Overview
| Condition | Pathogen |
|---|---|
| Laryngitis | Viral |
| Laryngotracheobronchitis | Parainfluenza virus |
| Spasmodic croup | Several viruses and allergic cause |
| Epiglottitis | Haemophilus influenza Type B; Gram + bacteria |
| Bacterial tracheitis | S. aureus |
| Foreign body obstruction | N/A (Foreign body) |
Laryngitis
Inflammation of the larynx. Corynebacterium diphtheria is a common cause in non-vaccinated individuals (will show up with whitish plaque in the back of the mouth). Diagnosis is clinical (rule out other diseases that cause voice loss).
Almost always caused by viruses (Rhinovirus, Parainfluenza virus, RSV, Adenovirus, Influenza virus, Measles virus, Mumps virus, VZV, Bordetella virus).
- Patient History
- Following non-specific URTI (common cold, chest congestion etc.)
- Signs and symptoms
- Hoarseness (out of proportion to presentaiton)
- Sore throat
- Cough
- Rhinorrhea
- Post-nasal discharge
- Fatigue
- Malaise
- Respiratory distress (in very very young patients, uncommon in older pts)
- Evidence of laryngeal edema (hypervascularity)
- Differentials
- Foreign body aspiration: Hx of aspiration; sudden onset
- Angioedema: Hx/FHx of angioedema; Trigger identifiable; Urticaria; Swelling of hands/feet; Respiratory distress
- Reflux laryngitis: Hx of GERD reported
- Diphtheria: Whitish-gray plaque visible on tonsils or oropharynx; Bull’s neck
- Retropharyngeal abscess: Drooling, dysphagia; does not improve w/typical laryngitis treatment
- Extrinsic compression: Does not improve with typical laryngitis treatment
- Investigations
- Oropharyngeal swab for culture: rule out URTI
- Treatment
- Humidified air (Nebulizer)
- Vocal rest
- Smoking cessation if pt smokes; Parents should stop smoking in the house if they do that
- Mucolytics (Guaifenesin) OTC
- PPR if reflux laryngitis is suspected
- Refer to ENT if Symptoms persists past 3 weeks (Chronic laryngitis)

Laryngotracheobronchitis (Croup)
Croup AKA laryngotracheobronchitis (may or may not extend to bronchi). More severe in young infants who have a narrower airway. Diagnosis is clinical provided the patient is stable. Consider other differentials is the patient is drooling, appears very ill, or if nebulization is ineffective at relieving sx.
Makes upto 15% of pediatric URTI Emergency Department visits. Peak incidence is 6 months to 3 years. M:F 1.4:1.
Causes are parainfluenza virus (80%). Other causes include adenovirus, RSV, enterovirus, human bocavirus, coronavirus, rhinovirus, echovirus, reovirus, metapneumovirus, influenza virus A and B. Rarely caused by measles virus, varicella and Mycoplasma pneumoniae.
- Patient History
- 6 months – 3 years old
- Inspiratory stridor following URTI
- Signs and Symptoms
- Sudden onset hoarsness and “seal-like” barking couagh
- Low-grade fever
- Insipratory or biphasic stridor (can involve the upper trachea)
- Variable levels of respiratory distress (cyanosis, suprasternal, intercostal, subcostal retraction, FAN)
- Lethargy
- Respiratory arrest
- Differentials
- Spasmodic (recurrent) croup: similar to croup but may have a prodrome, rarely has fever, may respond to nebulization
- Retropharyngeal abscess: drooling; neck pain; may be seen on radiograph
- Peritonsilar abscess: change in voice, neck pain, ear pain (referred); halitosis; deviation of uvula; no sudden; radiograph helps w/ddx
- Angioedema: swollen face, lips, feet, hands; urticaria; Hx/FHx
- Epiglotittis: Drooling, very ill, “sniffing position”, thumb-sign on radiographs
- Foreigh body: Hx, sudden-onset of drooling, respiratory distress, no systemic signs, may be seen on radiographs
- Trauma: Hx of trauma…
- Tracheomalacia: Congenital; associated anomalies such as GERD, Cardiovascular defects, developmental defects, TEF
- Investigations
- Complete Blood Count
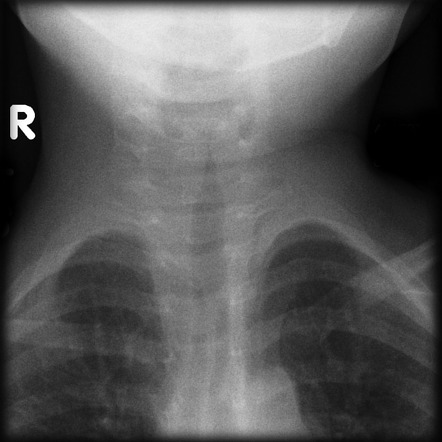
- AP and lateral neck radiograph:
- Steeple sign on AP (almost pathognomonic for Croup, also seen in bacterial tracheitis)
- Treatment
- Monitor pulse oximetry, HR, RR
- Manage pyrexia
- Fluids
- Supplemental oxygen as needed
- Dexamethasone and Nebulized racemic epinephrine (or salbutamol)
- Observe for at least 3 hours after administering epinephrine (or salbutamol)
Spasmodic Croup
Part of the differential diagnosis of croup. Shares similarities but key differences from croup. Causes: viral, allergens, psychogenic. Clinically inconsequential, Tx is reassurance and Sx based.
Croup vs Spasmodic croup
| Croup | Spasmodic croup | |
|---|---|---|
| Cause | Viral (Parainfluenza) | Viral, allergic, psychogenic |
| Signs and symptoms | Barking, cough, hoarseness, insp. stridor following URTI | Similar Sx but recurrent and short-lived |
| Timing | Worse at night | Worse at night |
| Fever | Low-grade | None |
| Diagnosis | Clinical or CXR | Dx of exclusion |
| Treatment | Respnds to nebulization and steroids | Often does not respond to nebulization/steroids |
| Complications | Hypoxia with complete obstruction | None |
Westley Score for Croup Severity
≤ 2 Mild Croup – Barking cough and hoarseness may be present, no stridor at rest
3-5: Moderate croup – easily heard stridor etc. but few other sx
6-11: Severe croup – obvious stridor, chest wall indrawing
≥ 12: impending respiratory failure
| Feature | 0 | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|
| Retractions | None | Mild | Moderate | Severe | ||
| Stridor | None | w/agitation | At rest | |||
| Cyanosis | None | w/agitation | at rest | |||
| Consciousness | Normal | |||||
| Air entry | Normal | Decreased | Markedly decreased |
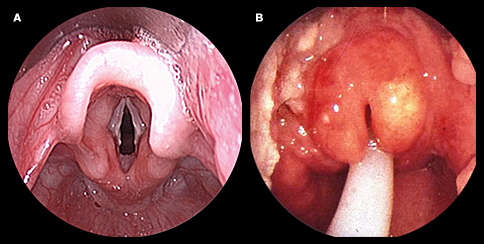
Epiglottitis
Most deadly upper airway disease. Epiglottitis is a true Pediatric/Medical EMERGENCY!. It is an acute inflammation of the supraglottic region of the oropharynx (epiglottis, vallecula, arytenoids, and aryepiglottic folds).
Caused by H. influenzae Type B (25% and declining), Haemophilus parainfluenzae, Streptococcus pneumonia. Other causes include GAS, GCS, Neisseria meningitidis, Pseudomonas spp., Moraxella catarrhalis, Klebsiella spp., Pasteurella spp., Candida albicans. Non-infectious causes include thermal, caustic, trauma, post-foreign body ejection, and Head and Neck chemotherapy.
- Patient History
- 2-6 years of age
- Sudden onset of symptoms
- No prodromal symptoms
- H/O of recent viral infection (URTI)
- Signs and symptoms
- Fever (first Sx)
- Dysphagia
- Refusal to feed
- Muffled/hoarse “hot potato” voice
- Sore throat
- Anxiety
- Pt appears toxic (shock can appear early)
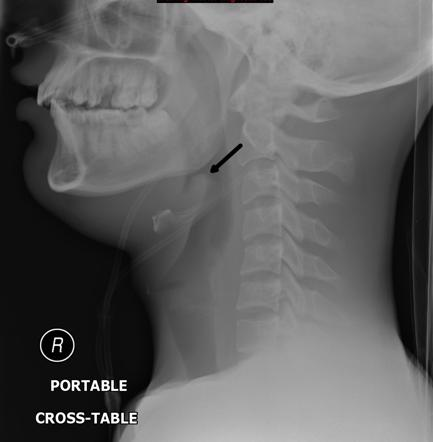
- “Sniffing/Tripod position” (leanign forwards, chin hyperextended)
- Mouth open
- Protruding tongue
- Drooling
- Stridor
- Accessory muscle use
- Respiratory distress
- Cyanosis
- Tender LAN
- Investigations
- CBC
- BMP
- Cultures
- Portable Lateral Neck XR (do not send child to radiology): Thumb sign
- Laryngoscopy
- Treatment
- Secure airway (Intubate; even in pts who aren’t in distress once Dx is made )
- Avoid procedures until the airway is secured
- Admit to ICU
- Consult anesthesiology, ENT, or Surgery as necessary
- Avoid supine position (may precipitate respiratory arrest)
- Keep emergency cart by bedside
- IV antibiotics: 3rd or 4th gen cephalosporins (Ceftriaxone, Cefotaxime, Cefuroxime)
- D51/2NS until oral feeds can be tolerated
- Extubate 24-48 hours provided there are signs of resolutions (decreased erythema, edema, air-leaks around ET tube)
- Discharge after 24 hours if afebrile and stable
- Contacts should get Rifampin
Differences between Epiglottitis and Laryngotracheobronchitis (LTB)
| Epiglottitis | LTB | |
|---|---|---|
| Causative organism | H. influenzae | Parainfluenza |
| Age of presentation | 2 – 6 years | 6 months – 3 years old |
| Prodromal symptoms | Absent | Present |
| Onset | Sudden | Gradual |
| Fever | High-grade | Low-grade |
| Toxic appearing | Yes | No |
| Cough | Absent | Barking |
| Drooling | Present | Absent |
| X-ray | Thumb sign on lateral view | Steeple sign on PA view |
| Management | Requires intubation and admission to the ICU, IV antibiotics, Rifampin | Racemic Epinephrine and Dexamethasone |
Bacterial Tracheitis
Bacterial tracheitis is diffuse infection and inflammation of the larynx, trachea, and bronchi, wih the major point being at the cricoid cartillage level. Presents as coup (barking cough, stridor, fever in a pt <3 years of age) but won’t respond to racemic epinephrine (and will have a high-fever). Presume S. aureus until cultures show otherwise. Can be a superinfection following viral infection or trauma (intubation).
Incidence is low – 0.1/100,00. Mortality of 4-20%. M:F 2:1. Rare but more common than acute epiglotitis.
- Pathogens
- S. aureus (consider CA MRSA)
- S. pyogenes
- S. pneumoniae
- M. catarrhalis
- Patient History
- High Fever
- URTI “prodrome”
- Intubation for other purposes
- Signs and symptoms
- High fever
- Dyspnea
- Barking cough
- Hoarseness
- Stridor
- Sore throat
- Variable but progressive respiratory distress (AROM use → FAN → Cyanosis → Lethargy)
- Often appears toxic (septic due to bacteria; does not happen in croup)
- No drooling (rule out epiglottitis)
- Investigations
- Portable AP/Lateral Neck XR: distinguish from croup; provided the patient is stable
- Steeple sign
- Narrowing of the airway
- Clouding of the air column
- Laryngotracheoscopy: most accurate test. Used for definitive diagnosis via tracheal toilet, strip purulent membranes
- Purulent
- Pseudomembrane
- CBC
- BMP
- Blood cultures
- Portable AP/Lateral Neck XR: distinguish from croup; provided the patient is stable
- Treatment
- Intubate if respiratory distress is present (use smaller size tube)
- Cardiorespiratory monitoring for all pts
- Admit to PICU
- IV fluids
- Empitic IV antibiotics targeting staph
- 3rd gen cephalosporin (Cefotaxime, Ceftriaxone) AND a PCNase resistant PCN (Oxacillin, Nafcillin)
- If CA-MRSA is endemic locally use Vancomycin +/- Clindamycin
- Consult ENT



Foreign body obstruction
Children < 3 years of age account for ~ 73% of all cases. Most common location of obstruction is the right bronchus (58%). Incomplete obstruction is usually followed by an asymptomatc interval where the foreign body becomes lodges, reflexes are diminished and the patient becomes more comfortable. This is where non-diagnosis or misdiagnosis is common. If index of suspicion is high go straight to bronchoscopy.
Laryngeal foreign body: leads to complete obstruction and asphyxiation/death unless Heimlich manoeuvre is performed. Usually, a flat thin object (coin) lodged between vocal cords sagittaly.
- Most common aspirated objects
- Nuts (peanuts; 1/3 of cases)
- Raw carrot
- Apple
- Dried beans
- Popcorn
- Sunflower seeds
- Watermelon seeds
- Small toys/parts
- Patient History
- Sudden coughing, respiratory distress
- What was around the patient when signs and symptoms started?
- What has the patient been fed? (particularly ask about nuts)
- Symptoms of incomplete obstruction
- Violent paroxysms of couging
- Gagging
- Wheezing
- Drooling
- Symptoms of laryngeal foreign body
- Asphyxiation
- Manifests as “croup”
- Hoarseness
- Stridor
- Cough
- Dyspnea
- Symptoms of Tracheal foreign body
- Choking reflex (90%)
- Stridor (60%)
- Wheezing (50%)
- Symptoms of Bronchial foreign body
- Unilateral wheeze
- Investigations
- AP/Lateral neck radiograph
- Expiratory chest radiograph
- Air trapping
- Mediastinal shift from affected side
- Treatment
- Decompress stomach via NG tube (prevent aspiration)
- Provide IV fluids
- Perform rigid bronchoscopic extraction of foreign body
- Complications of incomplete obstruction
- Obstruction
- Erosion
- Infection (fever, cough, hemoptysis)
- Pneumonia
- Atelectasis
- Complications of complete obstruction
- Asphyxiation
- Sudden respiratory distress → inability to speak or cough
- Globular objects are more frequent offenders of complete obstruction
- Asphyxiation



