Basic Anaesthetic Monitoring
ASA has prescribed standards for basic anaesthetic monitoring.
| Standard | Statement |
|---|---|
| Standard I | A qualified anaesthesia personnel shall be present in the room throughout the conduct of all general anaesthetics, regional anaesthetics and monitored anaesthesia care |
| Standard II | During all anaesthetics the patient’s oxygenation, ventilation, circulation and temperature shall be continually evaluated. |
Continuous vs. continual measurement
| Term | Definition |
|---|---|
| Continual | Repeated regularly and frequently in steady rapid succession e.g. BP measured q 5min |
| Continuous | Prolonged without interruption at any time e.g. EKG monitoring, disconnect alarm, presence of anesthesia personnel |
Summary of basic anaesthetic monitoring
| Parameter | Monitors |
|---|---|
| Oxygenation | Inspired gas FiO2 analyzer + low O2 concentration alarm, Pulse oximetry with variable pitch tone |
| Ventilation | Capnography (with expired Vt), Disconnect alarm if mechanically ventilated |
| Circulation | 3 lead or 5 lead EKG, Blood pressure q5min + at least one of these: pulse oximetry tracing, a-line tracing, palpable pulse, auscultation, doppler |
| Temperature | Temperature probe if clinically significant changes in body temperature are anticipated |
Pulse oximetry
The probe of a pulse oximeter emits light at a wavelength of 660nm (red = Deoxyhemoglobin -Hb) and 940 nm (Infrared = Oxyhemoglobin – O2Hb). Sensors detect the light that passes unabsorbed at each wavelength. A process known as photoplethysmography is used to identify arterial flow (as alternating current = AC) and light absorption during non-pulsatile flow (as direct current = DC). The ratio (R) of AC/DC at 660nm and 940nm is used to derive the SpO2. A ration (R) of 1:1 = SpO2 of 85% (hence why a pulse oximeter that is not connected to the patient reads 85%)
| Hemoglobin | Absorption |
|---|---|
| Oxyhemoglobin (O2Hb) | Absorbs more infrared light (940nm) and allows more red light to pass |
| Deoxygemoglobin (Hb) | Absorbs more red light (660nm) and allows more infrared light to pass through |
| Measurement | Formula |
|---|---|
| SaO2 (Fractional Oximetry) | O2Hb/(O2Hb + Hb + MetHb +COHb |
| SpO2 (Functional/Pulse Oximetry) | O2Hb/(O2Hb + Hb) |
- When is cyanosis clinically apparent?
- With 5 g/dL of desaturated hemoglobin
- What factors produce a “falsely” elevated SpO2?
- Carbon monoxide poisoning (Carboxyhemoglobin)
- Cyanide toxicity
- What factors produce a falsely low SpO2
- Dyes (Methylene blue > indocyanine green > indigo carmine)
- Blue nail polish
- Shivering/other motion
- Ambient light
- Malpositioned sensor
- Low perfusion
- What factors do not affect SpO2?
- Bilirubin (Jaundice)
- HbF
- HbS
- Acrylic nails
- Fluorescein dye
Methemoglobin (MetHb)
MetHb has similar light absorption at 660nm and 940nm (R = 1:1 ratio). At high levels, SpO2 approaches 85%, while PaO2 remains normal on ABG.
- Causes of MetHb
- Prilocaine/benzocaine topicalization
- Metoclopramide
- Dapsone
- Nitric oxide
- Nitroglycerine
- Treatment of MetHb
- Methylene Blue
- Vitamin C (in G6PD deficiency)
Carboxyhemoglobin (COHb, Carbon Monoxide poisoning)
COHb has a similar absorbance to O2Hb (940nm). Carbon monoxide has a higher affinity to Hb than O2. At 50% COHb, SpO2 reads 95% despite a low SaO2 (50%) on ABG, thus producing a falsely high SpO2.
- Causes of COHb (Carbon monoxide poisoning)
- Smoke inhalation
- Volatile anaesthetic degradation
- Desiccated baralyme/soda lime
- Treatment of COHb (Carbon monoxide poisoning)
- 100% FiO2
- Hyperbaric O2
Cyanide Toxicity
In cyanide toxicity, Hemoglobin remains oxygenated, but tissues cannot use it. Cyanide toxicity is clinically diagnosed when a patient has cyanosis despite a high SpO2. ABG and VBG will also have similar PO2 due to the uncoupling of oxidative phosphorylation, while lactate will be elevated.
- Causes of cyanide toxicity
- Sodium nitroprusside
- Smoke inhalation
- Treatment of cyanide toxicity
- Hydroxocobalamin (previously sodium/amyl nitrite was used)
Circulation
Electrocardiogram (EKG)
| System | Leads |
|---|---|
| 3-Electrode System | 3 Limb leads: RA (white), LA (black), and LL (red). Monitors Leads I, II, and III. Placed on limbs, or on chest equidistant from teh heart |
| Modified 3-Electrode System | LA lead is moved to V5 position. Lead I is monitored if there is a concern for anterior wall ischemia |
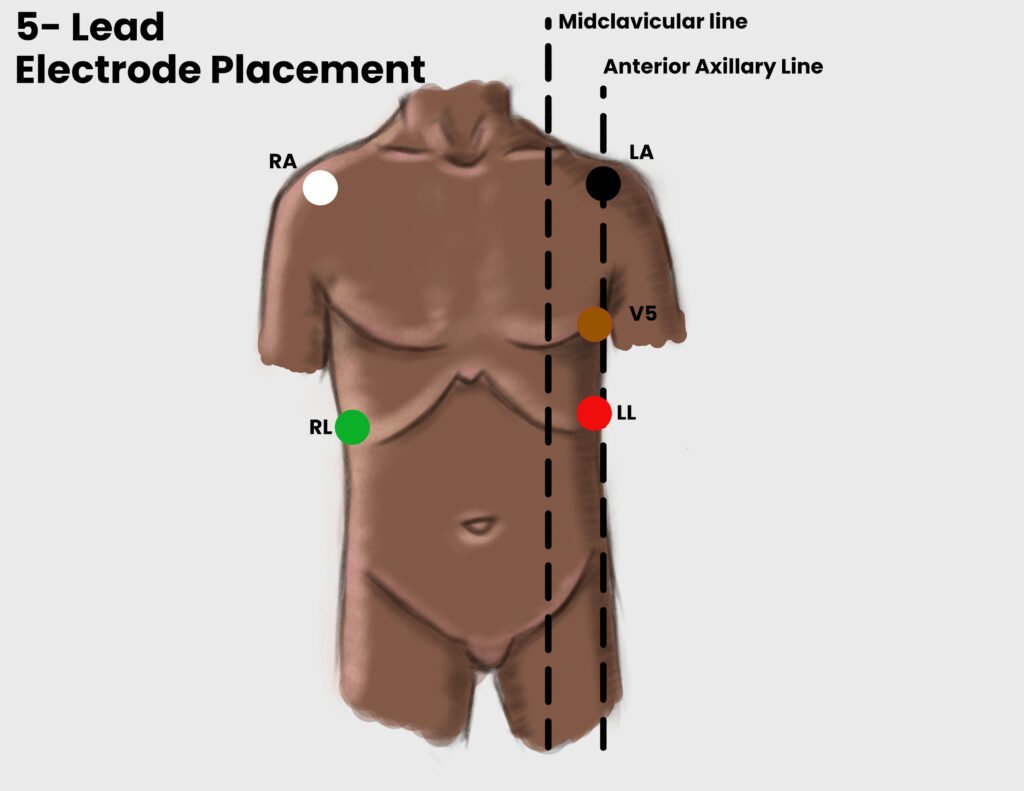
| 5-Electrode system | 3-limb leads, and LL (green), and V5 leads (brown). Allows monitoring of 7 leads simultaneously. The green lead is the reference point/ground, traditionally placed on the RL but can be placed anywhere on the body away from the other leads. |
Sensitivity for detecting ischemia
| Leads | Sensitivity |
|---|---|
| V5 | 75% |
| II + V5 | 80% |
| II + V4 + V5 | 98% |
- Mnemonic to remember positioning of electrodes
- Smoke over fire (black lead over red lead)
- Clouds over grass (white lead over green lead)
- White on the right (white lead on the right)
- Which lead is most sensitive for detecting atrial arrhythmia?
- Lead II
- What are the advantages and disadvantages of a 3-lead EKG?
- Advantage: Good for detecting atrial arrhythmia (Lead II) and R wave changes
- Disadvantage: Poorly sensitive for ST segment changes
- What are the advantages of a 5-lead EKG?
- Addition of V1 to enhances detection of Atrial Arrhythmia
- Addition of V4 and V5 improves detection of ischemic events
Non-invasive Blood Pressure (NIBP)
NIBP is measured by a NIBP cuff. MAP is the primary measure and SBP and DPB are derived from algorithms. The cuff should encircle > 80% of the extremity and the cuff width should be > 40% arm circumference.
- Consequence of a cuff that is too small
- Falsely High BP
- Consequence of a cuff that is too big
- Falsely low BP
Invasive Blood Pressure (IBP)
IBP is measured using an intra-arterial catheter and pressure transducer.
Setting up the transducer
| Term | Definition |
|---|---|
| Zeroing | Exposes the transducer to air-fluid interface, thus establishing Patm as the “zero” reference for pressure |
| Levelling | Assign the zero reference point to a specific point on the patient. By convention, the transducer is “levelled” at the right atrium. Can be leveled at the Circle of Willis in neurosurgical cases to assess cerebral perfusion. |
- Indications for IBP
- Moment-to-moment BP changes anticipated (when rapid detection is vital)
- Planned pharmacologic or mechanical manipulation of BP
- Repeated blood sampling
- Failure of NIP (due to positioning – arms tucked, lateral positioning with up arm and down arm)
- To provide supplementary diagnostic information e.g. pulse pressure variation to guide volume status
Arterial line tracings
The further from the aorta, the later the dicrotic notch, the higher the systolic pressure (and widened pulse pressure), and MAP is unchanged.
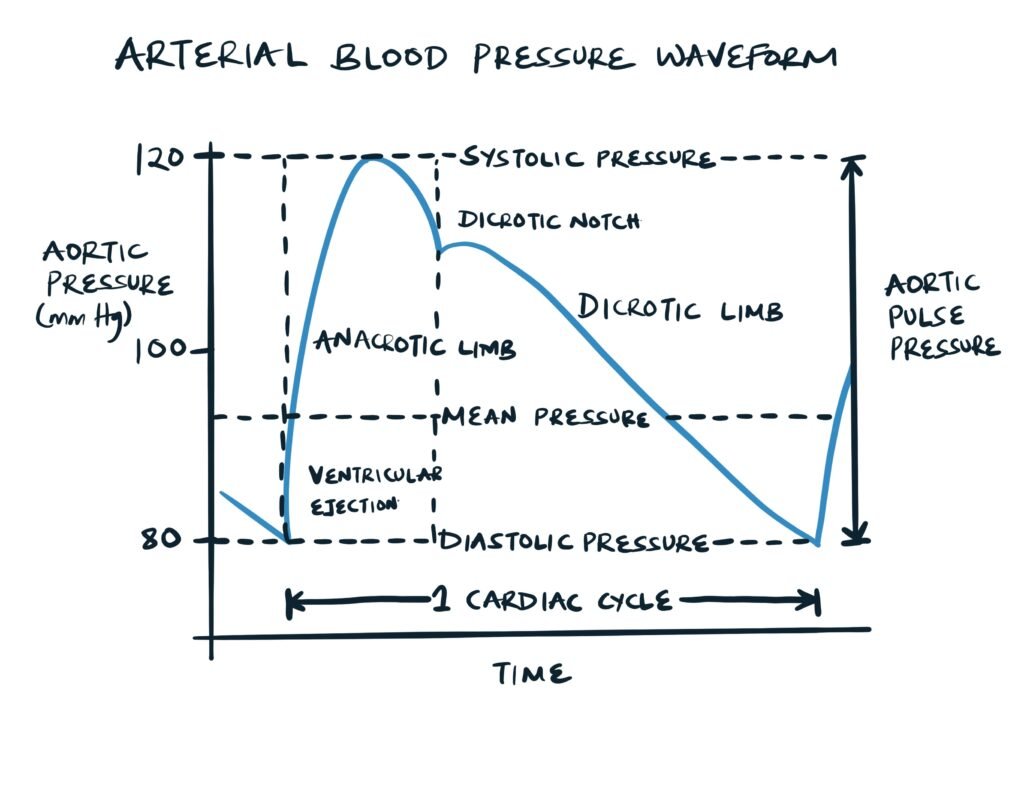
Pulse Pressure Variation
Variation in pulse pressure on arterial tracing can guide volume resuscitation.
- How does pulse pressure change in spontaneously ventilating patients?
- It decreases
- How does pulse pressure change with increased stroke volume?
- It increases
- How does pulse pressure change with decreased vessel wall compliance?
- It increases
Effect of patient and transducer position on BP Measurement
Blood pressure varies by position. A change in pressure (”p”) of 7.4 mmHg coincides with “H” change of 10 cm (Mnemonic: pH 7.410).
- When a patient is seated in beach chair position, the BP cuff on the leg reads 120/80 mmHg. But if the brain is 60cm vertically higher than the cuff, what is the BP in the brain?
- Close to 75/35 mmHg
Ventilation
Capnography (etCO2)
Capnography measures exhaled CO2. The sampling rate is 50-500 ml/min.
- 3 reasons why ETCO2 may drop
- Decreased elimination of CO2: acute cardiovascular collapse (reduced cardiac index), massive venous air embolism (increased ET nitrogen), large pulmonary embolism (with ECG showing S1, Q3, T3), kinked or dislodged or esophageal endotracheal tube
- Decreased production of CO2: hypothermia, hypothyroidism, neuromuscular blockade
- Circuit sampling line disconnect
- How much does ETCO2 increase when apnoeic?
- 6 mmHg after 1 minute
- 3 mmHg every minute thereafter
- How does hypotension affect EtCO2
- Causes a significant drop
- How does pulmonary embolism affect EtCO2?
- Decreases EtCO2 but increased A-a gradient between ETCO2 and PaCO2
- What is the goal of ETCO2 during CPR?
- 10
- If there is a sudden increase in ETCO2 return of spontaneous circulation is likely
- What trace does bronchospasm have on capnography?
- An upsloping trace
Capnography phases
| Phase | Event |
|---|---|
| I | Dead space gas is exhaled |
| II | Transition between dead space and alveolar gas |
| III | Alveolar Plateau |
| IV | Inspiration |
Spontaneous ventilation, Mechanical ventilation, Prolonged exhalation (spontaneous), Emphysema (upsloping plateau), Sample line leak, Exhausted CO2 absorbant, Cardiogenic oscillation, Electrical noise
Temperature
- What is the major mechanism of heat loss with general anesthesia?
- Redistribution: Vasodilation causes blood to shift from the core to the periphery
- Radiation is second
- Others: Conduction, convection, and evaporation
Core temperature monitoring
| Site | Description |
|---|---|
| Pulmonary artery | “Core” temperature – Gold Standard |
| Tympanic membrane | Correlates well with core; approximates brain/hypothalamic temperature |
| Nasopharyngeal | Correlates well with core and brain temperature. Can get refractory epistaxis if there is coagulopathy |
| Oropharynx | Good estimate of core temperature. Correlates with tympanic and esophageal temperatures |
| Esophagus | Correlates well with core. Avoid with esophageal varices |
Temperature monitoring that correlates less with “core” temperature
| Site | Description |
|---|---|
| Bladder | Approximates “core” when urine flow is high. Delay between bladder temperature reading and true temperature |
| Axillary | Inaccurate. Varies by skin perfusion |
| Rectal | Innacurate. Temperature is affected by venous return, enteric organisms and insulation by stool |
| Skin | Inaccurate. Varies by site |
Other Monitors
| Parameter | Monitors |
|---|---|
| Depth of anaesthesia | Bispectral index (BIS) monitor/Sedline |
| Circulation/Fluids | Pulmonary Artery Catheter +/- Continuous cardiac output, Central venous pressure (CVP), Intracranial pressure (ICP), Transesophageal echo (TEE), Precordial doppler (if the risk of air embolus is high), Cerebral oximetry (NIRS), Esophageal stethoscope, Foley, Orogastric tube |
AAAAAh!! I just Intubated (A’s)
- Airway (ETT secured and ventilator settings)
- Anaesthesia (volatile, infusions)
- Access (arterial line, peripheral IV, central venous catheter etc.)
- Another thing in the mouth (orogastric tube, bite block, TEE probe)
- Arms (patient positioning)
- Air (forced air, Bair Hugger + temperature probe)
- ABG (check baseline ABG)
- Antibiotics
- Analgesia (redose pain medication prior to incision)




