Overview
Knowing the physiology and pathology behind wounds is important in surgery since it is a specialty that primarily deals with wounds.
| Term | Definition |
|---|---|
| Wound | A break in the integrity of skin or tissue, often associated with disruption of structure and function, and is commonly due to external force. |
| Ulcer | A type of wound whereby there is disruption or break in the continuity of any lining (skin, mucous membranes, etc.) |
Phases of Wound Healing
Wound healing is defined as the normal body response to surgical or traumatic injury in order to restore normal structure and function. The normal process of wound healing should occur in 4-6 weeks.
There are three phases of wound healing:
| Phase | Processes involved |
|---|---|
| Hemostasis and inflammation | Hemostasis, chemotaxis, epithelial migration |
| Proliferation | Collagen synthesis, matrix synthesis and deposition, angiogenesis |
| Remodelling | Contraction, scar formation, scar remodelling |
| Term | Definition |
|---|---|
| Regeneration | Perfect restoration of pre-existing tissue architecture without scar formation |
| Repair | Wound healing that occurs by proliferation of connective tissue leading to scar formation |
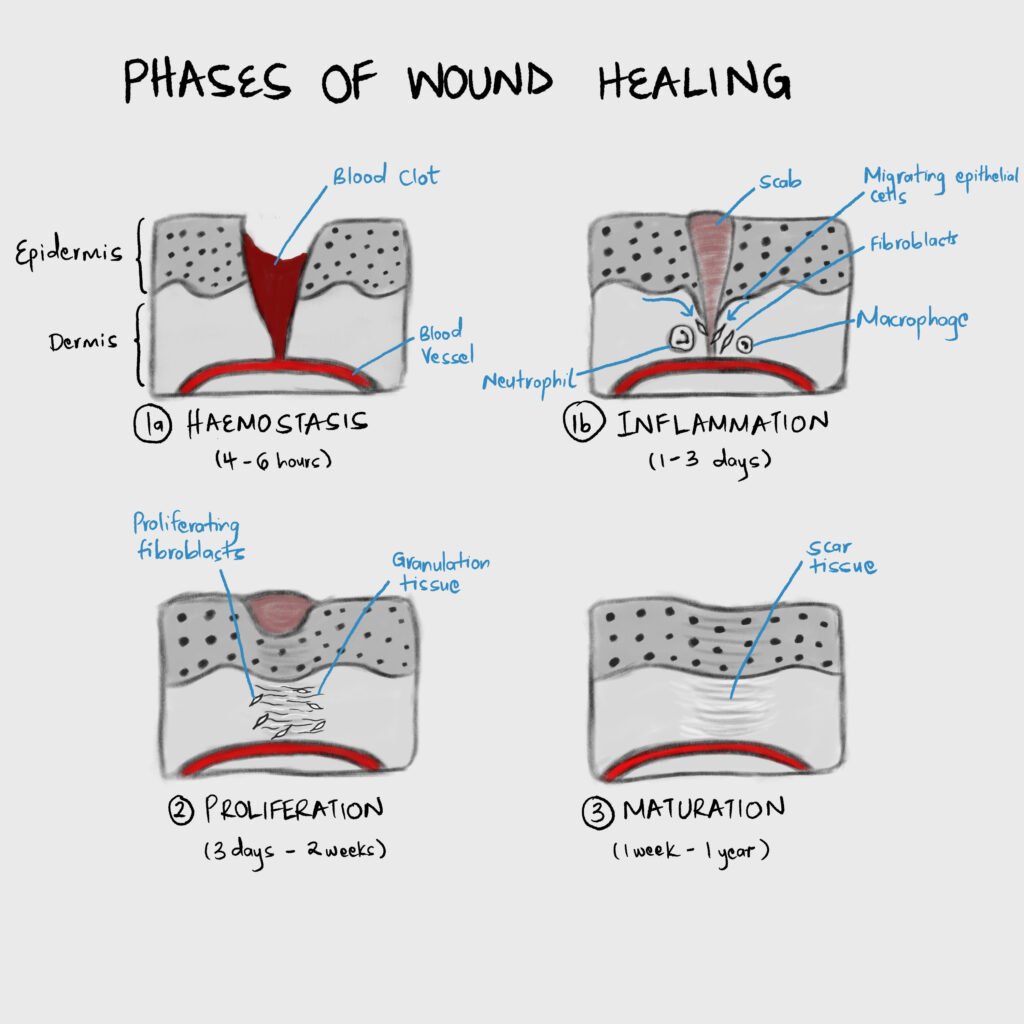
Hemostasis
Damage to tissue causes blood to fill the wound defect. When blood is exposed to collagen and Von Willebrand factor in the extracellular matrix platelets bind, aggregate and degranulate to release preformed granules that activate the coagulation cascade and mediate inflammation. Some of the mediators released by platelets during degranulation include Platelet-derived growth factor (PDGF), Transforming growth factor-B (TGF-B), Platelet-activating factor (PAF), Fibronectin, and Serotonin.
Inflammation
Various cytokines are released which stimulate the movement of cells to the site of inflammation/trauma.
Important Cytokines and Growth Factors
| Molecule | Origin | Effect |
|---|---|---|
| PDGF | Platelets, macrophages, monocytes, smooth muscle cells, endothelial cells | Collagen synthesis, angiogenesis, chemotaxis of fibroblasts, smooth muscle, monocytes, neutrophils |
| FGF | Fibroblasts, endothelial cells, smooth muscle cells, chondrocytes | Angiogenesis by chemotaxis of endothelial cells |
| Transforming Growth Factor-a | Keratinocytes, platelets, macrophages | Chemotaxis of endothelial cells |
| Transforming Growth Factor-B | Platelets, neutrophils, macrophages, lymphocytes, fibroblasts, keratinocytes | Wound matrix synthesis, Regulates inflammation, chemotaxis of neutrophils, macrophages, and lymphocytes |
| Vascular Endothelial Growth Factor (VEGF) | Macrophages, fibroblasts, endothelial cells, keratinocytes | Angiogenesis by mitosis of endothelial cells, pro-inflammatory |
| IL-1 | Macrophages, neutrophils, keratinocytes | Pro-inflammatory, angiogenesis, epithelialization and tissue remodelling |
| IL-4 | Neutrophils | Collagen synthesis |
| IL-6 | Fibroblasts, endothelial cells, keratinocytes | Pro-inflammatory, angiogenesis, epithelialization and tissue remodelling |
Cells involved in the inflammation stage
| Cell | Timeframe | Role | Essential for wound healing |
|---|---|---|---|
| Neutrophil | First to enter the wound within 6 hours due to increased vascular permeability. Numbers peak 24-48 hours from injury | Phagocytosis of bacteria and tissue debris. Also releases cytokines | No |
| Macrophage | Numbers peak within 48-96 hours and remain until the wound is healed | Phagocytosis and wound debridement. Regulates cell proliferation, matrix synthesis, and angiogenesis. Also activates other cells by releasing cytokines. | Yes |
| Lymphocyte | Appears about 5 days post-injury and peaks about 7 days | Not clear. However, decreased number of lymphocytes results in decreased wound strength and collagen content. | Yes |
Proliferation
In proliferation, the continuity of the underlying tissue is re-established through collagen deposition and matrix synthesis, and angiogenesis occurs. This happens over 3 days to 2 weeks post-injury. Characterized by formation of granulation tissue.
| Term | Definition |
|---|---|
| Granulation tissue | A loose extracellular matrix embedded with fibroblasts, inflammatory cells, and new capillaries. |

Cells involved in the proliferation stage
| Cell | Role | Role |
|---|---|---|
| Fibroblast | Recruited and activated primarily by PDGF, and other cytokines | Matrix synthesis (collagen and glycosaminoglycans) |
| Endothelial cells | Recruited and activated primarily by VEGF, and other cytokines | Migrates from venules near the wound to form new blood vessels (angiogenesis) |
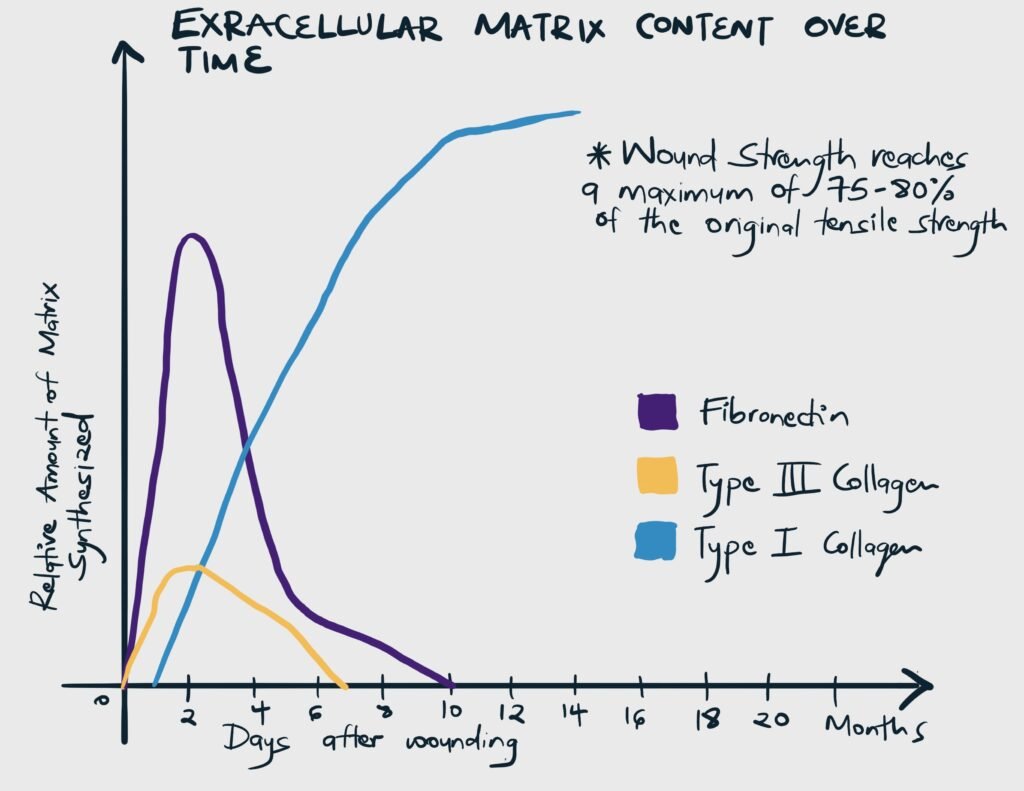
Substances involved in matrix synthesis
| Molecule | Role |
|---|---|
| Type I collagen | Deposition increases throughout the healing process. Responsible for the tensile strength of a scar (strength against tension) |
| Type III Collagen | Deposited early in the healing process and is gradually replaced by type I |
| Glycosaminoglycans (GAGs) | Examples include fibronectin, hyaluronic acid, dermatan, and chondroitin sulfate. They pair with proteins to form proteoglycans. Proteoglycans influence the arrangement and orientation of collagen. |
Remodeling and Scar Formation
Remodelling overlaps with proliferation since collagen reorganization occurs as soon as it is synthesized and deposited.
| Term | Description | Nota bene |
|---|---|---|
| Wound strength | The final tensile strength of the wound is determined by the quantity and quality of collagen deposited and maintained by an appropriate balance of collagen deposition and degradation. | The final strength of injured skin/scar always remains less than that of uninjured skin (on average about 70-80% of uninjured skin) |
| Wound contraction | The inward movement of the wound edge, resulting in reduced granulation tissue required to fill the wound, reduced area requiring re-epithelialization, and reduced scar volume. Primarily mediated by myofibroblasts and is promoted by TGF-B and PDGF. | Occurs to some degree in all wounds about day 5-15 post-injury. It is vital in wounds that heal by secondary intention. Becomes problematic when it impairs cosmesis and function. |
Epithelialization
This is a distinct phase of wound healing whereby the epithelial layer of the skin is restored. It begins within one day of injury and is complete within 48 hours in surgically approximated wounds (but takes longer in wounds left to heal by secondary intention). Basal cells detach from the dermis, enlarge, and migrate across the underlying matrix to cover the defect. Once they defect is bridged the cells rapidly divide and the surface layer is keratinized.



