Overview
Acute complications of Diabetes Mellitus can be split into Hyperglycemic crises and Hypoglycemia. Hyperglycemic crises include Diabetic Ketoacidosis (DKA) and Hyperosmolar Hyperglycemic State (HHS). DKA and HHS have distinctly different pathophysiology but the basic management protocols are the same. Euglycemic DKA is just like DKA but without the hyperglycemia. Its incidence has been increased after the introduction of SGLT2 inhibitors for T2DM and off-label use for T1DM.
Diabetic Ketoacidosis (DKA)
Hyperglycemia + metabolic acidosis + Ketonuria = DKA
DKA is an acute, major life-threatening complication of Diabetes characterized by hyperglycemia, ketoacidosis, and ketonuria. It occurs when there is absolute or relative insulin deficiency, which inhibits glucose entry into the cell. The liver then rapidly produces ketones as an alternative source of fuel causing it to accumulate in blood and urine and make the blood acidic (anion gap metabolic acidosis). Diagnosis is clinical, but hyperglycemia, ketonuria/ketonemia, and anion gap acidosis can be used to confirm. Hyperkalemia is common in patients with DKA despite total body potassium being depleted.
DKA is predominantly seen in T1DM and is often a presenting problem in newly diagnosed patients. Intercurrent illness commonly causes DKA in established T1DM patients as these patients are unable to adjust their insulin dose appropriately to compensate for the increased stress and insulin requirements. DKA also develops because of errors in self-management, and in young patients with recurrent episodes of DKA, 20% have an underlying psychological problem complicated by eating disorders.
Approximately 5-8 episodes of DKA per 1000 people with diabetes occur annually. DKA has a mortality rate of approximately 1%. The mortality is higher in developing countries and among non-hospitalized patients. Mortality is also higher in the elderly than in younger populations. The most common cause of mortality in children and adolescents is cerebral edema. For adults, it is hypokalemia, ARDS, and comorbidities such as myocardial infarction, sepsis, and pneumonia.
Some variants of DKA
| Variant | Presentation | Patient History |
|---|---|---|
| Euglycemic DKA (EDKA) | Acidosis, Ketonemia but normal | SGLTi, Pregnancy, Alcoholism, Glycogen storage disease, Very low-calorie diet, Severe liver disease |
| Ketosis-prone Diabetes | Ketoacidosis in individuals without anti-GAD and anti-islet cell antibodies. Genotypically idiopathic TIDM but phenotypically T2DM. | African American, Asian, Sub-Saharan Africa, African Carribeans. Middle-aged and Obese. |
- Precipitating factors
- Infection (Commonly UTI and Pneumonia)
- Non-compliance
- Illicit drug use
- Treatment failure +/- inability to afford treatment)
- Surgery
- Trauma and Burns
- Alcohol use
- Drugs e.g. Glucocorticoids, Cocaine
- Pathophysiology
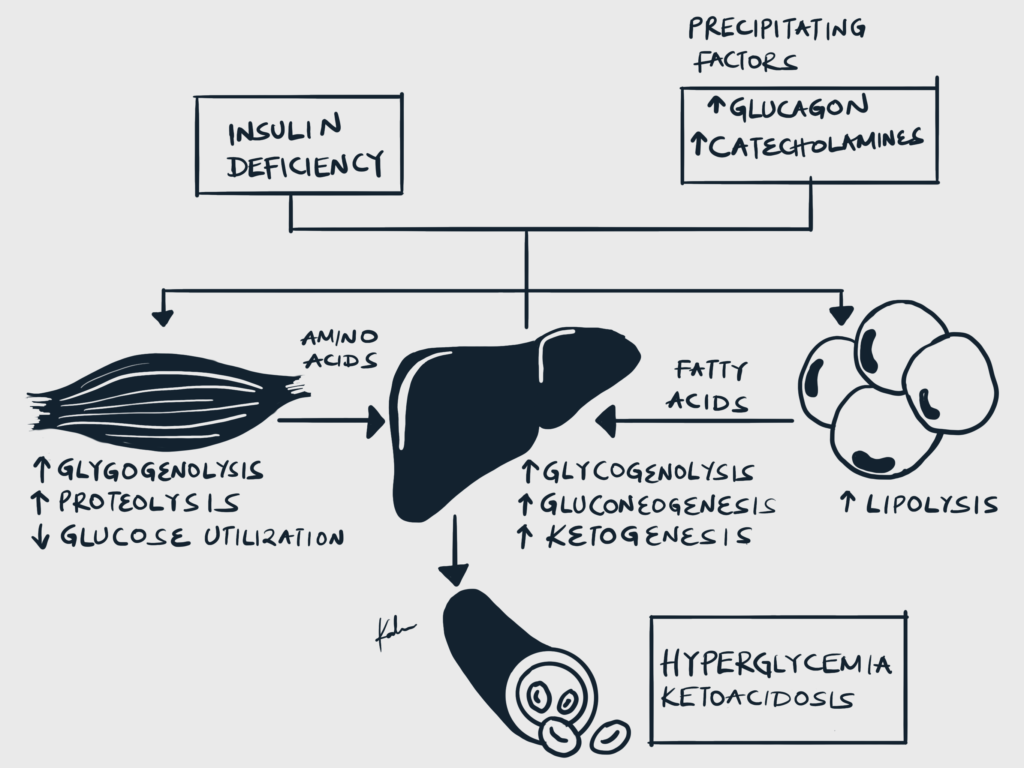
- Insulin deficiency and increased counter-regulatory hormones cause inhibition of glycolysis and increased gluconeogenesis and glycolysis → Hyperglycemia
- Insulin deficiency increases lipolysis through disinhibition of Hormone-sensitive lipase (HSL) → Lipolysis and generation of Free Fatty Acids → Ketogenesis
- Osmotic diuresis and hypovolemia
- Hyperglycemia causes hyperosmolality and osmotic diuresis which leads to volume depletion and hypovolemia
- Metabolic acidosis with increased anion gap
- Non-esterified fatty acids (NEFAs) generated from lipolysis are converted into ketones in the liver (acetoacetate, Beta-hydroxybutyrate)
- These ketones are acidic and bicarbonate is consumed as it buffers them.
- This causes metabolic acidosis with an elevated anion gap
- Intracellular potassium deficit
- Hyperglycemic hyperosmolality shifts potassium along with water from the intracellular to extracellular space
- Shifted potassium in the extracellular space is lost through urine
- Insulin is absent in DKA and can therefore not promote intracellular potassium uptake
- Total body potassium deficit develops although serum potassium may be normal or paradoxically elevated
- Signs and Symptoms
- Abdominal pain
- Nausea and vomiting
- Polyuria
- Polydipsia
- Fruity breath
- Palpitations
- Malaise
- Fatigue
- Reduced appetite
- Loss of consciousness
- Tachypnea (Kussmaul breathing)
- Signs of dehydration (dry skin and mucous membranes, reduced skin turgor)
- Hypotension
- Tachycardia
- Confusion
- Ill-looking patient
- What are the differentials for anion gap metabolic acidosis? (CUTMUDPILERS)
- Carbon Monoxide, Cyanide
- Alcohol (Ethanol, Methanol)
- Toluene
- Uraemia
- DKA
- Propylene glycol, Paraldehyde, Paracetamol
- Iron tablets, Isoniazid
- Lactic acidosis
- Ethylene glycol
- Renal failure
- Salicylates, sepsis, starvation
- Causes of hyperglycemia and hypovolemia
- Sepsis
- Acute pancreatitis
- Causes of Altered Mental Status
- Hypoglycemia
- Hepatic encephalopathy
- Uremic encephalopathy
- Wernicke encephalopathy
- Diagnostic criteria for DKA
- Acidemia: Venous Blood pH <7.3 or HCO3- <15.0mmol
- Hyperglycemia: Blood Glucose >11mmol/L, Know Diabetic
- Ketonemia or significant ketonuria: ≥3.0mmol/L or 2+ on urinalysis respectively
- Investigations
- Blood Glass Analysis: best initial test. High-anion gap metabolic acidosis (pH <7.3)
- RBS: hyperglycemia (>14mmol/L, may be high)
- HbA1C: determine glycemic control
- Urinalysis with dipstick: ketones
- CBC: Leukocytosis. Left-shift suggests infection
- Electrolytes
- Hyponatremia: due to osmotic diuresis or dilution as hyperglycemia shifts intracellular fluid into the extracellular space
- Hyperkalemia: insulin deficiency and acidemia shifts potassium to the extracellular space. Note that total body potassium is however depleted and may need to be replaced when therapy is started with insulin.
- Hypomagnesemia: due to osmotic diuresis
- Urea and Creatinine: elevated urea and creatinine suggests AKI secondary to volume depletion secondary to osmotic diuresis
- Blood culture: rule out infection
- Hydroxybutyrate: Elevated
- Chest X-ray: rule out pneumonia
- EKG: rule out myocardial infarction (patients with Diabetes may present with silent MI)
Grading the Severity of DKA
| Arterial pH | Serum bicarbonate | Anion gap | Mental Status | |
|---|---|---|---|---|
| Mild | >7.24 | 15-18 mmol/L | >10 mEq/l | Alert |
| Moderate | 7.0-7.24 | 10-15 mmol/L | >12 mEq/l | Alert or drowsy |
| Severe | <7.0 | <10 mmol/L | >12 mEq/l | Stuporous |
- Goals of treatment
- Restore volume deficit
- Resolve hyperglycemia and acidosis
- Correct electrolyte abnormalities (K+ > 3.3 mEq/L before administering insulin)
- Treat precipitating event
- Steps by step management of DKA Potassium levels must be ≥ 3.3 mEq/L before starting treatment. Do not add potassium to the first bag!Sodium bicarbonate can only be given if pH remains < 6.9 despite IV fluids
- Check blood glucose, ketones, and potassium
- Administer insulin and IV fluids to replace fluid loss
- NS at 2L first hour; 1L in subsequent hours
- 50 IU Insulin in 50mL 0.9% NS infused continuously at 0.1 units/kg/h. And continue the patient’s long-acting insulin at normal times or consider starting with newly diagnosed T1DM
- Re-check blood glucose and ketone bodies
- If glucose is normal (<11.1 mmol/L) and ketones are high continue Insulin and give Dextrose infusion (125mL of 10% Dextrose along NS) with Potassium
- When glucose is normal and ketones are normal stop infusion and give potassium as needed
Potassium replacement
| Serum K+ | Amount of KCl to add per litre of IV fluid |
|---|---|
| >5.5 | Nil |
| 3.5-5.5 | 40 mmol |
| <3.5 | Stop insulin. Seek help from HDU/ICU for higher doses |
- Causes of treatment failure
- Lack of insulin replacement therapy
- Insufficient insulin replacement therapy
- Additional procedures
- Urinary catheterization if anuric after 3hrs or incontinent
- Nasogastric tube if obtunded or persistent vomiting
- Central venous line
- Pregnant women
- Renal or cardiac failure
- Septic shock
- Other severe comorbidities and severe DKA
- ABG, Repeat CXR if SpO2 <92%
- ECG monitoring in severe cases
- Thromboprophylaxis with Low Molecular Weight Heparin
- Criteria for resolution of DKA
- Glucose <11.1 mmol/L
- PLUS at least 2 of the following:
- Venous pH > 7.3
- Serum bicarbonate ≥ 15 mEq/L
- Anion gap ≤ 12 mEq/L
- Complications of DKA
- Cerebral edema
- Arrhythmias secondary to severe hypokalemia and or acidosis
- Heart failure
- Respiratory failure
- Mucormycosis
- Hypoglycemia due to inadequate monitoring of glucose levels during insulin therapy
- Hypokalemia – the total body potassium depletion caused by osmotic diuresis is worsened during treatment by insulin-induced intracellular potassium shift, in the absence of adequate repletion
Hyperosmolar Hyperglycemic State (HHS)
HHS commonly occurs in patients with T2DM witch concomitant illnesses that cause reduced fluid intake. At at-risk population includes the elderly and those who are chronically ill as they have decreased thirst perception and or limited free access to water.
The mortality rate is higher for HHS than for DKA. This is because most patients with HHS are old and frail and usually present with comorbidities. However, incidences of DKA are much higher than HHS. The prevalence of HHS in children and young adults is increasing due to the exponential growth of obesity and increasing T2DM in this age group.
- Precipitating factors
- Acute illness: Infection, Myocardial infarction, Cerebrovascular events (Stroke), Pulmonary embolism, Acute pancreatitis
- Underlying conditions: Renal dysfunction, Congestive Heart Failure, Acromegaly, Burns, Cushing syndrome, Peritoneal dialysis, GI hemorrhage, Heatstroke, Hypothermia, Intestinal obstruction, Intellectual disability, Sepsis, Surgery: especially cardiac surgery, Thyrotoxicosis, Trauma
- Drugs that raise serum glucose, inhibit insulin or cause dehydration:
- Alcohol and cocaine
- Anaesthesia
- Antiarrhythmics: Encainide, propranolol
- SGLTi
- Antiepileptics: Phenytoin
- Antihypertensives: CCBs, Diazoxide
- Antipsychotics: Chlorpromazine, Clozapine, Olanzapine, Lithium, Risperidone, Duloxetine
- L-asparaginase
- Beta blockers
- Corticosteroids
- Thiazide and loop diuretics
- Histamine-receptor blockers: Cimetidine
- Immunosuppressive agents: Interferons, protease inhibitors
- Statins
- Non-compliance with oral hypoglycemics or insulin therapy
- Pathogenesis
- The pathogenesis of HHS is similar to that of DKA
- However, in HHS there is a small amount of insulin being secreted by the pancreas
- This insulin is sufficient enough to inhibit HSL activity, lipolysis, and in turn, ketogenesis.
- For this reason, HHS typically occurs in T2DM as it has relative insulin deficiency rather than absolute insulin deficiency as in T1DM. However, DKA can occur in the advanced stages of T2DM when beta cell function has declined markedly such that insulin levels are negligible.
- Complications of HHS
- Electrolyte abnormalities
- Hypoglycemia: inappropriate insulin administration
- Hypokalemia: inappropriate insulin and bicarbonate administration
- Cerebral edema
- Due to rapid lowering of glucose causing a rapid drop in plasma osmolarity. Neurons preferentially absorb water and swell during rapid dehydration
- This may lead to uncal herniation
- Acute Respiratory Distress Syndrome
- Due to a drop in paO2 secondary to a reduction in osmotic colloid pressure during therapy for HHS
- Vascular complications
- Thromboembolism due to hypotension and hyperviscosity caused by severe dehydration and contracted vascular volume
- Electrolyte abnormalities
- Signs and symptoms
- Polyuria
- Polydipsia
- Weight loss
- Weakness
- Stupor → Coma
- Seizures: occurs in 5% of patients, may be either focal or generalized
- Tachycardia
- Orthostatic hypotension
- Hypotension
- Tachypnea
- Hyperthermia, if infection is present
- Physical examination
- Altered mental status
- Lethargy
- Weak thready pulse
- Severe dehydration
- Poor capillary refill
- Decreased skin turgor
- Sunken eyes
- Dry mucous membrane
- Ill appearance
- Neurological deficits
- Coma
- Transient hemiparesis
- Hyperreflexia
- Generalized areflexia
- Lethargy → Coma
- Investigations
- Labs
- Blood glucose: 30mmol/L
- Serum osmolality: >320mOsmol/kg
- Plasma Bicarbonate: >15mmol
- Arterial Blood Gases: PH >7.3, Anion gap absent
- Urine Ketones: small ketonuria
- Serum ketones: Low or absent ketones
- CSF analysis: patients with acute alteration of consciousness and features that suggest meningitis or meningoencephalitis
- Lumbar Puncture: If meningitis of Subarachnoid hemorrhage is suspected
- Imaging
- Chest Imaging: To exclude pneumonia
- Abdominal Imaging: Indicated if the patient has abdominal pain or is vomiting
- CT head: indicated in patients with focal or global neurologic changes to exclude hemorrhagic stroke, subdural hematoma, subarachnoid bleeding, intracranial abscesses, and intracranial masses
- EKG: indicated in all patients with HHS and AMI or PE can precipitate the condition
- Labs
- Goals of treatment
- Rehydrate (while maintaining electrolytes)
- Correct hyperglycemia
- Treat the underlying disease
- Monitor and assist cardiovascular, pulmonary, renal and CNS
- Step-by-step management of HHS Consider LMWH thromboprophylaxis as there is a risk of occlusive events (Focal signs, chorea, DIC, leg ischemia, rhabdomyolysis)
- Protect the airway of obtunded or unconscious patients
- Replace fluids with IV NS over 48 hours
- Give Potassium when urine starts to flow
- If blood glucose does not fall 5 mmol/L/h with IV fluids give Insulin 0.05U/kg/h.
- Keep blood glucose 10-15 mmol/L in the first 24 hours to prevent cerebral edema
- Criteria for resolution of HHS
- Normalization of serum osmolality (<320 mOsm/kg)
- Normal mental status
- Poor prognostic indicators for HHS
- Hypothermia
- Hypotension (SBP <90mmHg)
- Tachy- or brady-cardia
- Severe hypernatremia (sodium >160mmol/L)
- Serum osmolality >360 mOsmol/kg
- Presence of other serious comorbidities
DKA vs HHS vs EDKA
| DKA | HHS | EKDA | |
|---|---|---|---|
| Predominant feature | Ketonemia and high anion gap metabolic acidosis | Very high glucose and serum osmolality | Ketonemia and high anion gap metabolic acidosis |
| Glucose | >13.9 | >33.3 | Normal (<11) |
| Ketones | > 3 mmol/L in blood, 2+ in urine | Normal | > 3 mmol/L in blood, 2+ in urine |
| Serum osmolality | Raised | > 320 | Raised |
| Predominant diabetes | T1DM, Less frequently T2DM and GDM | T2DM, Less frequently T1DM, T2DM in children and 6q24 genotype transient neonatal diabetes | T1DM, LADA, T2DM on SGLT2i, with pregnancy, glycogen storage disease, alcoholism, very low-calorie diet, severe liver disease |
| Age | Young | Older | Mostly young |
| Phenotype | Lean | Obese | Lean to obese |
| Complications | Cerebral edema, Iatrogenic hypoglycemia, Hypokalemia, ARDS, Arterial or venous thromboembolism | Iatrogenic hypoglycemia, hypokalemia, Myocardial infarction, disseminated intravascular coagulation, pulmonary, arterial or venous thromboembolism | Same as DKA |
Hypoglycemia
According to the American Diabetes Association (ADA 2021), Hypoglycemia in patients with diabetes is described as blood glucose ≤ 3.9 mmol/L. The threshold for the onset of hypoglycemic symptoms varies with patients. Severe symptomatic hypoglycemia occurs in most adults at blood glucose ≤ 2.2-2.8 mmol/L.
- Precipitating factors
- Insulin related
- Insulin excess – overdose or wrongly timed medication
- Liver or renal disease – decreased clearance of insulin
- Weight loss – increased sensitivity to insulin
- Increased exercise – increased sensitivity to insulin
- Drug interactions
- Glucose related
- Irregular ingestion of food
- Alcohol ingestion
- Extreme activity – increased utilization of glucose
- Prior episodes of hypoglycemia leading to impaired awareness of hypoglycemia
- Hypopituitarism and adrenal insufficiency
- Acute illness: sepsis, trauma, burns, organ failure
- Insulin related
- Pathogenesis
- Symptoms of hypoglycemia are related to activation of the sympathetic nervous system and brain dysfunction
- Stimulation of SNS causes sweating, palpitations, tremors, anxiety, and hunger
- The adrenergic symptoms precede neuroglycopenic symptoms and provide an early warning system for the patient
- Neuroglycopenia can manifest as confusion, difficulty with concentration, irritability, hallucinations, focal impairments (hemiplegia), and eventually, coma and death
- Threshold for symptoms
- Hypoglycemia associated autonomic failure (HAAF)
- The threshold for symptoms of hypoglycemia varies greatly
- Most adults become symptomatic at blood glucose ≤ 2.8 mmol
- The threshold for symptoms is variable in T1DM and Long-standing T2DM due to HAAF
- Recurrent episodes of hypoglycemia cause changes in the counter-regulatory response. There is reduced epinephrine release and this lowers the glucose threshold needed to trigger symptoms, thus leading to asymptomatic hypoglycemia
- The initial symptoms of patients with HAAF are often confusion
- Beta-blockers
- Beta-blockers can mask signs of hypoglycemia by antagonizing the effects of epinephrine
- Hypoglycemia associated autonomic failure (HAAF)
- Complications
- Coma
- Arrhythmia
- Death
- Permanent neurologic deficits
- Hemiparesis
- Memory impairment
- Diminished language skills
- Decreased abstract thinking capabilities
- Ataxia
- Whipple triad Helps confirm the diagnosis of hypoglycemia
- Low blood glucose levels (patients with diabetes have symptoms of hypoglycemia at higher thresholds than that of healthy individuals)
- Signs or symptoms consistent with hypoglycemia
- Relief of symptoms when blood glucose increases after treatment
- Signs and Symptoms due to increased sympathetic activity
- Tremor
- Pallor
- Anxiety
- Tachycardia
- Sweating
- Palpitations
- Signs and Symptoms due to increased parasympathetic activity
- Hunger
- Paresthesia
- Nausea
- Vomiting
- Neuroglycopenic symptoms
- Agitation
- Confusion
- Behavioral changes
- Fatigue
- Seizure
- Focal Neurologic signs
- Somnolence → Obtundation → Stupor → Coma → Death
- Differentials
- Differentials for hypoglycemia with AMS
- Primary CNS: Stroke, TIA, Seizure disorder, Tumor, Cerebral edema, TBI, Dementia
- Psychiatric: Depression, anxiety, psychosis, delirium
- Metabolic or autoregulatory: Hypoxia, endocrine derangements, electrolyte abnormalities, shock
- Infections: Sepsis, meningitis, encephalitis
- Pharmacological or toxin-related
- Medication side effects: sedatives, stimulants, opiates, anticholinergics, antiepileptics, polypharmacy
- Substance intoxication
- Withdrawal
- Poisoning
- Differentials for hypoglycemia with increased sympathetic activity
- Cardiac: Arrhythmia, ischemia
- Pulmonary: Pulmonary embolism, Pneumothorax
- Psychiatric: Pain disorder
- Metabolic: Hyperthyroidism, Thyroid storm, dehydration, shock
- Infectious: sepsis, active infection
- Pharmacological or toxin-related: Cocaine, amphetamine, alcohol intoxication, or withdrawal
- Pain
- Differentials for hypoglycemia with AMS
- Investigations
- CBC: Leukocytosis for infection
- RBS: Glucose levels
- LFTs: Liver failure
- TFT: Can suggest hypothyroidism
- Blood Ethanol: For alcohol-induced hypoglycemia
- Plasma insulin: Elevated insulin due to exogenous insulin
- C-peptide: Differentiate exogenous insulin from endogenous insulin
- Urine Sulfonylurea: Overdose or inappropriate ingestion of sulfonylureas
- Toxicology screen: For illicit drug use
Hyperinsulinism due to Exogenous insulin vs Sulfonylureas
| Exogenous insulin | Sulfonylurea | |
|---|---|---|
| Plasma insulin | Very high | High |
| C-peptide | Normal or low | High |
| Pro-insulin | Normal or low | Normal |
| Urine sulfonylurea | None | Present |
- Goals of treatment
- Reverse hypoglycemia (expect prompt recovery!)
- Treatment Fast-acting carbs cannot be used to treat hypoglycemia caused by alpha-glucosidase inhibitorsGlucagon will not work in malnourished patients since glycogen reserves have been depleted
- Conscious, oriented, and able to swallow
- 15-20g of quick-acting carbohydrate snack (200ml orange juice, sweets e.t.c)
- Repeat snacks up to 3 times
- Recheck Blood glucose q10-15min
- Conscious and uncooperative
- Squirt glucose gel between teeth and gums
- Unconscious or not responding to the treatments above
- IV Dextrose 10% at 200mL/h or IV Dextrose 10% 200mL/15min if unconscious
- Glucagon 1mg IV or IM
- Fast-acting carbohydrates: glucose tablets, candy, fruit juice (cannot be used to treat hypoglycemia caused by alpha-glucosidase inhibitors)
- Once blood glucose is >4.0 mmol/L give long-acting carbs (e.g. bread)
- Conscious, oriented, and able to swallow