Schizophrenia
Schizophrenia is characterized by two or more psychotic symptoms for 6 months or more. Symptoms can be delusions, hallucinations (mainly auditory), disorganized speech, disorganized or catatonic behaviour, and negative symptoms (affective flattening, avolition, mutism). They severely impact daily life (social and occupational) and lead to a downward drift (low SES). Diagnosis is clinical. It is unwise to stereotype people with schizophrenia as “homeless bums on the street”. It can happen to anyone, can come on at any age, and can be very difficult for patients and families to deal with. Schizophrenia is degenerative. Some days the patient may be symptom-free, but over time they are only getting worse
It affects 1% of the general population. Life-time risk if 40% higher in males (M:F ratio of 4:1). Peak onset in men is 15 – 24 years and about 5 – 10 years later in women. Women have a second peak at 55-64 years
14% achieve slow sustained recovery after treatment for 5 years. The rest show relapse (85% relapse rate, very difficult to treat)
6% of patients die by suicide with or without treatment. 20% attempt suicide (the suicide is usually bizarre, not planned for, and males are more likely – 20% higher incidence rate than the general population)
Historical perspective
| History | Description |
|---|---|
| Emil Kraeplin (1893, Germany) | Drew a distinction between manic depressive insanity & Dementia praecox to identify schizophrenia and isolate it. The term Dementia praecox to represent schizophrenia was popularized by him |
| Eugene Bleuler (Early 20th century Sweden) | Coined the term ‘schizophrenia’ which means ‘split mind’ in 1908 |
| Kurt Schneider (1959, Germany) | Desribed symptoms of the first-rank |

Etiology
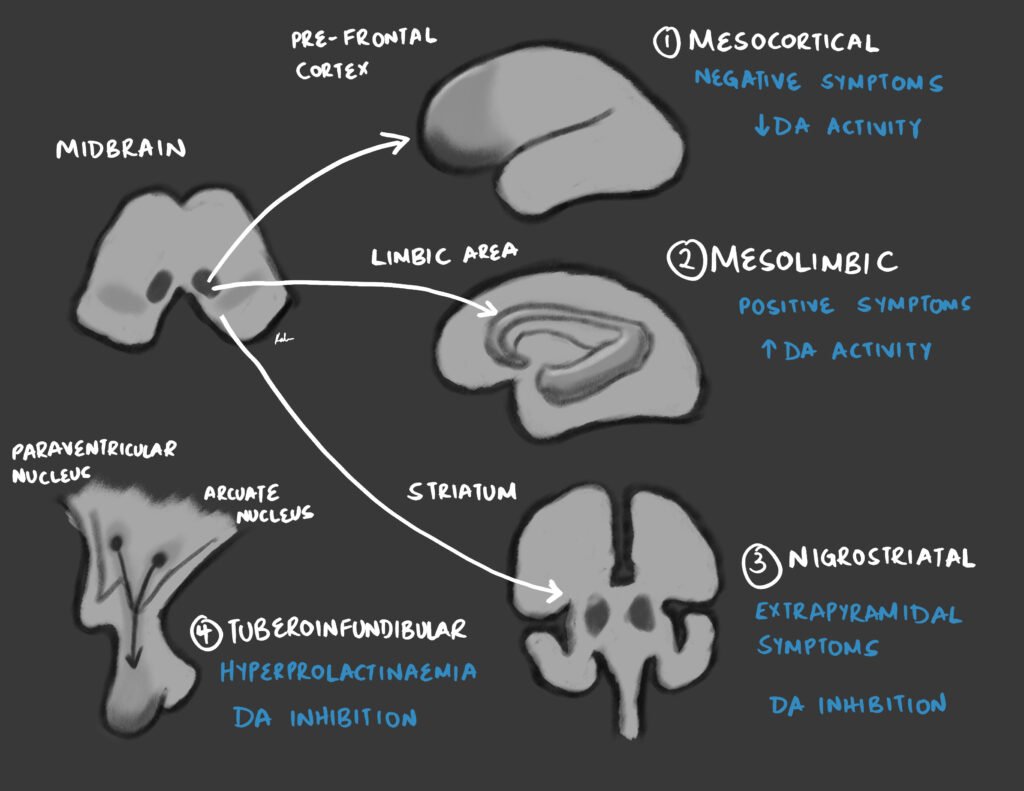
The theory goes that Dopaminergic activity increases so much in a patient with schizophrenia that it essentially “burns out” the basal ganglia. Hence the findings in neuroimaging and the need to inhibit dopamine as pharmacotherapy.
Schizophrenia has a very strong genetic linkage.
| Etiology | Description |
|---|---|
| Dopamine theory | There is increased amount of or activity of dopamine. The nigrostriatal pathway affects the limbic system (hippocampus, amygdala, thalamus and parts of the cortex) and Ventral striatum (nucleus accumbens). Blocking dopamine activity forms the basis for treatment. Dysfunction of glutamate, 5-HT, and GABA have alse been hypothesized. |
| Histological changes | Smaller and densely packed pyramidal cells (especially of the hippocampus and dorsolateral prefrontal cortex). This may be due to delayed neuronal migration. There are reduced synapses in the hippocampus and prefrontal cortex. There is no dysplasia or gliosis in the cortical regions. |
| Neuroimaging findings | Cortical atrophy (reduction of cortical volume especially around the basal ganglia), enlarged lateral ventricles, hypoactive frontal lobe (on PET), hyperactive basal ganglia (on PET). Which came first? Changes in the brain to cause schizophrenia OR schizophrenia to cause changes in the brain? |
| Genetics | 85% heritability (about similar to T1DM), 47% monozygotic concordance, 16% dizygotic concordance, 12% primary concordance (1st degree relative), 6% secondary concordance (2nd degree relative) and 1% lifetime risk (affects 1% of the population) |
| Epigenetics | Epigenetic changes occuring in response to environmental factors in genetically vulnerable or resilient individuals can be transferred to the next generation. Some that may play a role in schizophrenia include methylaiton affecting GABA and BDNF genes, and acetylation of Histone proteins. |
| Psychosocial factors | Childhood adversity (emotional abuse, physical abuse, sexual abuse, neglect, and death of one or both parents), migration (especially becoming a member of a lower SES in an affluent nation), being born in an urban area and any major stressful life events |
| Schizophrenogenic mother | Proposed by Frieda Fromm-Reichman, a psychoanalysis. His theory was that a mother could ‘cause’ Schizophrenia in her offspring though her attitude towards the child e.g. being dominant and overprotective but also rejecting and insensitive. This is no longer valid |
| Double-bind hypothesis | Proposed by Gregory Bateson, a British Anthropologist. A child being given mutually contradictory messages that puts him/her in a bind, resulting in schizophrenia. This is no longer valid. |
Phases of schizophrenia
The risk phase is crucial for prevention. The prodrome is crucial for early detection, especially in children.
At-Risk Mental State (ARMS): these are features which if present, put the person at an increased risk of developing future psychosis. They include a short-lived or mild symptoms of psychosis within the last 3 months, reduced functioning over the last 12 months (e.g. withdrawing from school) and brief limited intermittent psychotic symptoms (BLIPs) that spontneously stopped within 7 days. 1 in 3 individuals with ARMS develop psychosis.
| Phase | Description |
|---|---|
| Risk phase | Crucial for prevention. Involves genetic factors, intrauterine factors (viral infection), obstetric factors, and substance use (psychoactives – especially Cannabis) |
| Prodrome | Involves isolation (the patient simply withdraws), poor school performance, poor work output and odd thinking. This is a retrospective concept (compared to ARMS) i.e. it is obtained through history. |
| Psychiatric phase | Involves positive symptoms |
| Chronic phase (Disability) | Involves negative symptoms. It is essentially irreversible. |
Symptomatology
- Kurt Schneider’s Symptoms of the First Rank (these hallucinations and delusions strongly suggest the diagnosis of schizophrenia)
- Auditory hallucinations
- Audible thoughts (Thought echo): voices repeating the subject’s thoughts aloud (Echo de la pensee)
- 3rd person voices discussing or arguing about the patient
- 3rd person voices giving a running commentary on the patient’s actions
- Thought alienations or control
- Thought withdrawal: thoughts cease and the subject simultaneously experiences them as removed by an external force
- Thought insertion: Alien thought put into the subject’s mind
- Thought broadcasting: feeling that the subject’s thoughts are public e.g. through the radio or television
- Delusions of being controlled (Passivity phenomena)
- Somatic passivity: Influence playing on the body, the experience of bodily sensations imposed by an external agency
- Made feelings: feelings do not seem to be own, attributed to external force
- Made impulses: drive or impulse seem to be alien and external
- Made volitional acts: actions and impulses seem to be alien and external
- Delusional perception: normal perception has private and illogical meaning (experiences a normal sensory perception but assigns a false meaning to it). A two stage process where first a normal object is perceived then secondly there is a sudden intense delusional insight into the objects meaning for the patient
- Auditory hallucinations
- Positive symptoms (seen in the acute phase and respond well to antipsychotics)
- Hallucinations: these are remarkable and are mainly auditory. Can be in the form of 3rd person voices or second person voices.
- Delusions: usually bizzare. May have grandiose or persecutory themes
- Formal thought disorder: includes derailment, incoherence, and neologisms
- Disorganized speech
- Grossly Disordered or Catatonic Behavior
- Negative symptoms (seen in the chronic phase and tend not to respond well to medication)
- Flat affect: diminshed emotional expression with reduced expression of emotion in the face, speech, and bodily movement (patients may also have inappropriate affect)
- Anhedonia: reduced ability to experience pleasure, reduced interpersonal skills (the anhedonia of schizoprenia does not respond to antidepressant or other treatment, unlike that of depression)
- Asociality: apprent lack of interest in social ointeraction
- Avolition (apathy): reduced self-initiated purposeful activity
- Alogia: diminshed speech output (poverty of speech)
- Self-neglect
- Other signs and symptoms
- Cognitive dysfunction: 60-78% of patients have cognitive impairment. Can be detected with special testing before the first psychotic episode and persists throughout the course of the disorder (Dunedin Longitudinal Study). Dysfunction of working memory (executive functions) may be the core deficit.
- Impaired social cognition: difficulty inferring other people’s thoughts – thus unable to predict other’s reactions
- Catatonia: manifests as decreased motor activity, decreased engagement during interview, or excessive and peculiar motor activities
- Disorganized or chaotic behavior: classical ‘mad person’, goes hand in hand with self-neglect
- Negativism: the patient typically goes against what you say
Subtypes of Schizophrenia
Differentiation of these subtypes is not important since treatment remains the same. But be aware they exist. Disorganized schizophrenia has the worst prognosis.
| Subtype | Description |
|---|---|
| Paranoid type | Delusions, hallucinations and thought disorder are prominent. Delusional themes may be persecution, reference, jealousy, and grandiosity. Hallucinatory themes may be commenting/discussing, threatening/commanding, bodily sensations/movements. Thought disorder may manifest as incoherent/irrelevant speech or neologisms. |
| Disorganized (Hebephrenic) type | This is the most severe type. It is associated with disorganized speech and no association with reality. The patient may be highly unkempt, confused, child-like and difficult to maintain the interview. There may be inappropriate/incongruous affect and behavior is aimless rather than goal-directed. Delusions and hallucinations are either absent or are not prominent. |
| Catatonic type | This is the most dramatic presentation with prominent psychomotor symptoms. In catatonic stupor the patient is mute and mobile. Other catatonic signs include posturing, waxy flexibility, negativism, automatic obedience (command automatism) and excitement |
| Residual type | Positive symptoms are attenuated. Negative symptoms may only be present. There is also a marked decline in social functioning. |
| Undifferentiated type | Does not fit into any of the types above. None of the characteristics are prominent |
Management
It is important to do a proper risk assessment when diagnosing schizophrenia. Although not routinely needed in clinical practice, the Brief Psychiatry Rating scale (BPRS) or Positive and Negative Symptoms Scale (PANSS) can be used to monitor the progress of treatment. Regular medication should continue for at least 6 months after the first acute episode. Lifelong medication may be required to prevent relapse.
- Risk assessment
- Patients with acute schizophrenia, especially men, in the early course of illness are at an increased risk of suicide
- A very small proportion of patients pose a risk to others
- Some symptoms that may increase risk:
- Command hallucinations that order the patient to harm themselves or others
- Delusional beliefs of being controlled by someone else
- Other factors that increase risk to others
- History of violence
- Co-morbid alcohol or substance misuse
- Non-compliance with medication
- Antisocial personality traits
- Poor insight
- Investigations
- Baseline labs as indicated: CBC, LFTs, U/E/Cs, TFTs, Glucose, Lipids etc.c
- Urine toxicology screen if indicated
- Brain imaging (CT scan and MRI) if indicated
- EEG if indicated
- Baseline EKG since some atypical antipsychotics may prolong the QTc
- Pregnancy test for women
- Other tests: CDRL, BS for MPs, TFTs
- Treatment
- Hospitalization if symptoms are severe, there is poor insight, there is risk to self or others, or there is no reliable carer at home
- Antipsychotics**:** mainstay of treatment. Second generation antipsychotics are preferred.
- Cognitive Behavioral Therapy for treatment-resistant psychotic symptoms
- Electroconvulsive therapy in catatonic schizophrenia or augmentation of clozapine in treatment-resistnat schizophrenia
- Psychiatric social workers help the patient maximize function in the outside world
- Discharge to a rehabilitation centre or home
- Frequent outpatient review
- Other treatment options:
- Psychoeducation
- Family therapy/ family intervention
- Art therapy
- Adherence therapy
- Cognitive remediation therapy
- Social skills training
- Factors for good prognosis (25%)
- Female gender
- Older age of onset
- Significant mood component
- Family history of mood disorder
- Premorbid high IQ and robust, resourceful personality
- A significant mood component
- Nil or minimal cognitive impairment
- Compliance with treatment
- Sudden onset (stressor is identifiable and can be removed)
- Rapid response to treatment
- Treatment early in the course of the disorder (acute psychosis is ‘toxic’, causing progressive brain damage)
- Compliance with treatment
- Rejection of illegal substances
- Factors for poor prognosis
- Onset at an early age
- Insidious onset
- Long duration of untreated psychosis (DUP)
- Prominent negative symptoms
- Pre-morbid personality problems
- Co-morbid alcohol or drug abuse
- High expressed emotion in the family
- Prevention
- Genetics
- Personality change
High Expressed Emotions (HEE)
A mother or another close cares with whom the patient lives with can cause psychological harm by exhibiting High Expressed Emotions. HEE refers to high levels of emotional over-involvement, hostility and critical comments. The risk of relapse is high if the patient lives in a home environment with HEE. Families with HEE can be helped with family therapy and day hospitals where the patients spends the daytime away from home.
- Examples of HEE
- A mother who is very protective of her sone with schizophrenia and does not give him any independence
- A father who makes constnat negative comments about his son with schizophrenit e.t.c that he is an underachiever and idler
Treatment Resistant Schizphrenia (TRS)
Treatment resistance schizophrenia (TRS) is defined as failure to respond to at least two antipsychotic medications given at an adequate dose, with sufficient adherence and for a minimum duration of six weeks. Clozapine is indicated for the management of treatment resistant schizophrenia. Electroconvulsive therapy can also be used for clozapine-resistant schizophrenia.
- Investigations
- Complete Blood Count: Before initiation of clozapine, weekly for the first 6 months, biweekly for the next 6 months, then monthly for the remaining duration of treatment
- Fasting blood Glucose
- Lipid profile
- Liver Function tests
- Electrocardiogram
- Treatment
- Clozapine (maintenance of 300 – 600 mg per day): titrate dose gradually over 2 – 4 weeks to reduce the incidence of adverse effects
- Day 1: 12.5 mg
- Day 2-3: 25 mg
- Day 3-4: 50 mg
- Benzhexol or Trihexyphenidyl: if there are extrapyramidal side effects (drooling of saliva, rigidity, fine tremors or dystonia)
- Clozapine (maintenance of 300 – 600 mg per day): titrate dose gradually over 2 – 4 weeks to reduce the incidence of adverse effects
Schizophreniform disorder
Meets all the clinical criteria for schizophrenia BUT symptoms last less than 6 months (but greater than one month) Diagnose and manage just like schizophrenia with atypical antipsychotics. May need to be hospitalized acutely. Diagnosis shifts to schizophrenia if the patient has not recovered and still meets the criteria after 6 months. Not all patients progress to schizophrenia (about 50%)
Brief Psychotic Episode
Meets all the clinical criteria for schizophrenia BUT symptoms last for less than 1 month. Hospitalization if the patient is acutely psychotic. Atypical antipsychotics are the mainstay. Benzoz may be useful. Diagnosis shifts to schizophreniform disorder if the patient has not recovered and still meets criteria after 1 month.
- Adjustment disorder vs Brief Psychotic Episode
- Brief psychotic episodes last shorter (< than 1 month) and are accompanied by psychotic symptoms
Schizoaffective Disorder
The patient has symptoms of mood disorders (MDD, Manic episodes, mixed depressive/manic episodes) and symptoms of schizophrenia (delusions, hallucinations etc.). Better prognosis than schizophrenia. 50% of pts with schizophrenia have depression.
As per the DSM-V, schizophrenic (Psychotics) symptoms must be present for at least two weeks without mood symptoms (mood symptoms can clear but psychotic symptoms remain for 2 weeks). However, this definition is too rigid. Hence in practice the diagnosis is considered if the patient meets criteria A for schizophrenia and presents with a mood episode. 50% of patients with Schizophrenia have depression.
F>M. 30% of cases start 25-35y. 0.3% lifetime prevalence. 10-30% of inpatient admissions.
- Differentials
- Schizophrenia
- MDD with psychotic features
- Major Mood Disorde (BPD1 and BPD2)
- Treatment
- Atypical antipsychotics (first line, for psychotic symptoms)
- Mood stabilizers, SSRIs/Antidepressants (depending on mood symptomssymptoms)
- Cognitive Behavioral Therapy
- Electroconvulsive Therapy
- Family Therapy (depending on the case)
Delusional Disorder
Characterized by delusions for at least one month. Can have hallucinations**. NO IMPAIRMENT IN FUNCTION** (although people may think the patient is “crazy”). Remember to keep culture in mind. If the “delusion” is an accepted cultural view in that patient’s culture then it is not a delusion.
Can have hallucinations (not marked); undifferentiated; shared psychotic disorders
Further Reading
Reichenberg, A., Caspi, A., Harrington, H., Houts, R., Keefe, R. S. E., Murray, R. M., Poulton, R., & Moffitt, T. E. (2010). Static and dynamic cognitive deficits in childhood preceding adult schizophrenia: A 30-year study. American Journal of Psychiatry, 167(2), 160–169. https://doi.org/10.1176/appi.ajp.2009.09040574



