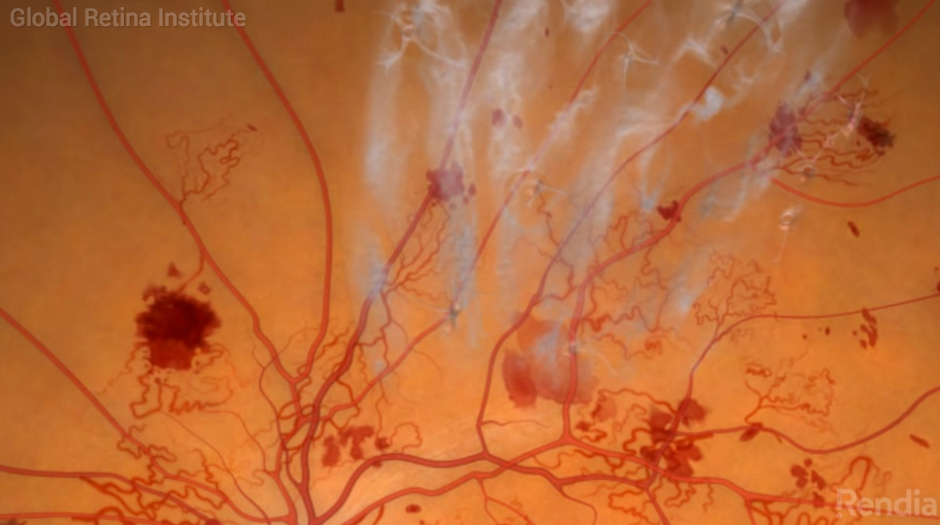
Background Retinopathy. Early diabetic changes are seen in the eye.  Venous loops. An advanced feature of NPDR
Venous loops. An advanced feature of NPDR
Proliferative diabetic retinopathy (most advanced stage)
- Fundoscopy
- Vessel proliferation: Retinal ischemia leads to new vessel growth. The abnormal vessels are friable and grow on the surface of the retina
- Can lead to retinal detachment
- Can cause macular edema resulting in blindness
- Vessel proliferation: Retinal ischemia leads to new vessel growth. The abnormal vessels are friable and grow on the surface of the retina
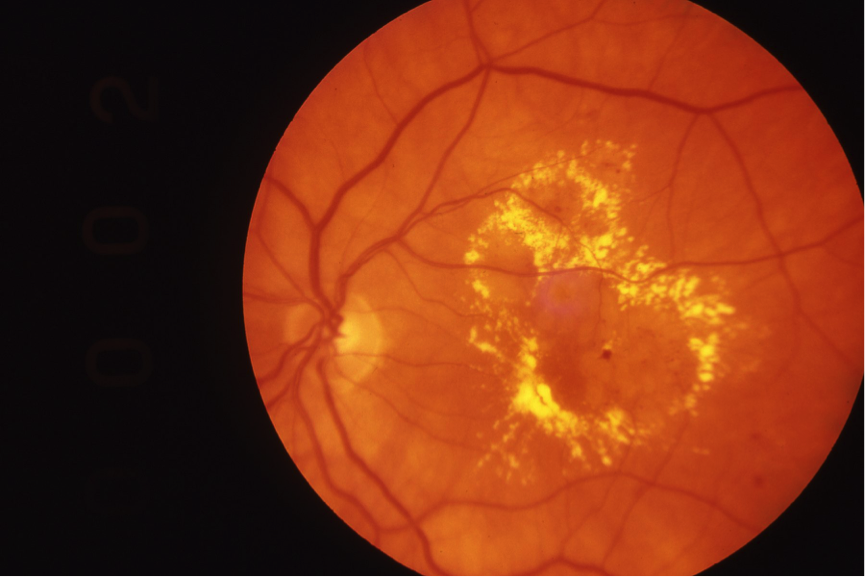
Diabetic Maculopathy
Diabetic maculopathy is symptomatic since the macula is affected (unlike background retinopathy). It is considered an advanced form of non-proliferative diabetic retinopathy, but may not progress into proliferative diabetic retinopathy.
- Signs and symptoms
- Loss of visual acuity
- Scotoma like black spots in central vision
- Blurred vision
- Image distortion (especially relative to other eyes
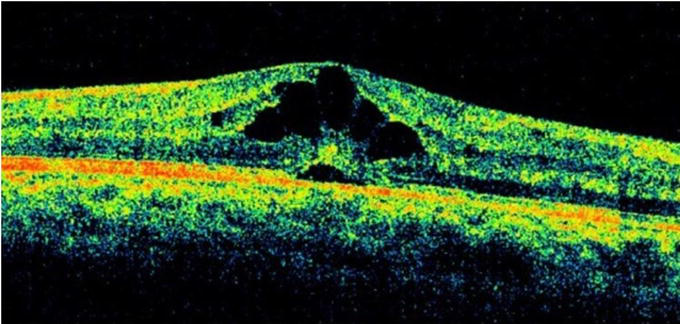
- Investigations
- Ophthalmoscopy
- Hard exudates
- Hemorrhages
- Optical Coherence tomography
- Macula Oedema
- Fluorescein angiography
- Ophthalmoscopy
- Treatment Primary prevention is most important
- Laser photocoagulation
- Intravitreal VEGF
- Vitrectomy
- Intravitreal corticosteroids (Dexamethasone, Fluocetonide)
Proliferative Diabetic Retinopathy
Proliferative Diabetic Retinopathy is the most advanced stage of diabetic retinopathy. In this type, new vessels begin to form since the native vessels have been damaged. As the new vessels continue to proliferate, they progress to the anterior structures and block the angle of the eye (which could lead to glaucoma). Dead vessels can also undergo fibrosis and act as a point of traction leading to retinal detachment.
- Signs and symptoms
- Blurry vision (due to vitreous hemorrhage or macular edema)
- Floaters
- Difficulty with nighttime vision
- Symptoms of retinal detachment
- Photopsia
- Floaters
- Visual field deficit
- Symptoms of glaucoma
- Pain
- Photophobia
- Neovascularization of iris
- Conjunctival injection
- Investigations
- Ophthalmoscopy
- Neovascularization from the optic disk or major vessels
- Hemorrhaging (microaneurysm, dot-blot)
- Vitreous haemorrhage
- Ocular Tonometry: To measure IOP if neovascular glacuoma is a concern
- Fluorescein angiography
- Ophthalmoscopy
- Treatment
- Panretinal photocoagulation (PRP)
- Intravitreal VEGF inhibitors (e.g. ranibizumab)
- Vitrectomy (to remove bleeding or debris)
- Intravitreal corticosteroids (Dexamethasone, Fluocetonide)