Overview
- Briefly describe Enterobacteriaceae
- Enterobacteriaceae are gram negative rods that inhabit a wide variety of niches (Human GIT, Animal GIT, Environmental sites and Urinary tract).
- Some are agents of zoonoses.
- They are facultative anaerobes.
- Some are encapsulated (e.g. Klebsiella)
- They ferment glucose with acid production and reduce nitrates to nitrite (possess nitrate reductase).
- Most are oxidase negative (Lack cytochrome oxidase) and catalase positive (Except Shigella dysenteriae type 1, though this is not used for identification)
- They contain endotoxin in their cell wall, posses a peritrichous flagella if motile and are non-spore forming.
- They are able to grow in media with bile salts.
- Enterobacteriaceae posses the O antigen, K antigen and H-antigens, and Endotoxin, and exotoxin.
- Sources of transmission of enterobacteriaceae include: Endogenous strains infecting normally sterile body sites, nosocomial infections, ingestion of contaminated foods or water (*Salmonella spp. Shigella spp. Yersinia enterocolita, Escerichia coli), Vector-borne (Yersinia pestis via flee bits) *and zoonoses (animals)
- Lactose fermenting (coliform) Enterobacteriaceae include Escherichia coli (Citrate negative), Klebsiella spp. (Citrate positive), Citrobacter and Enterobacter spp. Non-lactose fermenting Enterobacteriaceae include Salmonella, Shigella, Proteus, Yersinia.
- Briefly describe the Ewing’s Classification of Enterobacteriaceae
- I. Escherichieae – Escherichia, Shigella
- II. Edwardisellae: Edwardsiella
- III. Salmonelleae: Salmonella, Arizonae
- IV. Citrobactereae: Citrobacter
- V. Klebsielleae: Klebsiella, Enterobacter, Hafnia, Serratia
- VI. Proteae: Proteus, Providencia, Morganella
- VII. Yersinieae: Yersinia, Pasteurella
- VIII. Erwinieae: Erwinia, Pectobacterium ***Current classification is based on: morphology, biochemical, serological and DNA-based characteristics. This yields Bergey’s manual, Kauffmann and Edwards-Ewing’s classification ***Divided into major groups or tribes (with genera or subgenera) → different types (biotypes i.e. biochemical tests, serotypes i.e. antigenic types, bacteriophage types).
- Describe the antigenic structure of Enterobacteriaceae
- O-antigen: heat stable, cell wall or somatic, O-specific polysacharides on LPS
- K-antigen: heat labile, capsular, Vi in Salmonella
- H-antigen: heat labile, Flagellar flagellin amino acid sequence)
- What is the pathogenecity and spectrum of diseases caused by Enterobacteriaceae
- Opportunistic pathogens: Citrobacter spp, Enterobacter spp. Klebsiella spp, Proteus spp, Serratia spp
- Overt pathogens: Salmonella typhi (Typhoid fever), Shigella spp (Dysentery), Yersinia pestis (Plague) ***Eschericia coli lies somewhere in between as an over an opportunistic pathogen
- Briefly describe the laboratory characteristics of Enterobacteriaceae
- Characteristics: Gram-negative facultative anaerobes, Oxidase negative (Lack Cytochrome Oxidase)
- Fecal isolate: agar containing lactose and a pH indicator: MAC and EMB
- Cultivation
- Routine: SBA, CBA, MacConkey Agar
- Hektoen-enteric (HE) agar, Xylose Lysine Deoxycholate (XLD) agar, Salmonella Shigella (SS) agar
- Urinary pathogens: Isolated on CLED
- Biochemical identification by Analytical profile index (API) panels and automated and semi-automated sytems
- Triple Sugar Iron (TSI), IMViC series, Motility testing (MSM)
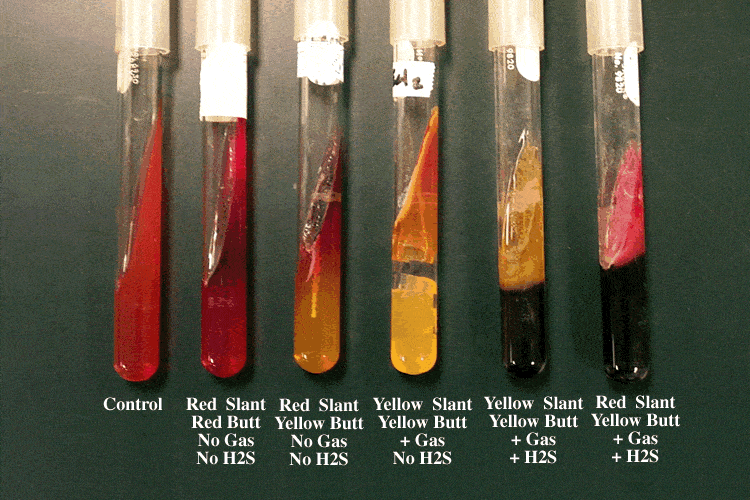
- Describe the Triple Sugar Iron (TSI) test
- TSI is used to determine whether GN bacilli utilize glucose and lactose/sucrose fermentatively and produce H2S. TSI agar contains 0.1% glucose, 1% lactose and 1% sucrose, phenol red (indicator) and iron salts (react with H2S to form a black precipitate) Media becomes yellow when acid is produced. Gas is H2O and O2 ****Possible sugar reaction interpretations:
- Alkaline/ Alkaline (Red/Red): No sugar fermented, no gas, no H2SAlkaline/ Acid (Red/Yellow): Only glucose fermented No gas no H2SAcid/Acid (Yellow/Yellow): Lactose and or sucrose fermentation occurs, in addition to glucose fermentation
- TSI is used to determine whether GN bacilli utilize glucose and lactose/sucrose fermentatively and produce H2S. TSI agar contains 0.1% glucose, 1% lactose and 1% sucrose, phenol red (indicator) and iron salts (react with H2S to form a black precipitate) Media becomes yellow when acid is produced. Gas is H2O and O2 ****Possible sugar reaction interpretations:
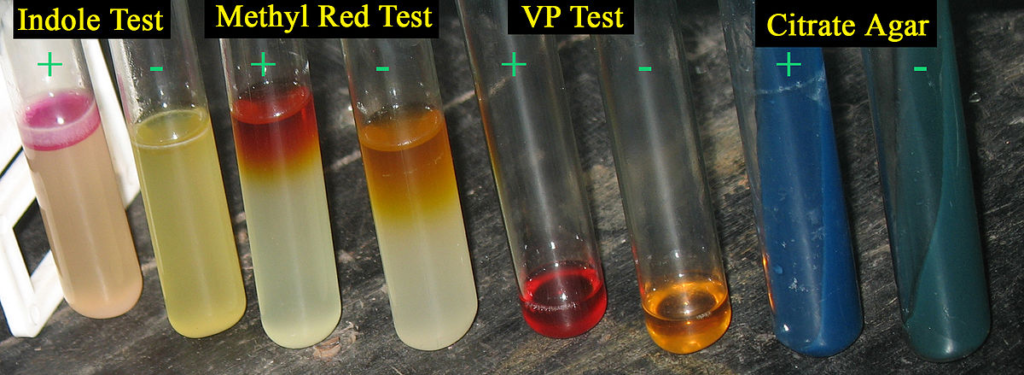
- Describe the IMViC series test
- Indole test:
- Differentiates enteric bacteria based on their ability ro metabolize tryptophan to indole. Cultures in peptone water broth containing tryptophan and Kovak’s reagent/erlich’s reagent as the indicator.
- Indole positive = Red/Crystal violet ring ****
- Methyl Red test:
- Based on the ability of the organism to oxidize glucose and end up with acidic by products. Inculated and cultured in MRVP broth containing Methyl red indicator
- MR Positive = Red colour
- MR Negative = Yellow/Pale colour
- Based on the ability of the organism to oxidize glucose and end up with acidic by products. Inculated and cultured in MRVP broth containing Methyl red indicator
- Vogues Proskauer:
- Based on the ability of the bug to produce acety-methylcarbinol from glucose. Inoculated and cultured in MRVP then small drops of Creatine, alpha napthol and sodium hydroxide are added
- VP positive – Red-Pink colour (Paler than MR test)
- VP negative – Pale/Yellow colour
- Based on the ability of the bug to produce acety-methylcarbinol from glucose. Inoculated and cultured in MRVP then small drops of Creatine, alpha napthol and sodium hydroxide are added
- Citrate test:
- Based on the ability of the bug to utilize citrate as a source of carbon and energy. Incubateed and cultured in Simmon’s citrate media or Koser’s media with Thymol (Bromothyl) blue indicator
- Citrate positive – Turbidity/ Blue colour
- Citrate negative – No turbidity
- Indole test:
- Describe the motility testing for bacteria (on SIM semi-solid agar)
- Cultured in Sulphur Indole Motility (SIM) semi-solid agar. Innoculation by stabbing. Can be used to differentiate Salmonella spp. from Shigella spp.
- Motility Positive: Turbid area that extends from the inoculation line
- Motility Negative: Red growth along the inoculation line but no extension
- H2S positive = Black colour
- Indole positive = Red ring on addition of Kovac’s or Erlich’s reagent
- Cultured in Sulphur Indole Motility (SIM) semi-solid agar. Innoculation by stabbing. Can be used to differentiate Salmonella spp. from Shigella spp.

- What are the constituents and principle of MacConkey agar (MAC)
- MacConkey agar contains bile salts and crystal violet (selective for GN by inhibiting GP), lactose and a red-dye (differential)
- Lactose fermenters = Pink
- Non-Lactose fermenters = Pale or Colourless
- MacConkey agar contains bile salts and crystal violet (selective for GN by inhibiting GP), lactose and a red-dye (differential)

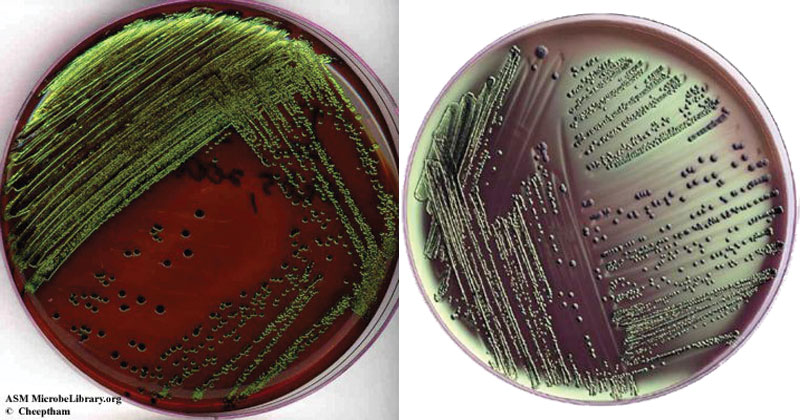
- What are the constituents and principle of Eosin-Methyl-Blue Agar (EMB)
- EMB contains peptone, lactose, dipotassium phosphate, eosin Y (dye), methylene blue (dye) and is selective for GN by inhibiting GP.
- Lactose fermenters = Green with a metallic sheen
- EMB contains peptone, lactose, dipotassium phosphate, eosin Y (dye), methylene blue (dye) and is selective for GN by inhibiting GP.
- What are the constituents and principle of Cysteine Lactose Electrolyte-Deficient Agar (CLED)
- CLED is used to culture urinary pathogens. It constains Cystein, Lactose, Bromothyl Blue (dye) and is Electrolyte deficient. Electrolyte deficiency = prevents swarming of proteus to ID individual colonies **(**useful for culture of urinary pathogens)
- Lactose fermenters = yellow
- Non-Lactose fermenters = Blue
- CLED is used to culture urinary pathogens. It constains Cystein, Lactose, Bromothyl Blue (dye) and is Electrolyte deficient. Electrolyte deficiency = prevents swarming of proteus to ID individual colonies **(**useful for culture of urinary pathogens)

Escherichia coli
- Briefly describe Escherichia coli
- Escherichia coli was named after the paediatrician Escheric.
- It is a **natural gut flora (**extensively found in large intestines and feces)
- It also colonizes the vagina and distal urethra.
- It is the single most common member of enterobacteriaciae found in fecal matter.
- Isolation of E.coli from water indicates recent pollution with human or animal feces.
- Reservoirs are humans and animals.
- Other species include Escherichia fergusonii, Escherichia hemanii, Escherichia vulneris, and Escherichia blattae.
- List the sources of infection of Escherichia coli
- The patient’s own normal flora (ascending the urethra to cause UTI)
- Maternal birth canal flora (vertically transmitted to cause neonatal meningitis and sepsis)
- Contaminated food and water (to cause traveler’s diarrhea)
- Undercooked meat (notoriously EHEC 0157:H7 diarrhea)
- Nosocomial (in premature infants and those requiring mechanical ventilation)
- How is Escherichia coli serotyped?
- Typing is based on the O group.
- Each O group is further divided into subgroups based on K antigens
- Each subgroup contains strains with different H antigens (O → K → H) i.e. O111:K58:H2.
- Strains found in the normal intestines of humans do not have the K antigen (K antigen is only present in extraintestinal srains.
- Normal colony strains – “early” O groups (1, 2, 3, 4 etc.)
- Enteropathogenic strains: “Later” O groups (55, 86, 111, 112)
- List the different strains of Escherichia coli and their Key associations
- Enteropathogenic E.coli (EPEC) – Gastroenteritis, Nosocomial infections, cholecystitis, and peritonitis, Microvilli effacement, infantile and childhood diarrhea ,outbreaks in maternity hospitals and neonatal units, self-limiting infection that may progress to chronic infection, prevented via breastfeeding (IgA, Lactoferrin), aseptic prep of feeds in bottles, hand-washing, good hygiene
- Enterotoxigenic E.coli (ETEC) – Traveller’s diarrhea, ST and LT toxins
- Enterohemorrhagic E.coli (EHEC) OR Verotoxigenic E.coli (VTEC) OR Shiga-toxin producing E.coli (STEC) – gastroenteritis, hemorrhagic colitis, and HUS, Improperly stored or incompletely cooked beef product, petting cows, apple juice, alfafa sprouts contaminated with cattle feces, Shiga-like toxin = apoptosis
- Enteroinvasive E.Coli (EIEC) – Dysentery-like syndrome (Shigellosis like, abdominal pain and fever), Blood, mucus, PMNs in feces
- Enteroaggregative E.coli (EAEC) – Watery diarrhea and chronic diarrhea in children of developing countries, Stacked brick appearance on Hep-2 cells or glass due to agglutination (Pili, plasmin mediated), plasmid mediated aggregative adherance of rods with shortened microvilli, mononuclear infiltration and hemorrhage (animal strains)
- Diffusely Adherent E.Coli (DAEC)
- Uropathogenic E.coli (EPEC) – UTI (Pyelonephritis and Cystitis), hemolysins, P-fimbriae, Ascending and descending infection, forms intracellular bacteria colonies, K-antigen
- Neonatal Meningitis Causing E.coli (NMEC) – Neonatal meningitis and pneumonia, natural gut flora, K1 capsular polysaccharide (cross reacts with capsule of N-meningitidis)
- Describe the **pathogenesis and key associations of the diarrheal strains of Escherichia coli
- Enteropathogenic Eschericia Coli (EPEC)
- Atthaches to enterocytes → effaces microvili → impaired absorption of water and electrolytes → watery diarrhea +/- fever
- Gastroentertitis, Nosocomial infection, Cholecystitis, Peritonitis, Infantile and childhood diarrhea, Outbreaks in maternity hospitals and neonatal units, Self-limiting inections prevented via breasfeeding IgA and lactoferrin, Aseptic preparation of feeds in bottles, hand-washing, good hygeine
- Enterotoxigenic Eschericia Coli (ETEC)
- LT causes ADP ribosylation of Gs → Activation of AC → Increased cAMP → net fluid and electrolyte ecretion → Profuse-watery non-bloody diarrhea
- ST binds glycoprotein receptor → Activates GC → Increased cGMP → Inhibits intestinal fluid and electrolyte uptake → net fluid secretion and diarrhea
- Traveller’s diarrhea
- Enterohemorrhagic Eschericia cColi (EHEC)
- Shiga like-toxin → effacement lesions
- Shiga like-toxin → Modifies 28S rRNA of 60S subunit by removing adening → Inhibits Elongation Factor → Inhibition of protein syntehsis → Apoptosis
- Gastroenteritis, Hemorrhagic colitis, Hemolytic Uremic Syndrome – Beef products, petting cows, apple juice, alfafa sprouts contaminated with cattle feces
- Enteroinvasive Eschericia coli (EIEC)
- Invasion via endocytosis → Lateral spread to adjacent cells → tissue destruction, necrosis, ulceration
- Dysentery-Like (Shigellosis like) syndrome – Bloody mucus diarrhea with PMNs in feces
- Enteroaggregative Eschericia Coli
- Enteroaggregative heat stable toxin (EAST-1) → Hemorrhagic necrosis and edema
- Pili – plasmin mediated aggregative adherance of the rods causing shortening of microvilli, mononuclear infiltration and hemorrhage
- Watery diarrhea, Chronic diarrhea in children of developing countries
- Enteropathogenic Eschericia Coli (EPEC)
- Discuss the pathogenesis and diseases caused by UPEC
- Pathogenesis
- P-fimbriae (Pyelonephritis associated pili) → binds to epithelial cells of UT to colonize bladder, prevents elimination when voiding
- Alpha and beta hemolysins → Lyse RBCs and UT cells causing cytokine release, inflammation and promote invasive disease
- K antigen → contributes to biofilm formation, immune evasion, antibiotic therapy causing chronic UTI
- Formation of intracellular bacterial communities → evades innate immunity
- Ascending infection
- Hematogenous infection (Descending)
- Diseases
- Cystitis
- Pyelonephritis
- Asymptomatic bacteriuria
- Pathogenesis
- Briefly describe the Laboratory features of Escherichia coli
- Specimen: Stool, Vomit
- Gram smear: Gram negative rod
- Culture: 35-37*c FOR 18-24 hours, Isolated on CLED yellow LF, Green sheen on EMB, Pink LF on MAC, B-hemolytic on BA
- Biochemistry: A/A, Gas, No H2S, IM positive, ViC negative, KSM negative, Ornithine decarboxylase positive, Lysine decarboxylase positive
- Serotyping: To identify diarrhoeic strains, Sorbitol MaC is used to serotype EHEC adn O157:H7 does not ferment sorbitol and colonies appear colourless
- Test for toxin production: Culture, ELISA and DNA probes
- Summarize the virulence factors, pathogenesis, clinical features, and laboratory features of Eschericia coli
- Virulence factors: P-fimbriae (Pyelonephritis associated, Pili, UPEC), Capsule (Extraintestinal strains), Peritrichious flagella (motility in some), Endotoxin (basically shock), O and K antigens (defense from complement and phagocytosis), **Exotoxins (**LT & ST ETEC, Shiga-like toxin EHEC), Colonizing Factor Antigen (CFA, adhesin), Intimin-Tir (Adhesin), Hemolysisn (UPEC, damages tubular epithelium promoting invasion), Aerobactin (UPEC, siderophore)
- EPEC: Attaches to enterocytes → effaces microvili → watery diarrhea +/- fever
- ETEC:
- LT causes ADP ribosylation of Gs → Activation of AC → Increased cAMP → net fluid and electrolyte secretion → profuse-watery non-blood diarrhea ***A (active subunit) B (Binding subunit)
- ST binds glycoprotein receptor → Activated GC → Increases cGMP → Inhibits ionic or intestinal fluid uptake → net fluid secretion and diarrhea}
- EHEC: Shiga-like toxin causes effacement lesions and its A subunit modifies 28S (part of 60s) rRNA by removing adenine base → Inhibition of elongation factor → inhibition of protein synthesis → apoptosis
- EIEC: invasion through endocytosis → lateral spread to adjacent cells → tissue destruction, necrosis, ulceration
- EAEC: shortens vili, forms mucus biofilm, Enteroaggregative heat stable enterotoxin (EAST-1) causes hemorrhagic necrosis and edema
- UPEC:
- Ascending infections: Fecal bacteria → spread up tract, bladder, kidney and prostate (F>M)
- Descending infections (Rare): Bacteremia → kidney/bladder → upper urinary
- P fimbriae (pyelonephritis-associtad pili) – binds to epithelial cells of UT colonize bladder and prevent eliminiation when voiding
- Alpha and beta hemolysins – lyse RBCS and urinary tract cells, causes cytokine relase and inflammation, promotes invasive disease
- Formation of intracellular bacterial communities – evades innate immunity
- K antigen – contributes to biofilm formation, avoiding immune factors and antibiotic therapy causing chronic UTIs
- Clinical features: UTI (Cystitis, pyelonyphritis, asymptomatic bacteriuria, UPEC), Diarrhea (EPEC, ETEC, EIEC, EHEC, EAEC), Septicemia (Septic shock and SIRS), Pyogenic infections – Wound infections and abscess (esp peritoneum after surgery of lower GIT or trauma), peritonitis (after appendicitis and trauma), Biliary tract infection, Neonatal meningitis (K1 antigen NMEC), Pneumonia (Immunocompromised)
- Laboratory features
- Specimen: Stool, vomit, urine, CSF, sputum
- Gram smear: Gram negative rods
- Culture: (Kleb colonis appear more mucoid than Escherichia coli)
- Nutrient agar – 35-37*C for 18 – 24 hours ****
- BA – B-hemolytic
- MaC – Pink LF ****
- EMB – Green sheen ****
- **MAC CLED (**Yellow LF)
- Biochemical tests:
- TSI: Acid/Acid, Gas, No H2S
- IMViC: Indole positive, Methyl Red Positive, Negative Vogues-Proskauer, Negative Citrate
- Klebsiella Screening Media (KSM) – Negative
- Ornithine decarboxylase – Positive
- Lysine decarboxylase – Positive
- Serotyping **(**for diarrhoeic strains identification – EPEC e.t.c)
- Sorbitol MacConkey Medium: Serotyping for EHEC (O157:H7 does not ferment sorbitol and colonies appear colorless)
- Tests for toxin production: in vivo and animal in vitro using culture, ELISA, DNA probes
- What is the treatment for E.coli infection
- Guided by in vitro susceptibility tests
- Community-acquired: sensitive to common antibiotics except penicilins
- Simple UTIs: TMP, ampicillin
- Diarrheal: self-limiting, antibiotic not usually necessary but reduce symptom duration, deferred till culture is available, risk of HUS in presumptive therapy
- Nosocimial infection is MDR: Cephalosproins, Carbapenems, FQs, AGs, Piperacillin-Tazobactum (PipTaz)
- What patients are at risk of Extended-spectrum Beta-Lactamase (ESBL) Escherichia coli infection**
- Those who are critically ill, prolonged hospitalization, have invasive medical devices, and are under heavy antibiotic treatment
Klebsiella
- Briefly describe Klebsiella
- Klebsiella is named after Edwin Klebs, a 19th century microbiologist.
- It was also called Frielander’s bacillus, isolated by Frielander in 1882 from fatal causes of pneumonia.
- Kleb is a short and plump gram negative bacillus with a large polysaccharide capsule (Colonies with characteristic mucoid appearance).
- He is a non-motile, lactose fermenting (coliform), facultative anerobe that is killed by moist heat at 55*C for 30 minutes.
- Kleb shows no hemolysis on BA (different from E.coli which shows B-hemolysis).
In a tabular format, illustrate the biochemical differences between Klebsiella spp. organisms
VP = Vogues Proskauer Lact = Lactose fermentation Ure = Urease Cit = Citrate Mal = Maltose utilization LDC = Lysine decarboxylase
| Test | VP | Lact | Ure | Cit | Mal | LDC |
|---|---|---|---|---|---|---|
| K. pneumonia | – | + | + | + | + | + |
| K. aerogenes | + | + | + | + | + | + |
| K. ozaenae | – | +- | – | +- | – | +- |
| K. rhinoscleromatis | — | – | – | – | + | – |
- List the **Klebsiella species ****and their key associations
- Klebsiella pneumoniae – (lobar)pneumonia, UTIs,
- Klebsiella ozaenae – atrophic rhinitis (Ozena)
- Klebsiella Rhinoscleromatis -rhinoscleroma
- Klebsiella oxytoca – HAIs
- Klebsiella granulomatis – granuloma inguinale or donovanosis (pseudobuboes, beefy red appearance, bipolar intracellular donova bodies)
- Summarize the virulence factors, pathogenesis, clinical features, and laboratory features of Klebsiella spp.
- Virulence factors: Pili (Adherance to RT and GUT), **K-antigen (**Capsule, antiphagocytic), Endotoxin (LPS, O-antigen, basically shock)
- Reservoirs: Patients GIT, Hands of hospital personnel (nosocomial)
- Normal flora of colon and biliary tract → aspiration into the Lower respiratory tract
- Invasive infection → sepsis
- nosocomial infection → Rapid spread
- Facilitating factors: Invasive devices, contaminated respiratory support equipment, use of urinary catheters, use of antibiotics, poor health status, therapy in ICU and nursing homes
- Clinical features
- Pulmonary infections
- Lobar pneumonia: rapid onset, high fatality, middle aged or older persons with medical problems i.e. DM, alcoholism, chronic bronchopulmonary disease, Extensive necrosis and hemorrhage → thick, mucoid, brick red sputum “currant jelly like” multiple lung abscesses → Friedlander’s pneumonia
- Bronchitis, bronchopneumonia
- Extrapulmonary infections: Meningitis and enteritis in infants, UTI, Septicemia, Cholecystitis, cholangitis, otitis, peritonitis, wound infections, osteomyelitis, thrombophlebitis, endocarditis, endophthalmitis, important cause of nosocomial infections unlike E.coli which is mostly community acquired
- Rhinoscleroma – chronic inflammatory process of the nasopharynx, purulent nasal discharge with crust and nodular formation, leading to respiratory tract obstruction, bacilli are seen intracellularly, treated with Rifampin
- Ozena – chronic atrophic rhinitis, necrosis of nasal mucosa, wasting of bony ridges and mucopurulent nasal discharge, not prominent like rhinoslceroma and often infects elderly persons, treated with TMP, Sulfamethoxazole
- Granuloma inguinale or donovanosis: painless non-purulent genital ulcers +/- SC granulomas (pseudobuboes) within inguinal region, lesions are highly vascular (beefy red appearance) and bleed, Diagnosis is clinical as it is difficult to isolate, Giemsa staining reveals bipolar intracellular Donova bodies, Transmission is through frequent sexual contact, fecal route or through an infected birth canal. Treatment is by azithromycin, doxycycline, ciprofloxacin, erythromycin, TMP-SMX and gentamicin 3 week course)
- Klebsiella oxytoca: Rarely isolated from clinical specimen, associated with neonatal bacteremia among premature infants and neonatal ICUs (HAIs)
- Pulmonary infections
- Laboratory features
- Specimen: Sputum, urine
- Gram stain: Gram negative Bacilli (Short-plump)
- Culture:
- BA: no hemolysis
- MacConkey: Pink, mucoid colonies
- CLED: Yellow , mucoid colonies
- Biochemistry:
- TSI: Acid/Acid , Gas , No H2S
- KSM: yellow +ve (ferments inositol turning the media yellow)
- IMViK: Negative Indole, Negative Methyl red, Positive Vogues-Proskauer, Positive Citrate
- What are the differential diagnoses of Donovanosis (Granuloma inguinale)
- Chancroid (Hemophilus ducreyi)
- Herpes Simplex (HSV)
- Lymphogranuloma venereum (Chlamydia trachomatis L1-L3)
- Pediatric syphillis (Treponema pallidum)
- What is the treatment for Klebsiella infection
- Resistant to ampicillin and other penicillins(B lactamase producers)
- HAIs – cephalosporins (cefuroxime ,ceforazim pneumonia and aminoglycoside)
- others: fluoroquinolones, ,3rd generation cephalosporins, azithromycin, doxycycline
Enterobacter and Citrobacter
- Briefly describe Enterobacter
- Enterobacter are motile **coliforms (**possess peritrichous fllagella).
- They are usually in mixed infections (wound, burns, pneumonia, TIs)
- Their general features are similar to those of Kleb (i.e. lactose fermenting, facultative anaerobe) .
- However, it differs by being motile, urease negative and ornithine decarboxylase positive.
- Colonies are mucoid.
- Found in soil, H2O, human feces and RT. Associated with nosocomial infections and are opportunistic.
- Discuss Enterobacter under the following: Endogenous infections, Exogenous infections, Virulence factors
- Endogenous infections: from skin, GIT or GUT colonized by the bacteria.
- Exogenous infections from hands of medical personnel, IV solutions, endoscopes, blood products, devices for monitoring intraarterial pressure and stethoscopes. MDR due to inducible beta-lactamases which are not detectable in vitro, but are responsible for resistance during treatment**. Blood culture i**s useful in bacteraemia.
- Virulence: express type 1 and 3 fimbriae (as Kleb) a-like hemolysin, outer memb proteins (OmpX Ent.cloacae) reduced sensitivity to B lactams. Toxins resembling E.coli verocytotoxin, + heat-labile toxins. Enterobactin (mediates high affinity iron uptake)
- Treatment: Resistant to penicillins, tetracyclines, chloramphenicol, streptomycin. Sensitive to other aminoglycosydes
- Briefly describe citrobacter
- Citrobacter is a coliform (LF) that is part of the normal intestinal flora.
- It is associated with nosocomial UTI, respiratory infections, endocarditis, neonatal meningitis and brain abscesses.
- MDR: Treat with Ags Carbapenems, FQs, Antipseudomonal penicillins
Proteus-Providencia-Morganella group
- Briefly describe the proteus-providencia-morganella group
- This group primarily cause UTI, both Community Acquired and Hospital Acquired.
- They are urease positive indole positive (Proteus mirabilis is indole negative), produce H2S gas
- Briefly describe Proteus
- Proteus is named after the Greek god Proteus who could assume any shape.
- Proteus (along with other members of the tribe Proteae) are Gram negative, unencapsulated, pleomorphic, motile bacilli that are MR positive and VP positive.
- Species of importance include:
- Proteus mirabilis (32 O antigens) ******
- Proteus vulgaris (22 O antigens).
- Proteus inhabits the GIT tract of man and animals, soil, sewage and water.
- It is a frequent contaminant of culture.
- Proteus is actively motile at 20-28*C and are arranged as singles, in pairs or in short chains.
- Many of them are long, curved and filamentous in young cultures.
- They produce two important enzymes:
- Urease (Associated with proteus and its disease manifestation)
- Phenylalanine deaminase (Important for its lab identification).
- Proteus is highly motile and exhibits a swarming effect on BA.
- They also exhibit **Dienes phenomenon (**whereby swarming is inhibited by dissimilar serotypes which produce colchicine-like factors that are species specific) – This is important for determining multiple or point sources during epidemics. *** Proteus does not swarm on CLED due to its electrolyte deficiency.
- The O-antigens of some strains (OX-2, OX-19, OX-K) were previously used in the Weil-felix reaction since the agglutinated with serum from patiens with rickettsial disease (typhus fever).
- Proteus swarming is inhibited by CLED and MAC enriched with Bile salts
In a tabular format, differentiate between Proteus mirabilis and Proteus vulgaris
| Proteus mirabilis | Proteus vulgaris | |
|---|---|---|
| Urease | Positive | Positive |
| Citrate | Varies | Varies |
| Indole | Negative | Positive |
| Gas (Glucose fermentation) | Positive | Different |
| Sucrose fermentation | Negative | Positive |
| H2S | Positive | Positive |
| Phenylalanine deaminase | Positive | Positive |
What laboratory characteristics distinguish Proteus from Morganella and Providencia?
| Proteus mirabilis | Proteus vulgraris | Morganella morganii | Providencia spp. | |
|---|---|---|---|---|
| Urease | Positive | Positive | Positive | Positive/Negative |
| Citrate | Varies | Varies | Negative | Positive |
| Indole | Negative | Positive | Positive | Positive |
| Glucose fermentation (Gas) | Positive | Varies | Varies | Varies, P. stuartii is negative |
| Sucrose fermentation | Negative | Positive | Varies | Varies, P. stuartii is negative |
| H2S | Positive | Positive | – | – |
| Phenylalanine Deaminase | Positive | Positive | – | – |
- Summarize the virulence factors, pathogenesis, clinical features, and laboratory features of proteus
- Virulence factors: Urease (Hydrolyzes urea into NH3), Fimbriae (uroepithelial colonization), Flagella (numerous, motility and spread), LPS (endotoxin, basically shock), Hemolysisns (Invasin, facilitates invasion of uropathogenic proteus)
- Pathogenesis: Attachment to uroepithelial cells (Fibmbriae):
- Secretion of IL-6 and IL-8 (immune response) → induction of apaoptosis and desquamation of epithelial cells
- Hydrolysis of urea into NH3 → increased urinary pH → Calculus formation (Magnesium ammonium phosphate = struvite, Calciium carbonae = apatite; bacteria in calculi are unaffected by antibiotics and are sites of reinfection) → obstruction of urine flow and damage to urinary epithelium → organism growth (alkaline pH favors) and extensive renal damage →
- Clinical features: Infections are nosocomial as proteus is found on the skin and oral mucosa of patients and hospital personnel. 90% of infections are by Proteus mirabilis
- UTI – especially in the elderly and young males following catheterization or cytoscopy. Infections associated with renal stones. 1-2% of UTIs in healthy women, 5% of HAIs UTIs/ Urethritis, cystitis, pyelonephritis, prostatis .
- **Abdominal and wound infections (**pressure sores, burns, damages tissues) – secondary infection
- Umbilical stump infection (neonatal sepsis, bacteremia)
- Nonclostridial anerobic myonecrosis (SC tissue, fascia and muscle + other organisms)
- Septicemia
- Occasionally meningitis, chest infection, Ear infections, Brain abscesses
- Proteus vulgaris is associated with HAIs (UTIs, Wound infections) and is normally more resistant to therapy than Proteus mirabilis. It has also been isolated from patients with chronic debilitating diseases and immunocompromise (Opportunistic)
- Laboratory features
- Specimen: Urine, pus, sputum
- Smear: GN pleomorphic, unencapsulated bacilli
- Culture:
- NA: 37*C (optium), aerobically, 12-24 hours, characteristic amoniac or fishy smell
- BA: Swarming
- MAC: Pale or colourless NLF
- CLED: Yellow LF
- Biochemical tests:
- Urease: Positive
- Oxidase: Negative (Pseudomonas is rapidly oxidase positive, on the other hand)
- TSI: alkaline/acid, Gas, H2S
- Indole: Negative (*P.mirabilis) ********Note however that Morganella and Providencia are indole positive
- Phenylalanine deaminase (PPA) reaction: Positive
- Beta-Galactosidase (ONPG): negative
- Urease test: positive (deep pink using pH indicator phenol red)
- Dienese phenomenon for typing Proteus strains
- Phage typing
- Serology
- What is the treatment for Proteus infections
- Sensitivity testing for sulfonamides, ampicillin (except mirabilis which is a B-lactamase producer), cephalosphorins, fluoroquinolones, aminogycosydes, resistance to polymixins, only 10-20% of strains devlop resistance to ampicillin and 1st gen cephalosporins
- Briefly describe Providentia spp.
- Includes Providencia alcalifaciens, Providencia rettgeri, Providencia stuartii.
- They are gram-negative, motile rods that cause UTI, burn infections and diarrhea.
- They are grown on selective enteric media (DCA, CLD, SS).
- Providentia are a differential diagnosis for shigella infection on KIA ( KIA contains lactose and glucose and is different from TSI).
- Briefly describe Morganella morganii
- Morganella morganii inhabits human and animal GIT, sewage, soil, and H20.
- It is a motile (some are non-motile) rod which occasionally causes UTIs, HAIs, and diarrhea in infants.
- Are NLF on MAC and do not exhibit swarming on BA
Serratia
- Briefly describe Serratia
- Serratia is pleomorphic, most are motile and are commonly resistant to penicillins and AGs. Causes UTI
- Important species is Serratia marcescens.
- Marcescens is Latin derived. It means decaying due to the fast-deteriorating nature of the bloody pigment produced by the bacteria.
- It is a Slow LF or NLF if picked earlier.
- Some species produce distinctive brick-red colonies (marscecens – red) on MAC.
Salmonella
- Briefly describe Salmonella
- Salmonella colonizes virtually all animals (Poultry, reptiles, livestock, rodents, domestic animals, birds, and humans)
- Animal-animal spread is through the use of contaminated animal feeds and this manintains the animal reservoir.
- Humans are the only host for Salmonella typhi and Patatyphi (A, B, C). They can establish chronic carriage in the gall bladder. The other strains have no host specificity and can cause disease in both human and non-human hosts.
- Others are found in arthropods (flies and cockroaches)
- Typhoid incidence is highest in the developing world.
- Classify Salmonella
- Classification of Salmonella spp. is problematic. It is mainly based on DNA hybridization.
- The most clinically significant isolates are those of Salmonella enterica.
- There are more than 2500 serotypes, though commonly listed as individual species:
- Salmonella typhi
- Salmonella choleraesuis
- Salmonella typhimuirium
- Salmonella enteritidis.
- List the sources of infection with Salmonella
- Contaminated water
- **Contaminated milk and dairy products (**Fecal contamination and inadequate pasteurization)
- Shellfish
- Dried or frozen eggs, fruits and vegetables,
- Meat and meat products (Infected poultry or contaminated with feces by rodents or humans)
- Recreational drugs (Marijuana)
- Animal dyes (Carmine, used in cosmetics and drugs)
- **Contact with infected reptiles (**Iguanas, pet turtles, and tortoises)
- Food handlers
- Briefly describe the antigenic structure of Salmonella
- O (somatic) antigen; Heat stable, Serotyping (variation in sugar composition and degree of polysaccharide branching), Less immunogenic (relative to H-antigen)p
- H (flagellar) antigen: Heat-labile, Genus specific (Flagellar proteins), Diphasic variation: in Salmonella Paratyphi, Phase 1 (specific or genus phase) and phase 2 (non-specific or group phase), Monophasic variation (Salmonella Typhi expresses only one H-antigen), Strongly immunogenic
- Vi antigen: Vi antigen because it was thought to confer virulence, surface polysaccharide (analogous to K antigen in coliforms), Encapsulates the entire bacteria (Makes it difficult for LPS-Ag recognition by antibiotics), Masks O antigen (Especially during diagnosis, heat bacterial suspension to remove it), Present in only a few serotypes (Typhi), Poorly immunogenic, Persistent antibodies (present in carrier state)
- M and N antigens: Polysaccharide antigens (M is responsible for mucoid colony formation)
- F antigen: present in Fimbriae
- What are the identifying features (characteristics) of Salmonella
- Pale NLF colonies on MAC
- Facultative anaerobes
- Ferment glucose, Mannitol and maltose forming acid only but not gas
- Do not decarboxylate ornithine
- Catalase positive
- Oxidase negative
- Motile
- H2S positive
- Indole negative
- Agglutinate with typhoid O antiserum (factor9/group D)
- Differentiate between chronic carriers, convalescent carriers and temporary carriers
- Chronic carriers are individuals who are infected with a pathogen and are able to transmit the infection to others for an extended period of time, often for the rest of their lives. This can occur when the infection persists in the body and the individual does not develop immunity to it, or when the individual is able to clear the infection but continues to shed the pathogen and transmit it to others.
- Convalescent carriers are individuals who have recovered from an infection and continue to shed the pathogen for a period of time after their recovery. This can occur when the individual has cleared the infection but still has some of the pathogen present in their body, or when the individual has developed immunity to the infection but continues to shed the pathogen for a short period of time after recovery.
- Temporary carriers are individuals who are infected with a pathogen and are able to transmit the infection to others for a short period of time before they either clear the infection or develop immunity to it. This type of carrier is often referred to as a “transient carrier”
- What are the differential diagnoses of enteric (typhoid) fever
- Malaria
- Typhus
- Rickettsial disease
- Tuberculosis
- Toxoplasmosis
- Leishmaniasis
- Influenza
- Dengue Fever
- Brucellosis
- Appendicitis
- Amoebic Liver or Hepatic Abscesses,
- What are the complications of enteric (typhoid) fever
- Intestinal Perforation
- Intestinal obstructions
- Hemorrhage
- Reiter’s syndrome (Reactive arthritis)
- Hepatosplenomegaly (50%)
- What are the differential diagnoses of late perforations as a complication of enteric (typhoid) fever
- Perforated appendix
- Amoebic liver abscess
- TB peritonitis
- Infected ruptured atopic pregnancy
- Intestinal strangulation
- Briefly describe the laboratory features of Salmonella ***Diagnosis is Based on: Isolation of Salmonella spp by culture, Serodiagnosis via Salmonella spp antibodies and antigens, and Molecular diagnosis by DNA probes and PCR. Typhi can be differentiated from others by being citrate negative, not producing gas and producing small amounts of H2S
- Specimen
- **Stool (**positive in 1st week – enterocolitis and in chronic carriers), Blood culture (Positive in 1st week), Urine culture (Positive in 2nd week), Bone marrow sulture (Often positive, most sensitive, not routinely done), Duodenal drainage (Positive culture from carriers), Blood clots (recovered after clot digestion with streptokinase and incubated in broth) Other specimen
- Culture
- MAC: White NLF
- CLED: Blue NLF
- DCA: Yellow or colourless, often with a dark centre
- XLD: Red, some with black centres
- SS-agar: Colourless NLF, Some with black centres
- Selenite F broth: Cloudy tube, yellow colour
- Tetrathionate broth: Positive for growth (Tetrathionate-reducing bacteria can grow – Salmonella and proteus)
- TSI: Alkaline/Acid, Gas, H2S (Paratyphi A = No H2S, Typhimurium produces a lot of H2S, Typhi = no gas, small amount of H2S, Recall that this reaction is similar to Proteus spp. and should be confirmed with urease)
- Biochemical tests
- Motility: Positive
- Catalase: Positive
- Oxidase: Negative
- Urease: Negative
- Indole: Negative
- Citrate: Positive (Typhi and Paratyphi A are indol negative)
- Serological
- Slide agglutination test: Serogroup identification into A, B, C, D, or E based on ‘O’ antigen
- Widal test:
- Rapid antibody tests: Positive IgM (Suggests current infection, more sensitive and specific than Widal), Indirect hemagglutination, Indirect immunofluorescent Vi antibody, and indirect ELISA
- Antigen tests (SAT): Serum + Urine ELISA + Stool (SAT)
- Typing: Phage typing, antibiotic resistance typing, Plasmid and pulsified gel electrophoresis typing (Food poisoning types)
- Specimen
- Summarize the virulence factors, pathogenesis, clinical features and laboratory features of Salmonella
- Virulence factors:
- **Endotoxin (**responsible for systemic manifestations of disease)
- Type III secretion systems: 20 proteins that mediate epithelial endocytosis, transfer of virulence factors into host cell (molecular syringe) and bacterial invasion. Encoded by several Salmonella pathogenicity islands (SPI). Their absence yields avirulent organisms.
- SPI-1: nonphagocytic cell invasion, injects proteins into the cell
- SPI-2: Facilitates survival and replication within macrophages
- Fimbriae: species-specific, binding to M (microfold) cells present in peyer patches)
- **Acid tolerance response gene (**protects from stomach and phagosome acidic pH)
- **Enzymes (Catalase and SOD) (**protect from intracellular killing by macrophages)
- Pathogenesis of Typhoid fever
- Ingestion
- Enters M cells in the SI by endocytosis (roughling)
- Bacteria multiply within endosomes and Kill M cells
- Bacteria are discharged from the basolateral membrane and are taken up by Macrophages in Peyer’s patches
- Bacteria multiply inside Macrophages, move to the SM/IM lymph nodes
- Released into the blood
- Filtered by spleen, liver, bone marrow where they multiply
- Re-released into the blood
- Infect the GIT thrugh the gall bladder
- Ultimately cause inflammation, ulceration and necrosis
- Clinical features
- There is strain to strain variation in virulence. The infectious dose for Salmonella enterica serova Typhi is **Low (10^3)**so prson-person spread is common (***Note however that it is not as low as that of Shigella) A larger inoculum (10^6-10^8) is required with othr serotypes to overcome acidity. Infections occuring with Low infectious dose is seen in immunodeficiency (Immunosuppression, Leukemia, Lymphoma, SCD), Low gastric acidity (Antacid administration), Foods that rapidly transit the stomach (Liquid) or foods that increase gastric pH (Cheese, milk)
- Gastroenteritis and Food Poisoning:
- Associated with various Salmonella serotypes. Enterocolitis (invasion of the epithelium ans subepithelial tissues of the SI and LI), Symptoms occur 6-8H post-ingestion. Initially prsents as nausea, vominting and non-bloody diarrhe +/-fever, abdominal cramps, myalgias and headach. Dehydration can cause hyptension, cramps and renal failure. Can persist for 2-7 days before spontaneous resolution. Blood cultures are negative since the disease is localized in the GIT. Stool cultures are positive even after weeks of infection
- Enteric (Typhoid) Fever
- Caused by Salmonella typhi and Paratyphi A, B(Schottmuelleri), C (Hirchfeldii) [though commonly referred to as paratyphoids) The organism passes the ileal mucosa → mesenteric LNs → Thoracic duct → bacteremia → colonization of the gall bladder and reinfection of the intestines. Typhoid ulcers (Cuased by gut and lymphoid tissue inflamation) +/- hemorrhage (Blood vessel erosion) or Peritonitis (Perforation). 10-14 days after ingestion there is remittent fever which increases to a level of approximately 40C by the end of the 1st week, headache, myalgias, maaise, anorexia, abdominal pains for ≥1 week then +/- GI symptoms. Diarrhea is rarely prominent. Rose spots are erythematous maculopapular lesioons 2-4 mm in diameter that blanch on pressure. They often appear on the abdomen and fade after 3-4 days.
- Septicemia (+ Metastatic Disease)
- Septicemia is commonly casued by localized infection with serovars Typhy, Paratyphi and Choleraesuis. In Sickle Cell Anemia it presents as osteomyelitis, Pneumonia, and Meningitis. Septicemia commonly occurs in pediatrics, geriatrics and immunosuppressed (HIV has 20-100 fold increase in risk)
- Asymptomatic colonization
- Sites of asymptomatic colonization include the gall bladder, GIT, GUT, Bone marrow and liver. Asymptomatic carriers excrete salmonella for ≥ 1 year in their feces and urine. Food handlers are an important source of infection (Typhoid Mary). Asymptomatic colonization allows bacilli to survive in the community in non-epidemic times. Factors associated with rate of carriage include older age, female sex, presence of biliary tract disease, urolithiasis, and bladder infection with Schistosoma haematobium
- Laboratory features
- Specimen: Stool, Blood, Urine, Bone marrow, Duodenal drainage, Blood clots
- Culture: Blue NLF CLED, White NLF MAC, Yellow or colourles with dark centre DCA, Red with black centre XLD, Colourless NLF with black centre SS-agar, Cloudy tube with yellow colour Selenite F broth, Positive growth Tetrathionate broth, Alkaline/Acid No Gas small H2S
- Biochemical tests: Motility positive, Catalase positive, Oxidase negative, Urease, negaitve, Indole negative, Citrate positive
- Serology: Slide agglutination test, Widal test
- Rapid antibody test: Positive IgM, Indirect hemagglutination, Indirect immunofluorescet Vi antibody, Indirect ELISA
- Salmonella antigen test (SAT): Serum, Urine, Stool ELISA
- Typing: Phage typing, antibiotic resistant typing, plasmid and pulsified gel electrophoresis typing for food poisoning types
- What is the principle, interpretation, advantages and disadvantages of Widal tests?
- The Widal test is a blood test used to detect the presence of antibodies against Salmonella typhi.
- Principle: agglutination, in which the antibodies present in the patient’s blood bind to specific antigens present on the surface of the bacterium and cause the bacteria to clump together (agglutinate).
- Interpretation: To perform the test, a sample of the patient’s blood is mixed with a suspension of S. typhi bacteria and observed for the formation of clumps. The presence of clumps indicates the presence of antibodies against S. typhi.
- Advantages:
- relatively inexpensive and easy to perform
- Provides rapid results
- Disadvantages:
- It is not highly specific, it can produce false positive results in individuals who have been vaccinated against S. typhi or who have been exposed to other bacteria that cross-react with the test.
- It is also not very sensitive, it may not detect low levels of antibodies or may produce false negative results in individuals who are in the early stages of infection.
- What is the treatment for Salmonella infection?
- Enterocolitis: self limiting, lasts only 2-3 days without treatment
- Enteric fever: FQs (depends on sensitivity patterns) Ceftriaxone, Azithromycin
- Bacteremia: Cipro, CAF, cotrimoxazole, meropenem
- Meningitis: cefotaxime, ceftriaxone
- How is enteric (typhoid) fever prevented and controlled?
- Management of chronic carriers
- Role of Surgery
- Prophylactic antibiotics
- Vaccines, type, administration and schedule
- What are the constituents and principle of Selenite F broth?
- Selenite F broth is a fluid enrichment media with the selective agent beign sodium biselenite.
- It is mainly used for the isolation of Salmonella and Shigella from fecal specimen (Selenite was found to be inhibitory to coliforms and other enteric bacteria)
- Positive reaction = yellow appearance
- What are the components and principle of Deoxycholate Citrate Agar (DCA)?
- Selective and differential media,
- Looks like CBA.
- Sodium deoxycholate inhibits GP Bacilli
- Citrate salts inhibit other enteric bacteria.
- Selective and differential for Salmonella and Shigella
- What are the components and principle of Salmonella-Shigella agar (SS)?
- SS-Agar is a modified DCA – by adding bile salts, citrates and brilliant green (inhibits GP, Coliforms, Proteus swarming)
- Has beef extract, enzymatic digest of caserin, enzymatic digest of animal tissue, lactose (Carbohydrate source), Sodium thiosulfate and ferric citrate (Permit detection of H2S)
- LF: Red/Pink colonies
- NLF: Colourless colonies
- H2S production: colonies with a Black center
- What are the constituents and principle of tetrathionate broth?
- Fluid enrichment media that contains bile salts (inhibits GP and GN bugs other than Salmonella)
- What are the components and principle of Bismuth Sulphate Agar (BSA)?
- Principle: Salmonella and Shigella species are able to grow on the medium, while other types of bacteria are inhibited by the bismuth sulfate. The lactose fermentation test allows for the differentiation of different types of bacteria based on their ability to ferment lactose.
- Components:
- Bismuth sulfate: selective agent, inhibits the growth of Gram-positive bacteria and many Gram-negative bacteria, allowing only the growth of certain types of Salmonella and Shigella species.
- Agar: solidifying agent that is used to turn the liquid medium into a solid gel.
- Peptone: source of nutrients for the bacteria, providing them with amino acids, vitamins, and minerals.
- Sodium chloride: added to provide a source of electrolytes for the bacteria and to maintain the proper osmotic balance.
- Lactose: included as a differential indicator.
- What are the components and principle of XLD agar?
- Principle: Salmonella and Shigella species are able to grow on the medium, while other types of bacteria are inhibited by the deoxycholate. The presence of xylose and lysine allows for the differentiation of different types of bacteria based on their ability to utilize these compounds as sources of nutrients.
- Components:
- Xylose and lysine: sources of nutrients for the bacteria.
- Deoxycholate: a bile salt that is a selective agent to inhibit the growth of Gram-positive bacteria and many Gram-negative bacteria, allowing only the growth of certain types of Salmonella and Shigella species.
- Agar: solidifying agent that is used to turn the liquid medium into a solid gel.
- Peptone: source of nutrients for the bacteria, providing them with amino acids, vitamins, and minerals.
- Sodium chloride: added to the medium to provide a source of electrolytes for the bacteria and to maintain the proper osmotic balance
Compare and contrast Salmonella with Shigella
| Shigella spp. | Salmonella typhi | |
|---|---|---|
| Reservoir | Humans | Humans |
| Infectious dose | Low | High |
| Metabolite | Potent Shiga-toxin and endotoxin | Potent endotoxin |
| Disease | Typhoid fever | Bacillary dysentery |
| Nature of infection | Gastrointestinal | Systemic |
| Diarrhea | Prominent bloody-mucous diarrhea | Less-prominent diarrhea |
| Bacteremia | No | Yes |
| Chronic carriage | No | Yes |
| Motility | Non-motile | Motile |
| Lactose fermentation | No | No |
| H2S production | No | Yes |
| TSI reaction | K/A+ | K/A |
| Vaccine | No vaccine | Vaccine available |
| Immunity | Short period | Long-lasting |
Compare and contrast Salmonella Typhi with other Salmonellae
| Salmonella typhi | Other Salmonellae | |
|---|---|---|
| Reservoir | Humans | Animals, Eggs, Poultry |
| Infectious dose | High | High |
| Diarrhea as a prominent feature | Less prominent | More prominent |
| Bacteremia | Yes | No |
| Chronic carriage | Yes | Infrequent |
| Lactose fermentation | No | No |
| H2S production | Small amounts | Yes |
| Vaccine | Yes | No |
- What selective media are used to culture Salmonella
- SS agar
- XLD agar
- Hektoen Enteric Agar
- H and E agar
Shigella
- Briefly describe Shigella
- Shigella spp. is part of the tribe escherichieae.
- He is a gram negative rod and the causative agent of Bacillary dysentery (Same mechanism as EIEC)
- Man is the only natural host.
- Shigella is negative for everything* (No chronic carrier state, no vaccine, no capsule, no flagella, no H2S, NLF, Oxidase negative, Urease negative, Citrate negative)
- Some strains posses fimbriae
- What are the sources of infection for Shigella
- Fecal-oral
- Contaminates food
- Person-person contact
- Flies
- What are the Shigella spp. based on their biochemical characteristics and serology?
- Shigella dysenteriae (10 serotypes, impoverished tropical countries)
- Shigella flexneri (6 serotypes, underdeveloped countries)
- Shigella boydii (15 serotypes)
- Shigella sonnei (no serotypes, developed countries)
- List the virulence factors for Shigella spp.
- **Endotoxin (**released by autolysis and causes inflammation and ulceration)
- Exotoxin (Shiga toxin): produced by Shigella dysenteriae, phage encoded AB-toxin similar to Shiga-like toxin of EHEC, invasive organisms without toxin can still cause disease
- Cytotoxic activity: A subunit binds and delivers B subunit → B subunit cleaves 28s RNA preventing binding of tRNA and inhibits proteins synthesis → apoptosis, bloody diarrhea and invasion of lamina propria
- Enterotoxic activity: Inhibits uptake of sugar, aa, fluid and electrolyte like cholera toxin thus causing diarrhea
- Neurotoxic activity: meningitis and coma in severe infections
- Type III secretory system
- Actin-Based motility (No H-antigen): movement from cell to cell
- Ability to survive gastric aciditiy – only a small Infectious dose is needed to cause infection
- Describe the pathogenesis of Bacillary dysentery
- Invasion of intestinal mucosa (M-cells)
- Transport to subepithelium and phagocytosis by macrophage
- Phagosome lysis and macrophage apoptosis
- Release of IL-1 and PMN transmigration
- Shigella migration through disrupted tight juncitons
- Multiplication and intracellular spread via F-actin polymerization
- Epithelial cells die and fluids are lost
- What are the clinical features of Shigellosis (Bacillary dysentery)
- Bacillary dysentery has an incubation of 2-3 days.
- Initially, there is abdominal colic and watery diarrhea.
- Bloody mucous diarrhea is frequent and in small amounts.
- The cardinal features include lower abdominal cramps and tenrmus with abundant pus and blood in stool
- Septicemia is rare
- Severe illness can lead to pediatric febrile convulsions and HUS.
- Major groups affected include young children, travellers, MSM, HIV/AIDS patients, patients on chemotherapy, people in overcrowded areas like military camps and day-care centres.
- What complications are associated with Shigellosis (Bacillary dysentery) ***Rare because shigella rarely causes septicemia
- HUS (like EHEC)
- Reactive arthritis
- Intususception (in children)
- Bronchopneumonea
- DIC
- Toxic megacolon
- Rectal prolapse
- Briefly describe the laboratory features of Shigella)
- Specimen: Stool
- Microscopy: Gram negative rods
- Fecal smear with Methylene Blue: Numerous PMN, RBC, and epithelial cells
- **Culture (**in air at 37*C for 18-24 hours)
- MAC and DCA: Colourless NLF (Sonnei turns red because it is a prolonged LF)
- XLD: Red/ pink colonies
- HE: Green colonies
- SS: colourless colonies
- Peptone water and nutrient broth: uniform turbidity
- Biochemical tests
- Urease: Negative
- Citrate: Negative
- Oxidase: Negative
- Catalase: Positive (Except Shigella dysenterieae I)
- Mannitol fermentation: Negative
- TSI: K/A, no gas, H2S-
- Motility: Non-motile
- What is the treatment of Shigellosis (Bacillary dysentery)
- Most cases are self-limiting
- Oral rehydration to replace fluids and electrolytes
- Antibiotics are given only in extremely aged patients, immunocompromised or severe infections
- Antiperistaltic drugs prolong fever, diarrhea and excretion of bacteria
- Antibiotics: FQs, Azithromycin, Cephalosporins,
- Major resistance to tetracycline, ampicillin and clotrimazole
- No vaccine
- How is Shigellosis (Bacillary dysentery) prevented and controlled
- Adequate chlorination of water
- Good personal hygiene
- Health education
- Proper seqage disposal
- Avoid swallowing water from swimming pools or lakes



