Overview
Shock is defined as a state of global cellular and tissue hypoxia due to either reduced oxygen delivery, increased oxygen consumption, inadequate oxygen utilization, or a combination of these processes. Shock is almost always caused by low blood pressure leading to reduced organ perfusion and invariably death. However, multiple mechanisms can lead to shock. It is important to note that not all patients with hypotension are in shock, and not all patients with shock have hypotension.
Types of shock
Other forms of shock
| Type of Shock | Pathophysiology | Common causes |
|---|---|---|
| Hypovolemic shock | Low preload due to reduced intravascular volume | Hemorrhagic shock, Non-hemorrhagic hypovolemic shock (diarrhoea, vomiting, burns) |
| Cardiogenic shock | Low contractility | Acute MI, Acute valve dysfunction, Cardiomyopathy, Arrhythmia, Myocarditis, Congestive Heart Failure exacerbation |
| Obstructive shock | Low preload de to reduced venous return to the left ventricle | Tension pneumothorax, Massive Pulmonary embolus, Cardiac tamponade |
| Distributive shock | Low systemic vascular resistance | Septic shock, Anaphylactic shock, Neurogenic shock |
| Special term | Definition |
|---|---|
| Undifferentiated shock | When a patient is recognized to be in shock but the type of shock is unknown |
| Arrhythmogenic shock | Low heart rate and low preload due to short diastolic filling time |
| Toxin-mediated shock | Cyanide poisoning, carbon monoxide poisoning |
| Endocrine shock | Addisonian crisis, Hyperthyroidism, Hypothyroidism |
- Pathophysiology of shock
- In general, low perfusion pressure is due to low preload, low contractility, low heart rate, and low systemic vascular resistance.
- There is global tissue hypoxia which increases serum [lactate], causes Na+/K+ pump failure, release of autolytic enzymes from lysosomes, and hyperkalemia
- There is also activation of the immune and coagulation system which may lead to Disseminated Vascular Coagulation
- The RAAS is activated resulting in increased sodium and water reabsorption
- There is also increased sympathetic tone causing increased pulse rate and total peripheral resistance
Stages of shock
| Stage | Description |
|---|---|
| Hypoperfusion and hypoxia | Anaerobic metabolism and Lactic acidosis |
| Compensation | Neuroendocrine response maintains perfusion to vital organs |
| Decompensation | Compensatory mechanisms fail |
| Irreversible shock | Cellular ATP metabolism is completely lost leading to Multi-organ dysfunction and multi-organ failure |
- Compensated vs uncompensated shock
- Compensated shock
- Initial stage of shock when a series of compensatory mechanisms are able to counter the decrease in tissue perfusion.
- Compensatory mechanisms (e.g., increased heart rate, increased heart contractility, and/or vascular constriction) are able to maintain cardiac output and blood pressure, thereby ensuring perfusion to vital organs
- Damage to the tissues and organs may be reversible and further deterioration can be prevented if shock is addressed during the compensated stage.
- Decompensated shock
- the cause of shock is not addressed promptly, and compensatory mechanisms may become overwhelmed and unable to support adequate tissue perfusion
- signs and symptoms of organ dysfunction begin to appear (e.g., decreased urination, confusion, cold and clammy skin, irregular heart rhythms, etc.)
- Damage to the tissues becomes irreversible.
- If shock persists for too long, vital organs such as the brain, heart, and kidneys may begin to shut down, leading to multiple organ failure.
- Compensated shock
- General signs and symptoms of shock
- Altered mental status: Agitation → Delirium → Somnolence → Loss of consciousness. Due to decreased blood flow to the brain.
- Tachypnoea and Hypoxaemia
- Tachycardia: Early stages, help to maintain normal BP, especially in hypovolemic shock. Anyone with a normal heart will become tachycardic in shock.
- Hypotension (SBP < 90mmHg or MAP < 60 mmHg or drop in SBP > 30 mmHg)
- Weak or absent pulse: Decreased flow to the periphery
- Cool extremities: Decreased flow to the periphery
- Weak peripheral pulses: Decreased flow to the periphery
- Decreased urine output: Decreased flow to the kidney
- Lab values that may be altered in shock
- Elevated Lactate and Decreased Bicarbonate
- Elevated Troponin
- Elevated Bilirubin and Transaminases (AST and ALT): shock liver
- Elevated Creatinine
General Treatment of Shock
Priorities in the management of shock include ventilation, oxygenation, pulse, fluids (unless cardiogenic shock), and pressure. Fluid resuscitation is the rapid delivery of fluids to patients with acutely disturbed hemodynamics. Conventionally, IV fluids are given if the MAP < 60-65 mmHg (or CVP < 8 mmHg) provided there are no signs of cardiogenic pulmonary edema. If the patient is fluid-responsive, their cardiac output should increase by at least 15% after receiving a 500mL fluid bolus. The surviving sepsis campaign recommends norepinephrine as the first choice vasopressor.
Categories for the treatment of shock
| Treatment | Effect |
|---|---|
| IV fluids | Increases central venous pressure |
| Ionotropes | Increases contractility |
| Vasopressors | Increases systemic vascular resistance |
Types of shock and their treatment
| IV fluids | Vasopressors | Ionotropes | |
|---|---|---|---|
| Hypovolemic | Yes | Temporary | No benefit |
| Distributive | Yes | Yes | Yes/No |
| Cardiogenic | Contraindicated | Contraindicated | Yes |
| Obstructive | Yes/No (temporary) | Yes/No (temporary) | Yes/No (temporary) |
First-line Inotropes and Pressors for shock
| Shock type | First line agents |
|---|---|
| Septic shock | Norepinephrine OR phenylephrine |
| Refractory septic shock | Vasopressin OR Epinephrine |
| Cardiogenic | Dobutamine +/- dopamine OR Dopamine OR Norepinephrine +/- dobutamine |
| Hypovolemic shock | IV fluids only; no prolonged use of pressors |
| Mixed septic and cardiogenic shock, or undifferentiated shock | Norepinephrine, Epinephrine, Dopamine |
- General management of Shock
- Airway
- Maintain patency through maneuvers, adjuncts, supraglottic airway, or definitive airways
- Breathing
- 15L/min 100% Oxygen via NRB to keep SpO2 > 94%
- Circulation
- Control bleeding
- Bilateral Large bore IV lines (16G) and IV fluid bolus
- Blood type; O- blood should be on hand (nobody will react to this)
- Maintaining adequate BP is critical (aim 100/70)
- Vasopressor and Inotropic support can be considered for distributive and cardiogenic shock
- IV norepinephrine 5-20ug/kg/min (for septic shock)
- IV dopamine 5-10 ug/kg/min
- IV dobutamine 5-10 ug/kg/min (for cardiogenic shock)
- Adjuncts
- Insert foley to monitory Urine Output (> 0.5 mL/KG urine output = good volume)
- Monitor HR, BP, RR, Temperature and SpO2
- Evaluate and Correct the underlying cause
- AMPLE history
- The FAST exam is useful for intracavitary bleed
- Chest decompression Tension Pneumothorax is suspected
- Airway
Hypovolemic shock
Hypovolemic shock is a common cause of shock in the setting of trauma. Due to VOLUME LOSS (External or internal). The index of suspicion should be very high since bleeding is common in trauma (obvious when external…but is the patient bleeding internally?)
- Common causes of hypovolemic shock
- External or internal haemorrhage
- Dehydration
- Burns
- Vomiting and Diarrhoea
- Diuresis
- Sites of bleeding ***Internal bleeding can be detected using FAST
- Thoracic cavity
- Abdominal cavity
- Pelvis
- Long-bones
- External bleeding (on the floor)
- How much blood can the body lose before symptoms start to manifest?
- 15-20% of volume (750mL – 1L)
- Can lose 15% because it is reserve volume
- Signs and symptoms
- Pallor
- Cold clammy skin (due to peripheral vasodilation)
- Tachycardia
- Reduced JVP
- Investigations
- CBC
- HCT: useful for acute haemorrhage but unreliable
- U/E/Cs: workup for AKI
- Coagulation Panel: workup for DIC
- Arterial Blood Gases: for metabolic acidosis, elevated lactate and base deficit
- Group and Crossmatch (with 6 units on hand)
- B-hCG: rule out ruptured ectopic in women
- ECG and CXR: if there is associated chest pain or breathlessness
- Urinalysis: after placing foley
- CVP: to guide fluid resuscitation
- CBC
- Treatment
- 1L crystalloid (Ringers Lactate, Hartmans) push within 1 hour
- Assess response to resuscitation
- Can consider colloid or whole blood
ACS Tennis staging for hypovolemia
| Stage 1 | Stage 2 | Stage 3 | Stage 4 | |
|---|---|---|---|---|
| % volume lost | ≤ 15% | 15-30% | 30-40% | ≥ 40% |
| Volume lost (mL) | <750 | 750-1500 | 1500-2000 | ≥ 2000 |
| Systolic Blood Pressure (mmHg) | Normal | Normal | < 100 | < 70 |
| Heart Rate (bpm) | <100 | > 100 | >120 | > 140 |
| Respiatory rate (breaths per minute) | 12-20 | 20 – 30 | >30 | > 30 |
| Mental status | Normal | Normal/Anxious | Confused, Anxious, Agitated | Lethargic, Coma |
| Urine output (ml/hr) | > 30 | 20-30 | < 20 | Absent |
| Other Sx | Subjective feelings of thirst; pallor | Pallor; Delayed cap refill | Pallor; Restlessnessl Oiguria | Pallor; Air hunger, Collapse Anuria |
| Base deficit | 0-2 mEq/L | 2-6 mEq/L | 6-10 mEq/L | 10 mEq/L |
| Blood Products | Observe | Consider Blood Products | Blood Transfusion | Massive Blood Tranfusion |
Obstructive Shock
Cardiac tamponade
Cardiac tamponade is the accumulation of blood in the pericardial space reducing the heart’s pumping ability and diminishing CO. More common in penetrating thoracic injury than blunt injury.
Acute form: Lose blood quickly, commonly chest trauma
Chronic form: lose blood slowly, not commonly seen in trauma
- Signs and symptoms
- Tachycardia
- **Jugular Venous Distension (**JVD helps to differentiate this from hypovolemia)
- Breath sounds normal bilaterally on auscultation (differentiates from pneumothorax)
- Heart sounds muffled or distant
- Pulsus paradoxus (≥ 10mmHg drop on inspiration)
- EKG findings if attached: decreased QRS amplitude, ST changes
- Investigations
- Sonography (FAST): for pericardial fluid
- Treatment
- Pericardiocentesis
Tension pneumothorax
Disruption of tissue causes progressive accumulation of air in the pleural space (one-way valve mechanism). The mediastinal shift causes compression of the IVC at the diaphragm which reduces preload and cardiac output. Diagnosis is clinical
- Signs and symptoms
- Dyspnea, SOB (Patient is not breathing well…), air hunger
- Jugular Venous Distension
- Absent breath sounds on the affected side (Differentiate from tamponade)
- **Hyperresonant to percussion on the affected side (**Differentiate from tamponade)
- Tracheal shift
- Subcutaneous emphysema
- Investigations
- DO NOT WAIT FOR CXR IF SIGNS ARE PRESENT/ IF THERE IS A HIGH INDEX OF SUSPICION
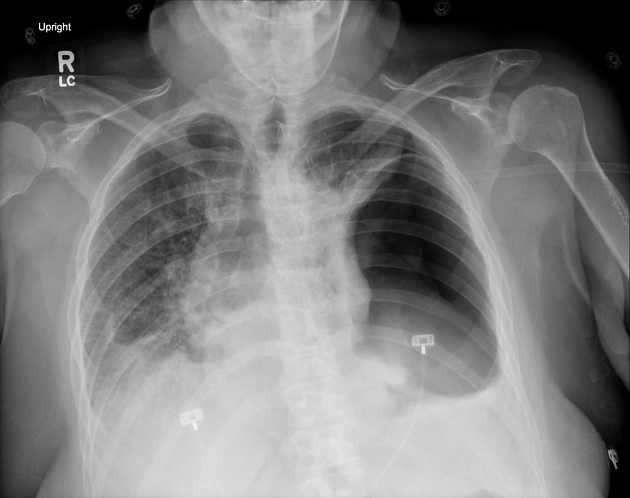
- CXR: Loss of pulmonary/vascular markings on the affected side (demonstrates collapse)
- Treatment
- Immediate NEEDLE OR FINGER DECOMPRESSION followed by CHEST-TUBE PLACEMENT
Other causes not trauma mediated
Cardiogenic shock
Decreased BP due to impaired pumping ability of the heart.
- Causes
- Myocardial infarction
- Arrhythmia
- Cardiomyopathy
- Valve dysfunction
- Investigations
- ECG
- Troponin T and CK-MB
- Treatment
- Refer to ACLS in the cardiology section
Distributive shock
Septic shock
Decreased BP due to the release of inflammatory mediators resulting in widespread vasodilation. The majority of blood volume is in the peripheral circulation (should normally be in the splanchnic vasculature)
FEVER, SKIN IS COLD AND CLAMMY**
| Term | Definition |
|---|---|
| Sepsis | SIRS + documented infection |
| Severe sepsis | Sepsis + evidence of end-organ dysfunction (hypotension, oliguria, elevated lactate) |
| Septic shock | Severe sepsis + refractory hypotension |
- SIRS criteria ≥ 2 of the following
- Hyperthermia or Hypothermia> 38 C or < 36 C
- Tachycardia > 90 bpm
- Tachypnoea > 20 breaths per min
- WCC > 12k or <4K or > 10% left shift
- Signs and symptoms
- Flushed and Warm periheries
- Hypotension
- Tachycardia
- Tachypnoea
- Bleeding (due to clotting dysfunction – DIC?)
- Physical exam determine the source of infection
- Indwelling catheter?
- Gallbladder disease? (Murphy sign)
- Peritonitis? (Guarding, Board-like rigidity, Percussion tenderness, Rebound tenderness)
- Pneumonia? (Respiratory distress, Consolidation)
- Appendicitis? (Blumberg’s sign, Pointing sign etc.)
- Investigations
- CBC: Leukocytosis
- U/E/Cs: evaluate for AKI
- Coagulation panel: evaluate for DIC
- Blood culture and sensitivity (obtain from 2 different sites)
- Arterial Blood Gas
- Chest XR: Pneumonia, ARDS
- EKG
- Urinalysis and Urine MCS: r/o UTI
- Treatment
- Circulation
- Push 1-2L of crystalloids
- Insert Central Line
- Consider Noradrenaline or Dopamine
- Antibiotics
- For immunocompetent patients: Cefriaxone or Ciprofloxacin
- For immunocompromised patients: Ceftazidime or Ciprofloxacin + Gentamicin
- For gram-positive source (burns, central and peripheral line): Cefazolin or Vancomycin (if indwelling catheter, intravenous drug user)
- For Anerobic source (peritonitis, biliary, female GUT, aspiration PNA): GEMA /C (Gentamicin + Metronidazole + Amoxicillin or Ceftriaxone)
- Circulation
Prognosis
| Number of organs affected | Survival |
|---|---|
| 1 organ | 70% survival |
| 2 organs | 50% survival |
| 4 organs | Almost 100% mortality |
Anaphylactic shock
Decreased BP due to release of inflammatory mediators resulting in widespread vasodilation
FEVER IS ABSENT, SKIN IS RED AND SWEATY
- Patient History
- Bee sting
- Consuming and allergen: shellfish, eggs, peanuts,
- Exposure to an allergen: dust or pollen
- Medication: Penicillin, NSAIDs, Aspirin, Sulpha drugs, Traditional herbs
- Infection: parasitaemia, EBV, HBV, Cocksackie virus
- Treatment
- Stop the precipitating factor
- Stop medication
- Remove stinger
- Gastric lavage and activated charcoal
- Airway
- Maintain patency.
- Prepare for intubation or surgical airway
- Breathing
- 100% Oxygen via NRB mask
- Circulation
- Push 2L crystalloids (Hartman’s)
- Medications
- Adrenaline
- Glucagon (if adrenaline failed or is contraindicated)
- Antihistamines (Diphenhydramine, Chlorpheniramine, Promethazine, Cimetidine)
- Salbutamol (for bronchospasms)
- Hydrocortisone
- Stop the precipitating factor
Neurogenic shock
Decreased BP due to loss of autonomic reflexes. This is different from spinal shock which is transient depression of cord function.
- Cause
- Spinal cord injury
- Patient History
- Trauma (probably high-energy)
- Signs and symptoms
- Hypotension
- Relative bradycardia
- Hypothermia
- Investigations
- Trauma series: C-spine XR, AXR, Pelvic XR
- CT or MRI if stable
- Treatment
- Manage airway and breathing
- Circulation
- Titrate fluids with urine output
- Consider vasopressors if BP does not respond
- IV high dose Methylprednisone (for non-penetrating spinal injury within 8 hours of injury)