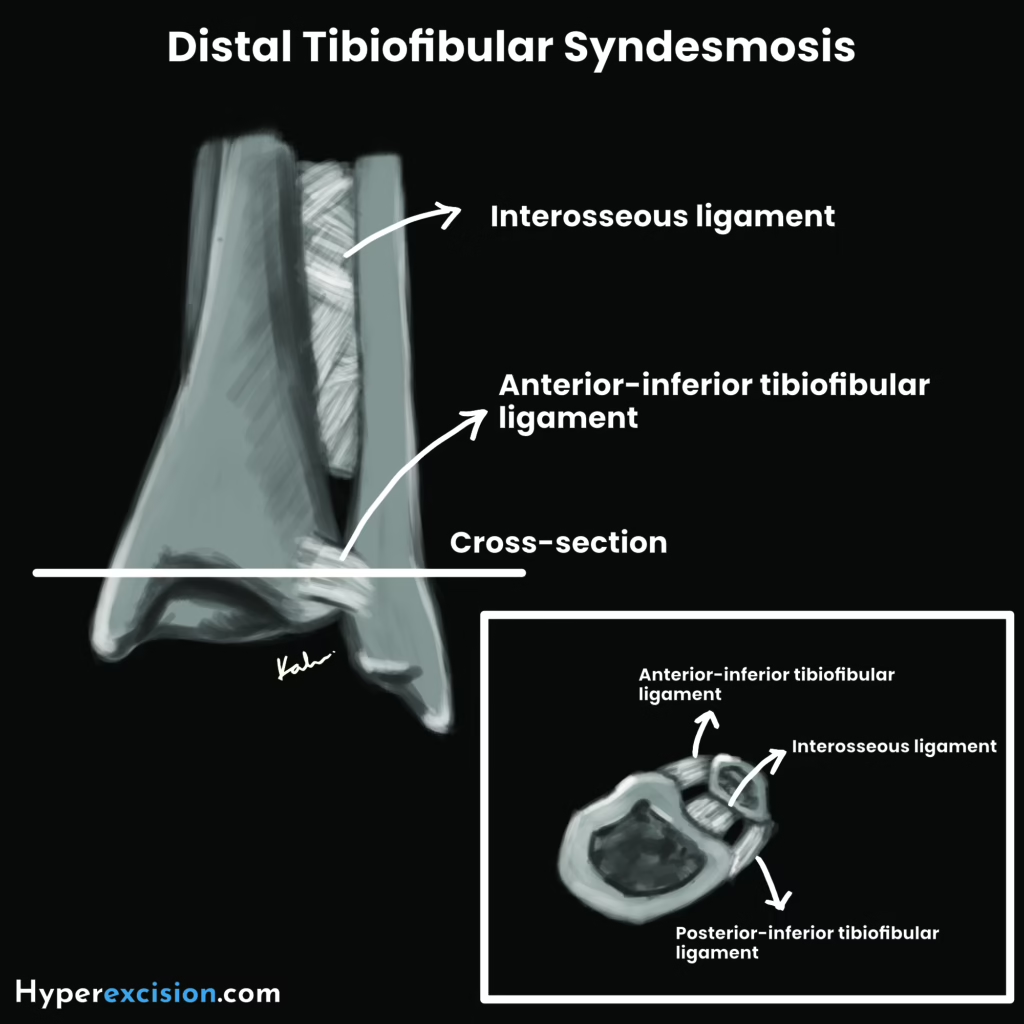
Anatomy
The ankle mortise is comprised of the socket (distal ends of the tibia and fibula) and the tenon (upward projecting talus). It is a hinge joint that is supported by a fibrous capsule, 3 bands of lateral ligaments and the medial deltoid ligament. The syndesmotic ligaments also contribute to stability by resisting axial, rotational and translational forces between the tibia and fibula.
Ligaments around the ankle joint
| Ligaments | Description |
|---|---|
| Fibrous capsule | Surrounds the joint and is attached to the articular margins |
| Lateral ligaments | Consists of three bands – anterior-talofibular ligament (ATFL), calcaneofibular ligament (CFL) and posterior talofibular ligament (PTFL) |
| Medial (deltoid) ligament | Strong triangular ligament with a superficial layer formed by tibiocalcaneal, tibionavicular, posterior superficial tiboitalar and tibiospring ligament, and a deep layer formed by anterior tibiotalar and posterior deep tibiotalar ligament |
| Distal tibiofibular syndesmosis | Formed by the anterior inferior tibiofibular ligament (AITFL), posterior inferiot tibiofibular ligament (PITFL), transverse tibiofibular ligament and interosseous ligament |
Malleolar fracture
Malleolar fractures are common, generally occurring following a twisting, rotating, or rolling motion (from standing, tripping or falling) on the ankle causing the tallus to tilt/rotate forcibly on the socket of the mortise. It is also associated with high-energy injury. They can be classified into isolated malleous fracture (70%), bimalleolar fracture (20%) or trimalleolar fracture (7%).
Only 15% of ankle injuries are fractures. Patients often present with an ankle sprain rather than a malleolar fracture.
Mechanism of injury – Lague Hansen guides the method of reduction and suggests associated ligament injuries
| Mechanism | Fracture pattern | Corresponding Weber |
|---|---|---|
| Supination-External Rotation (SER) | Pull off medial malleolus. Oblique/vertical push off fibular fracture | Weber B |
| Pronation-External Rotation (PER) | Pull-off medial malleolus. High spiral fibula fracture +/- posterior malleolus | Weber C |
| Supination-Adduction (SA) | Transverse fibular fracture due to avulsion or pull-off. Vertical tibial fracture because of push-off. | Weber A |
| Pronation-Abduction (PA) | Medial malleolus + comminuted fibula | |
| Axial load | Posterior malleolus or plafond fracture |
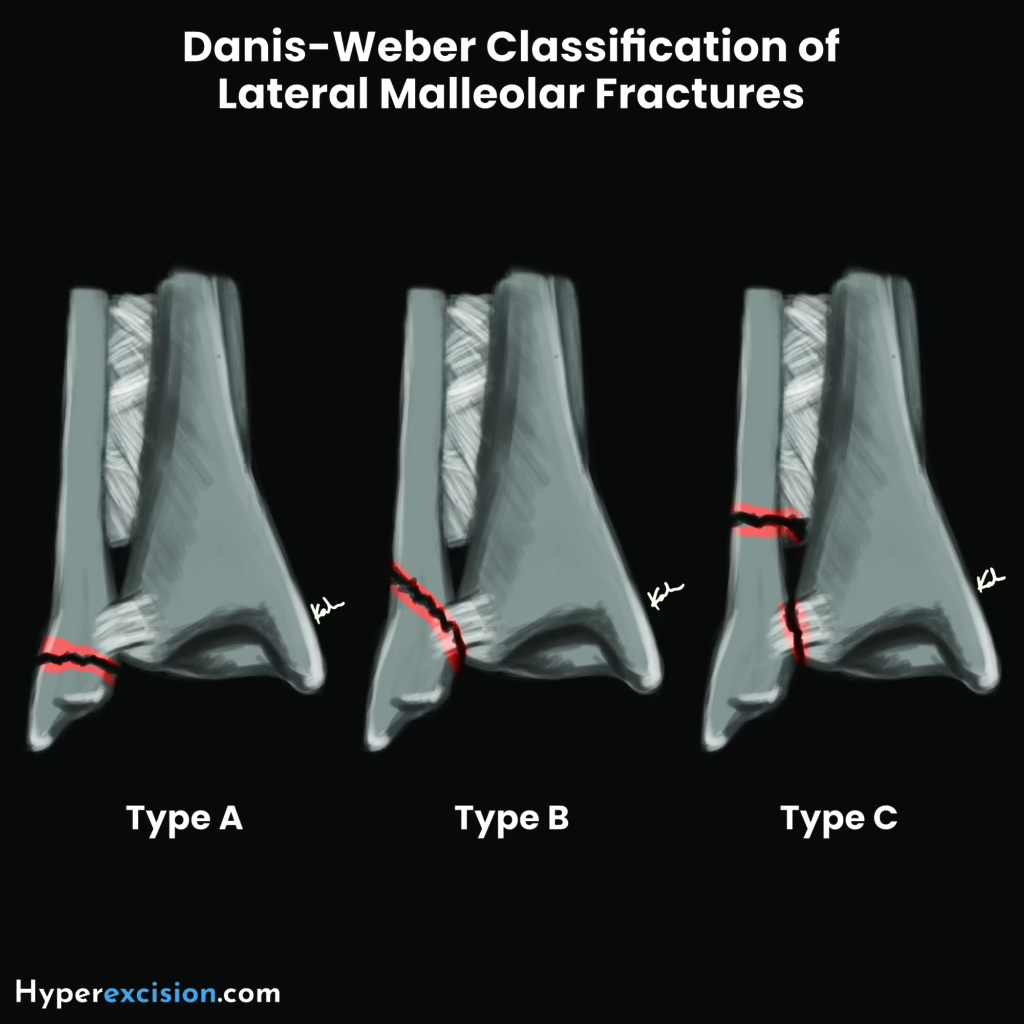
Danis-Weber – location of fibular fractures
| Classification | Description | Associated injury |
|---|---|---|
| Type A (infrasyndesmotic) | Transverse fracture of the fibular below the tibiofibular syndesmosis. Usually stable. | Oblique/vertical fracture of the medial malleolus |
| Type B (transsyndesmotic) | Oblique/spiral fracture of the fibular at the level of the syndesmosis. | Avulsion on the medial side or posterior malleolus, ATFL tear |
| Type C (suprasyndesmotic) | Severe fracture above the syndesmosis | Tibiofibular ligament tear and part of the interosseous membrane, avulsion of medial malleolus, ruptured medial collateral ligament, posterior malleolar fracture, and diastasis of tibiofibular joint |
Variants of ankle fractures
| Fracture type | Description |
|---|---|
| Isolated malleolus (70%) | Fracture of either the lateral or medial malleolus. May be stable. |
| Bimalleolar | Fracture of both the medial and lateral malleoli. Unstable. |
| Trimalleolar | Fracture of the medial, lateral and posterior malleoli. Highly unstable |
| Isolated posterior malleolus | Fracture of the posterior malleolus, due to axial load or plantarflexion |
| Maisonneuve fracture | Proximal fibular fracture with syndesmotic disruption + medial malleolus fracure or deltoid ligament rupture |
| Lefort-Wagstaffe fracture | AITFL avulsion fracture of the anterior fibular tubercle |
| Tillaux fracture (adolescent) | AITFL avulsion fracture of the anterolateral distal tibial epiphysis |
| Triplane fracture (adolescent) | Multiplanar involving the epiphysis, physis and metaphysis |
| Bosworth fracture-dislocation | Proximal fibular fragment is entrapped behind the tibia and remains irreducible by closed methods |
- Associated injuries
- Open fracture (2%)
- Syndesmotic injury (10%)
- Chondral injury
- Peroneal tendon tears (4%)
- Signs and symptoms
- Severe ankle pain
- Swelling and bruising
- Inability to bear weight
- Flat out inability to ambulate compared to ankle sprain
- Children may present with pseudoparalysis with ankle sprains
- Deformity
- Perimalleolar swelling
- Bruising
- Point tenderness over the posterior or tip of the malleoli (favors fracture over sprain)
- Physical examination
- Colour of the foot appearance (dusky appearance suggests compartment syndrome)
- Posterior tibial and dorsalis pedis pulse
- Sensation
- Firmness of muscles (difficult to test on the foot due to many bones)
- Limited ankle motion
- Investigations
- Ankle X-ray: AP, Lateral view (for level of fracture)+ 30 degree oblique ‘mortise’ view (for diastasis). Include X-ray of the Knee to rule out proximal fibular fracture (Maisonneuve)
- Decreased tibiofibular overlap (syndesmotic injury)
- Widened tibiofibular space (syndesmotic injury)
- Asymmetrical talotibial space
- Widened medial joint space
- Tilting of the talus
- CT-scan : For joint involvement and operative planning
- MRI: to evaluate for soft tissue or cartilaginous injuries
- Ankle X-ray: AP, Lateral view (for level of fracture)+ 30 degree oblique ‘mortise’ view (for diastasis). Include X-ray of the Knee to rule out proximal fibular fracture (Maisonneuve)
- Clues for hidden ligament injury on XR
- Widened tibiofibular space
- Asymmetrical talotibial space
- Widened medial joint space
- Tilting of the talus
- Management
- Reduce swelling: Elevation, foot pump, or cold-compress
- Reduction: Only be done by orthopedic surgeons OR when the patient has neurovascular compromise
- Definitive therapy determined by ortho
- Undisplaced Fractures
- Type A: minimal splintage w/ firm bandage or stisrrup brace for comfort
- Type B:
- Undisplaced Fractures
- Assessing the accuracy of reduction in ankle fractures
- Restore fibular to full length
- Talus sits squarely in the mortis w/ talar and tibial articular surfaces parallel to each other
- Medial joint space same width as tibiotalar space (4mm)
- No tibiofibular diastasis on oblique (’mortise view’) XR
- Complication
- Early complications
- Vascular injury:
- Wound breakdown and necrosis: in Diabetics and poorly padded casts
- Late complications
- Incomplete reduction: common and will lead to degenerative changes. Make sure talus fits mortise accurately.
- Non-union: flap of periosteoum or other soft-tissue may be interposed between the medial malleolus and tibia. Hence open reduction and internal fixation with screws to ensure union.
- Joint stiffness: d/t soft-tissue injury
- Complex regional pain syndrome (CRPS): common in ankle fractures. Sx include pain in foot with swelling and diffuse tenderness. Gradual development of trophic changes and severe osteoporosis
- Post-traumatic osteoarthritis: if malunion and/or incomplete anatomical reduction
- Early complications



