Overview
Retinopathy of prematurity is a disease of the retinal vasculature in pre-term and low birthweight infants. It is one of the leading causes of avoidable childhood visual impairment and blindness. The severity of retinopathy of prematurity varies. Screening is important since it can lead to complete retinal detachment and permanent visual deficits. All at-risk neonates should be screened via dilated fundoscopic exam by about 5 weeks of age.
Affects 50% of babies < 1250g at birth. 10% will go on to develop more severe diseases that will require surgery.
- Risk factors
- Prematurity (the more premature the higher the risk, esp. <32 weeks gestation)
- Low birth weight (especially <1500g)
- Supplemental oxygen
- Hypoxemia
- Hypercarbia
- Concurrent illnesses
- Male sex
- IUGR
- Pathogenesis
- Normal vascularization of the retina begins at 16 weeks of gestation, proceeds anteriorly towards the ora serrata, and is completed by 36-40 weeks gestation.
- Preterm infants are bone before retinal vessels are fully formed. There is an anterior avascular zone.
- The retina experiences hyperoxia due to exposure to ambient or supplemental oxygen. This causes vasoconstriction, cessation fo vascular growth and retinal hypoxia .
- Abnormal vascular development at the junction of the vascular and avascular retina forms a visible ridge.
- There is subsequent increased production of VEGF which triggers abnormal vascularization of the retina
- These new vessels are fragile and can easily bleed. Severe proliferation can cause traction on the retina causing detachment.
- Signs and symptoms
- Leukocoria
- Investigations
- Dilated fundoscopic exam: Screen all at-risk neonates by 5 weeks of age
- Treatment
- Stages 1 and 2
- Observe with regular exam q1-2 weeks (arrested at this stage and regresses spontaneously)
- Stage 3 and higher/ Zone I/ Plus disease/ Aggressive posterior ROP
- Laser ablation or Cryotherapy to arrest vascular proliferation
- Anti-VEGF (Bevacizumab, Ranibizumab)
- Long-term follow-up for 9-12 months to assess for other ocular abnormalities
- Stages 1 and 2
- What interventions are recommended to control ROP?
- Antenatal corticosteroids for preterm births < 35 weeks
- Delayed cord clamping by 30-60 seconds in preterm infants
- Pain Control
- Oxygen is used judiciously and saturation is maintained at 90-95% (remember that both hyperoxia and hypoxia are undesirable)
- Infection control
- Nutrition (exclusive breastfeeding)
- Temperature maintained at 36.5 – 37.2 C
- Supportive care (Kangaroo mother care, minimum blood transfusion, minimum noise, proper positiong in cots)
- What risk does ROP confer to infants
- Retinal detachment
- High-refractive error
- Anisometropia
- Amblyopia
- Strabismus
- Glaucoma
- Cataract
Classifying ROP
- How is ROP classified?
- By zone (anterior-posterior location. Zone I-III)
- By stage (Stage 1-5)
- By the extent (clock hours): number of 30-degree sectors or clock hours of retinopathy along the circumference of the vascularized retina
- Presence or abscence of plus disease
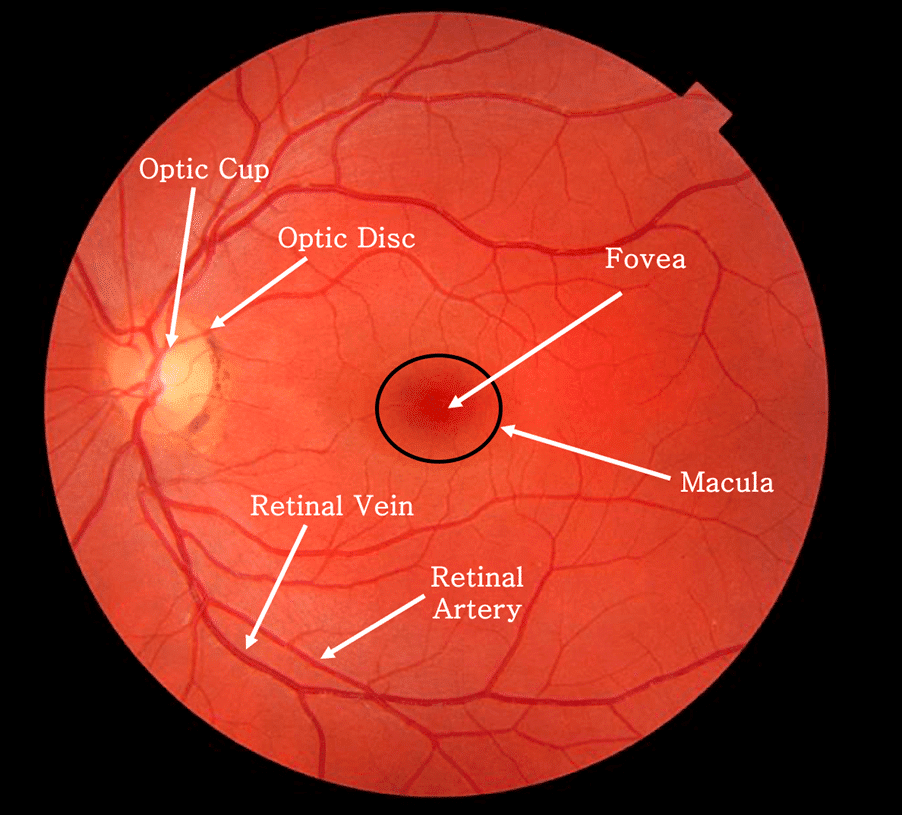
Zones of the Retina
Retinal zones are important when discussing Retinopathy of Prematurity.
| Zone | Description |
|---|---|
| Zone I | Twice the radius from the optic nerve to the fovea (macular involvement) |
| Zone II | Nasal Involvement to the temporal equator |
| Zone III | Residual crescent anterior to zone II |
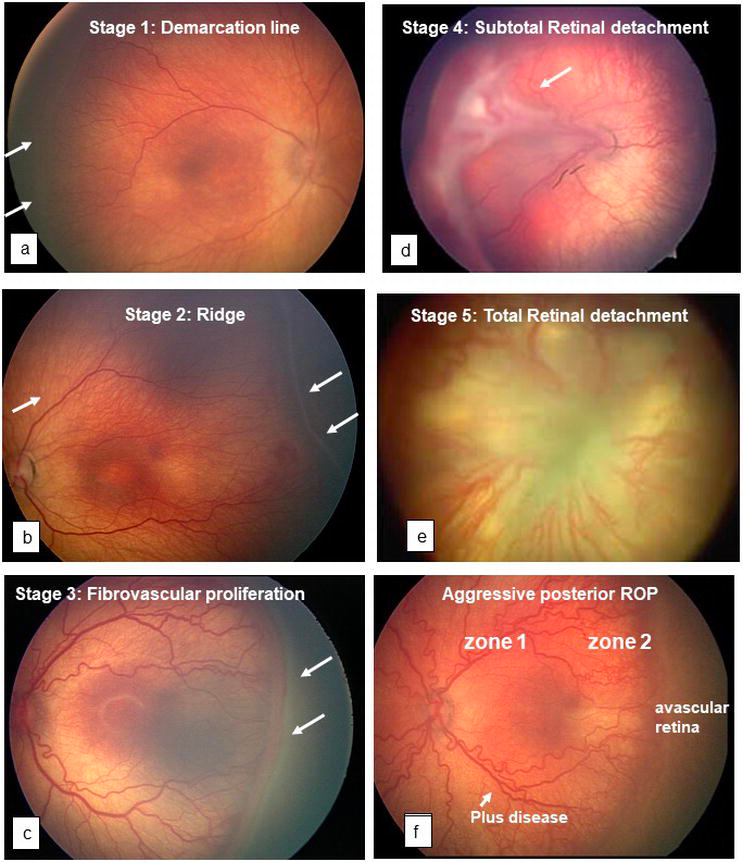
Stages of Retinopathy of Prematurity
| Stage | Description |
|---|---|
| Stage 1 | Demarcation line present between vascular posterior retina and avascular anterior retina |
| Stage 2 | Elevated “Ridge” present between avascular and vascular retina |
| Stage 3 | Fibrovascular proliferation around the ridge |
| Stage 4 | Partial retinal detachment |
| Stage 4a | Extrafoveal detachment |
| Stage 4b | Foveal detachment |
| Stage 5 | Total retinal detachment |
| Plus disease | Significant vascular dilation and/or tortuosity; Vitreous haze; Pupil restriction; Iris vascular engorgement |
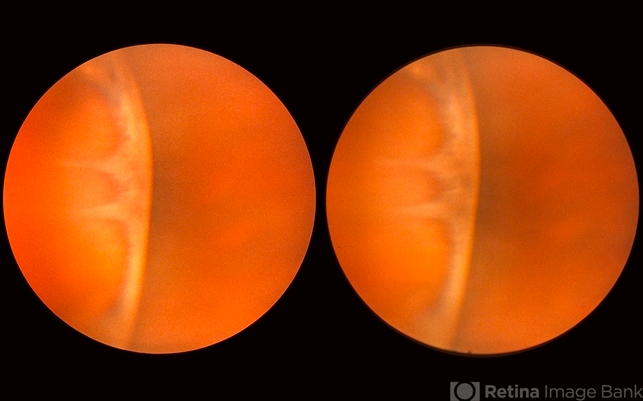
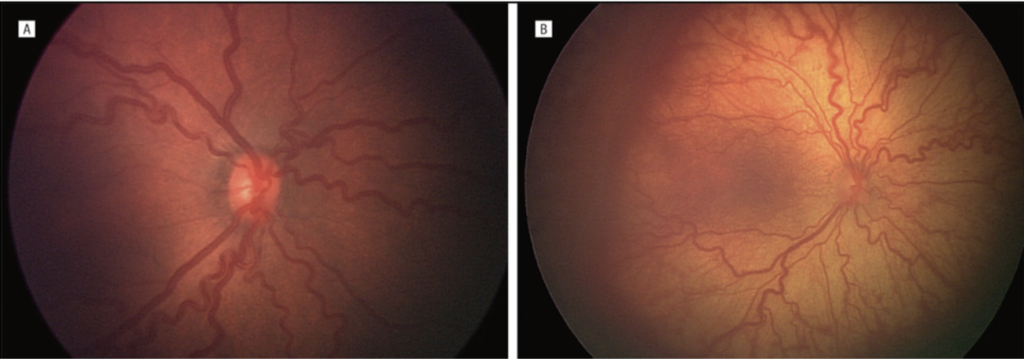
Plus Disease
- Significant vascular dilatation and/or tortuosity in two or more quadrants
- Vitreous haze
- Pupil restriction
- Iris vascular engorgement
Aggressive Posterior ROP
- Severe dilatation and tortuosity of posterior pole vessels
- May occur in zone I and zone II and is rapidly progressive
Screening ROP
- Who should be screened for Retinopathy of Prematurity?
- ALL babies born < 32 weeks of gestation
- ALL babies born weighing less than 1500g
- Babies born 32-35 weeks of gestation, weighing 1200-2000g with comorbidities (high/prolonged oxygen supplementation, Sepsis, NRDS, IVH etc.)
- Babies who have received high/prolonged supplemental oxygen exposure
- When should an infant be screened for Retinopathy of Prematurity?
- Within 3 weeks after delivery for neonates born < 30 weeks gestation
- Within 4-6 weeks after delivery for all other newborns
- When should follow-up screening be performed?
- q1-2 weeks
- What criteria should be met to allow the neonate to be released from screening?
- Complete retinal neovascularization up to zone III
- Post-menstrual age > 45 and the absence of pre-threshold disease
- ROP regression with non-reactivation certainty
- Which babies will need follow-up screening until 6-9 months of age?
- Surgical intervention
- General anaesthesia
- Sepsis
- Deterioration of clinical status
- On anti-VEGF treatment

Further Reading
- Mwangi, Nyawira & Onyango, Oscar & Gachago, Muchai & Murila, Florence & Njambi, Lucy & Gichangi, Michael & Nyamu, Gaceri & Mundia, Daniel & Bitok, Monicah & Sitati, Sarah. (2018). Kenya national guidelines for the screening and management of Retinopathy of Prematurity. 10.13140/RG.2.2.11928.44809.




