Abnormal Uterine Bleeding (AUB)
Abnormal uterine bleeding is defined as menstrual blood loss (MBL) that interferes with physical, social, and mental quality of life, irrespective of the regularity frequency, or duration (NICE)
Heavy menstrual bleeding is the most common cause of iron deficiency anaemia. 20% of women complain of heavy menstrual bleeding. Perception of heavy menstrual bleeding remains unreliable since 50% of these women have a normal amount of blood loss when investigated.
Non-menstrual bleeding (postcoital, intermenstrual or post-menopausal bleeding) always warrants further investigation and early referral to a gynaecologist.
Normal vs Abnormal parameters for menstrual blood loss
| Parameter | Normal Range | Nota bene |
|---|---|---|
| Menarche | 10 – 16 years (mean age 13) | Abnormal if the thickness is out of phase or exceeds 16 mm in secretory phase |
| Cycle Frequency | 21–35 days | <21 is polymenorrhoea while >35 days is oligomenorrhoea |
| Bleeding Duration | 2–7 days | > 7 days suggest heavy menstrual bleeding |
| MBL Volume | 5–80 mL/cycle | >80 mL is heavy menstrual bleeding |
| Cycle Regularity | Variation < 9 days | Variation ≥ 9 days |
| Endometrial thickness (pre-menopausal) | 6 – 12 mm | It can be up to 8 mm if there is hormonal replacement therapy |
| Endometrial thickness (post-menopausal bleeding) | < 4 mm | Can be up to 8 mm if there is hormonal replacement therapy |
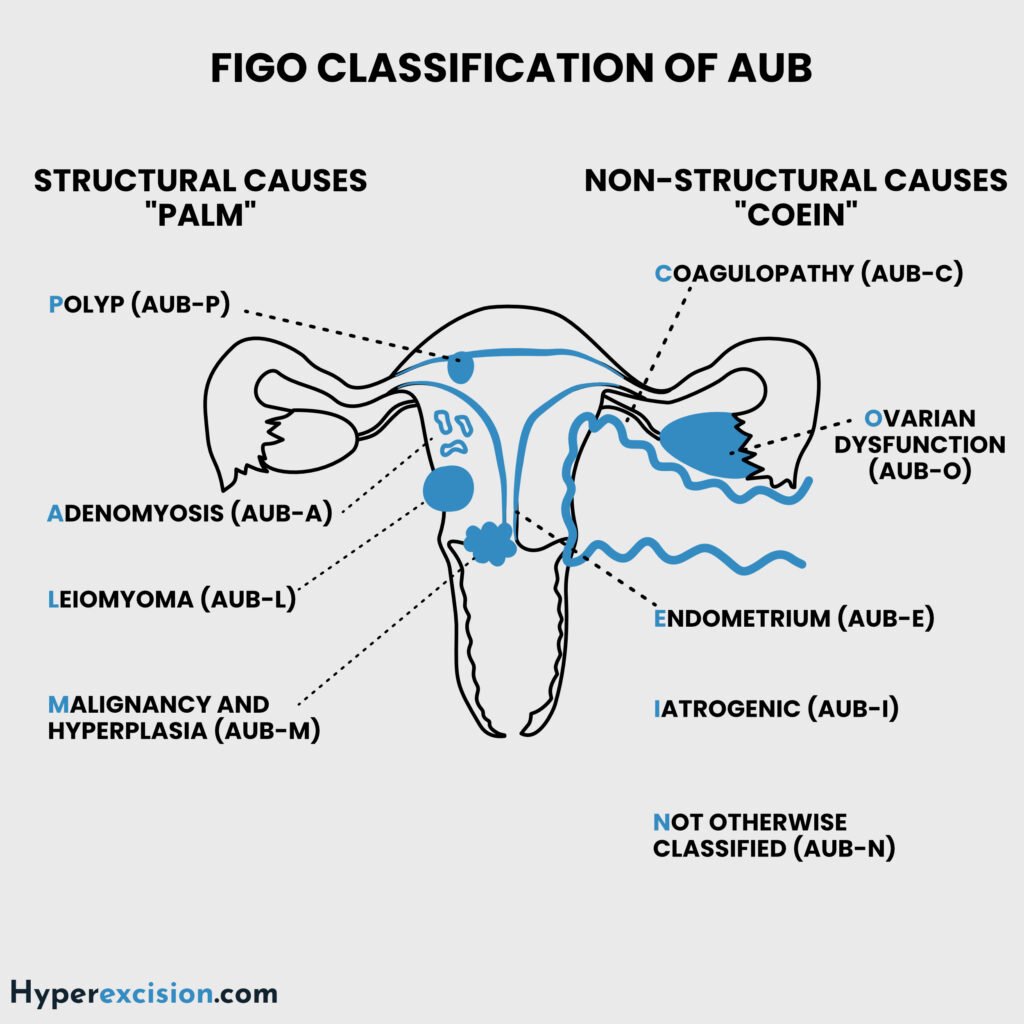
FIGO Classification of Abnormal Uterine Bleeding(PALM-COEIN)
Structural Causes (PALM)
| Acronym | Description |
|---|---|
| P | Polyps (AUB-P) |
| A | Adenomyosis (AUB-A) |
| L | Leiomyoma (AUB-L; submucosal most relevant) |
| M | Malignancy or hyperplasia (AUB-M) |
Non-Structural Causes (COEIN)
| Acronym | Description |
|---|---|
| C | Coagulopathy (AUB-C; e.g. von Willebrand disease) |
| O | Ovulatory dysfunction (AUB-O; commonly anovulation) |
| E | Endometrial (AUB-E; primary disorder) |
| I | Iatrogenic (AUB-I; e.g. anticoagulants, IUD) |
| N | Not classified e.g. niche, arteriovenous malformation |
- Some terms used to describe abnormal uterine bleeding
- Heavy menstrual bleeding (HMB)
- Intermenstrual bleeding (IMB)
- Postcoital bleeding
- Postmenopausal bleeding
- Oligomenorrhoea and amenorrhoea
- Dysfunctional uterine bleeding
- Irregular menstrual cycle
- Pathogenesis of uterine bleeding
- Fibrinolytic Pathway Dysregulation:
- Progesterone controls fibrinolysis.
- Increased Tissue plasminogen activator (tPA) > PAI-1 → Excessive clot breakdown
- Prostaglandin Imbalance:
- Increased PGE₂ (vasodilatory) vs. reduced PGF₂α (vasoconstrictive) → Increased blood flow
- Endometrial Inflammation:
- ↑ TNF-α, IL-1β → disrupted vascular integrity
- Fibrinolytic Pathway Dysregulation:
- Patient History
- Adolescents:
- AUB-O most common – infrequent cycles, painless prolonged or HMB
- Rule out coagulopathy (e.g., VWD in 20%) – HMB since menarche
- Perimenopause:
- Exclude endometrial hyperplasia/cancer first.
- HMB Indicators:
- Soaking >2 pads/hour
- Changing pads every 3 hours
- More than 20 pads used in 1 cycle
- Passing clots > 1 inch
- Needs extra pads at night
- Bleeding soils clothing or bedsheets
- Flow lasts > 7 days
- Signs and symptoms of anaemia
- Menstrual Patterns:
- Cyclical HMB = AUB-L (submucosal), AUB-A, AUB-C, AUB-E
- Cyclical IMB = AUB-P (benign or malignant)
- Acyclical HMB = Malignancy
- Acyclical IMB = AUB-O
- IMB and Post-coital bleeding = exclude malignancy and polyps
- Red Flags:
- Postmenopausal bleeding
- Weight loss
- Family history of malignancy (Lynch syndrome/BRCA)
- Adolescents:
- Investigations
- B-hCG: rule out pregnancy
- TVUS: to measure endometrial thickness and identify structural lesions
- Normal or thick endometrium = hyperestrogenic (hyperplasia with or without atypial – will respond to progesterone)
- Thin endometrium = low estrogen level (less risk of malignancy, may not respond to progesterone initially)
- Complete blood count and iron panel: assess for iron deficiency anaemia
- Endometrial biopsy: for high-risk patients – if age >45 or unopposed estrogen exposure
- Hysteroscopy: to identify for focal lesions
- Coagulation panel
- Medical treatment
- Keep a menstrual calendar
- NSAIDS and Tranexamic or mefanamic acid for 5 days: first-line. Controls bleeding in 60 – 80% of patients
- Tranexamic acid reduces MBL by 40 – 50%
- NSAIDs reduce bleeding by 30%
- High-Dose Progestin e.g. Norethisterone for 10 days to stabilize the endometrium
- Combined oral contraceptive pills: 80% of patients respond to COCs
- Hormonal IUD (MIrena/LNG-IUD): most effective hormonal agent. Reduces bleeding by 95%
- Surgical treatment
- Temporary Balloon tamponade
- Hysteroscopic resection of polyps or submucosal fibroids
- Endometrial ablation for refracotry AUB-E (contraindicated if future fertility is desired)
- Hysterectomy
Long-term treatment
| Cause | Treatment |
|---|---|
| AUB-O | Cyclic progestins/COCs |
| AUB-L | Myomectomy/Uterine artery embolization |
| AUB-A | LNG-IUS/endometrial ablation |
| AUB-C | Desmopressin (for VWD) |

