Table Of Contents
Colorectal cancer
Colorectal cancer is the third most common cancer and the second most common cause of death from cancer. The incidence is increasing in Sub-Saharan Africa and in younger patients. Rectal cancer is as common as colon cancer. Screening for colorectal cancer is offered every 2 years to all men and women aged 50 – 74 years, beginning with a FOBT, then a colonoscopy.
80% of colorectal cancers are sporadic.
Syndromes associated with hereditary colorectal cancer
| Syndrome | Description |
|---|---|
| Familial adenomatous polyposis (FAP, 1%) | Autosomal dominant condition caused by mutation in the APC gene. Characterized by hundreds to thousands of adenomatous polyps in the colon which begin to develop shortly after puberty. 100% of patients with FAP develop colorectal cancer by 50 years old. Total proctocolectomy is the treatment once polyps begin to develop |
| Attenuated FAP | Polyps appear later in life and cancer develops in about 50% of patients in middle age. |
| Hereditary non-polyposis colon cancer (1-3%, HNPCC /Lynch Syndrome) | Autosomal dominant condition caused by mutation of DNA mismatch repair genes (MLH1 or MSH2). 70% of individuals develop colon cancer, commonly right-sided. Diagnosis is made using the Amsterdam criteria. |
| Familial colorectal cancer (10-15%) | A family history of colon cancer carries a 12% risk of developing colon cancer with one first-degree relative and 35% with two or more (6% in patients without a family history). |
| Juvenile polyposis syndrome (JPS) | Autosomal dominant syndrome characterized by multiple harmatomatous polyps throughout the gastrointestinal tract. Has an increased risk of colorectal and gastric cancer. 30-50% of patients develop colon cancer by 45 years. |
Duke’s staging of colorectal cancer
| Duke stage | Description |
|---|---|
| A | Invasion not breaching the muscularis propria i.e. tumor confined to mucosa and submucosa |
| B | Local invasion breaching the muscularis propria but no regional lymph node involvement |
| C | Regional lymph node metastases |
| D | Distant metastases |
- Risk factors for colon cancer
- Older age (90% occur above 50 years old)
- High fat diet
- Low-fiber diet (high fiber diet is protective)
- Long-standing inflammatory bowel disease (both Crohn’s and ulcerative colitis)
- Hereditary colorectal cancer syndromes
- Alcohol and smoking
- Obesity
- Pathophysiology
- Colon cancers arise through the adenoma-carcinoma sequence
- APC/B-catenin pathway (80%): activated in the classic adenoma carcinoma sequence. Loss of APC function causes b-catenin to accumulate and activate transcription (MYC, Cyclin D1). Also associated with mutation in KRAS, SMAD2, SMAD4, TP53, methylation of CpG islands (silencing of tumor suppressor genes), and increased telomerase expression
- Microsatellite instability (MSI) pathway: associated with defects in mismatch repair and accumulation of mutations in microsatellite repeat regions of the genome. Genes involve include MLH1, MSH2, MSH6, PMS1, PMS2. Common in sessile serrated lesions and frequently causes right-sided cancer
- Both pathways involve multiple genetic alterations occuring over a period of time, which resultin in an invasive tumor.
- Patient history
- Older age
- Family history of colon cancer
- Inflammatory bowel disease
- High-fat diet
- Familial polyp disease
- Signs and symptoms
- Asymptomatic until advanced stages
- Rectal bleeding
- Melaena
- Hematochezia
- Maroon coloured stool
- Change in bowel habits
- Diarrhoea (common with right sided lesions)
- Constipation
- Tenesmus
- Obstruction
- Right-sided lesions commonly present with anaemia and melaena
- Left-sided regions are more likely to present with hematochezia and obstruct (left colon is smaller in caliber and has a firmer stool consistency)
- Fatigue
- Anorexia
- Investigations
- Fecal occult blood testing (FOBT): has a positive predictive value (PPV) of 5 – 15%. The PPV for an adenoma is 30 – 45%.
- Colonoscopy with biopsy: best initial test for patients with an abnormal fecal occult blood testing. Screening reduces mortality by 16%.
- 5 out of 10 patients have anormal exam
- 4 out of 10 patients have polyps that may be removed due to their premalignant potential
- 1 out of 10 patients has cancer
- Treatment
- Resection
- Chemotherapy
Location of cancer and procedure
| Location | Procedure |
|---|---|
| Right sided colon | Right colectomy with ligation of the ileocolic artery |
| Transverse colon | Transverse colectomy with ligation of the IMA |
| Descending colon | Left colectomy with ligation of the IMA |
| Sigmoid colon | Left colectomy with ligation of IMA |
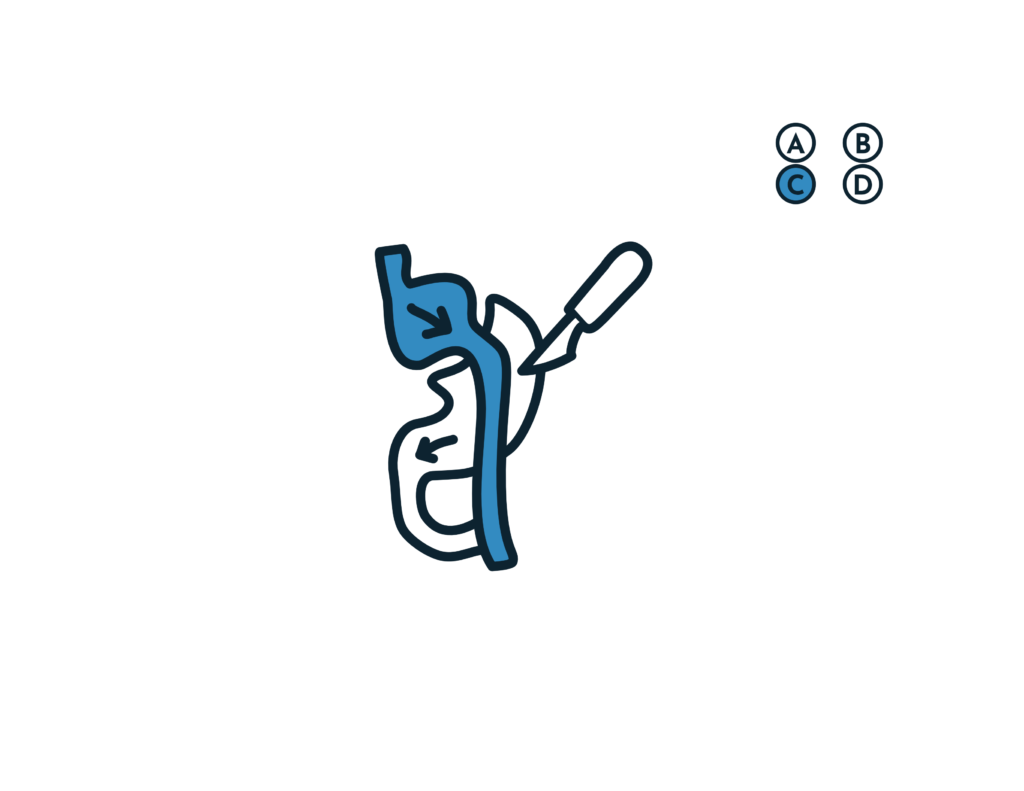
| Rectum > 3 cm from the dentate line | Low anterior resection (LAR) |
| Rectum < 3 cm from the dentate line | Abdominoperineal resection (APR) |