Chorioamnionitis
Chorioamnionitis is an ascending bacterial infection with resultant inflammation of any combinaito nof the amniotic fluid, placenta, fetus, fetal membranes or decidua. It is a common cause of maternal fever, and major complication of PPROM and prolonged ROM. The infection is typically polymicrobial (GBS used to be the most common isolate but currently GNs are more common isolates since they aren’t covered by penicillin) and can affect intact or ruptured membranes. Diagnosis is clinical – risk factors + Fever + two other symptoms (including abdominal tenderness). The goal of treatment is to reduce maternal and fetal complications, especially neonatal sepsis. Once chorioamnionitis is diagnosed the mother is treated with IV antibiotics. Labor should be induced to expedite deliver.
Diagnostic criteria for chorioamnionitis
| Diagnosis of Choriomnionitis is made if there is maternal fever > 38 C with 2 or more of the following. |
|---|
| Lower abdominal (uterine) pain and tenderness |
| Foul smelling PV discharge |
| Maternal tachycardia > 100 bpm |
| Increased WBC >15 |
| Fetal tachycardia > 160 bpm |
| CRP > 40 |
- Etiology
- Polymicrobial – commonly gram negative rods, group B streptococcus
- Typically an ascending infection from the vaginal flora into the sterile amniotic cavity
- Can occur after invasive procedure e.g. amniocentesis or chorionic villus sampling
- Can occur by hematogenous route secondary to maternal sepsis
- Risk factors for chorioamnionitis
- Prolonged ROM
- Prolonged labor
- PPROM and prematurity
- Multiple digital exams with membrane rupture (use sterile gloves, not worth it to do more than an hour)
- Presence of certain genital tract pathogens (e.g. group B streptococcal infection and sexually transmitted infections)
- Epidural anesthesia (controversial…)
- Cervical insufficiency (less space between vagina and membranes)
- EtOH and tobacco use
- Low parity
- Use of internal uterine and fetal monitors
- Meconium-stained amniotic fluid
- Signs and symptoms
- Maternal fever (> 38 C)
- Significant maternal tachycardia (HR > 120)
- Fetal tachycardia (FHR 160-180)
- Uterine tenderness
- Purulent/foul smelling amniotic fluid discharge
- Maternal leukocytosis
- Differentials
- Epidural-associated fever
- Urinary tract infection
- Appendicitis
- Influenza
- Pneumonia
- Malaria
- Investigations
- Amniocentesis: Traditionally the gold standard, to analyze and culture the amniotic fluid (takes 3 days). Profile similar to CSF analysis in Bacterial meningitis.
- Glucose: Low
- WBC: high
- Protein: high
- Gram stain: positive
- Esterase: positive
- IL-6: positive
- Culture: positive
- Urinalysis and urine culture: rule out urinary tract infection
- Amniocentesis: Traditionally the gold standard, to analyze and culture the amniotic fluid (takes 3 days). Profile similar to CSF analysis in Bacterial meningitis.
- Treatment of chorioamnionitis
- Fetal monitoring
- Intrapartum IV antibiotics until delivery: decreases the rate of neonatal bacteremia, pneumonia and sepsis. Also decreases maternal febrile morbidity and the length of hospital stay.
- Ampicillin/amoxicillin + gentamicin + metronidazole (can be given in late pregnancy when benefits outweight the risk)
- Add clindamycin if performing a caesarean delivery or penicillin allergy
- Antipyretics (paracetamol): reduces fetal HR and distress, and reduces the risk of encephalitis)
- Expedite delivery
- Monitor and ensure good progress of labour (prolonged labour can contribute towards intra-amniotic infection)
- Augment protracted labour
- Mode of delivery based on obstetric indications. Chorioamnionitis is rarely an indication for caesarean delivery
- Notify paediatrics
Complications of Chorioamnionitis
- Maternal complications of chorioamnionitis
- Increased risk of C-section
- Endometritis
- Wound infection
- Pelvic abscess
- Bacteremia
- Postpartum hemorrhage
- Fetal complications of chorioamnionitis
- Fetal Inflammatory response syndrome
- Chronic lung disease
- Multi-organ damage
- Brain damage
- Preterm birth
- Perinatal death
- Neonatal infection and sepsis (early onset neonatal sepsis)
- Respiratory distress due to pneumonia
- Cerebral palsy (due to decompensation of brain tissue)
- Intraventricular hemorrhage
- Necrotizing enterocolitis
- Fetal Inflammatory response syndrome
Diagnosis of Intra-amniotic infection
- Diagnosis of intraamniotic infection can be made by using clinical criteria, or objectively by culture, gram stain, biochemical analysis or histology
- For most women in labor the initial diagnosis will be made using clinical criteria
- Consider the three categories of intraamniotic infection below:
- Isolated maternal fever
- Defined as either a single oral temperature of 39°C or greater, or an oral temperature of 38–38.9°C that persists when the temperature is repeated after 30 minutes
- Markedly elevated maternal temperatures are most likely due to infection, while transient lower temperature elevations may be due to infection, or other factors such as dehydration, epidural analgesia
- Suspected intraamniotic infection (Based on clinical criteria)
- Maternal intrapartum fever AND two or more of:
- Maternal leukocytosis (>15*10^9/l)
- Maternal tachycardia (>100bpm)
- Fetal tachycardia (>160bpm)
- Purulent/ offensive cervical discharge
- Uterine tenderness
- CRP (>40)
- Confirmed intraamniotic infection (Based on laboratory studies)
- Positive amniotic fluid result – gram stain, glucose level, culture results consistent with infection
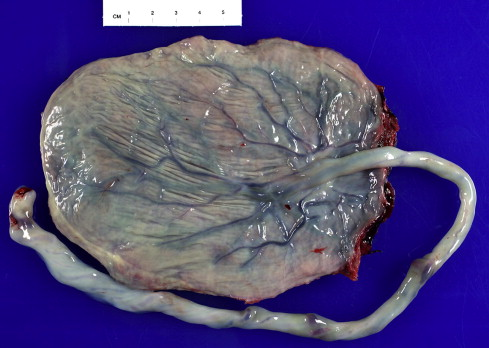
- Placental pathology demonstrating histologic evidence of placental infection and inflammation
- Isolated maternal fever

