Presenting Complaints
- Cough
- Duration of cough?
- Character?
- Loud, brassy: pressure on the trachea
- Hollow, ‘bovine’: recurrent laryngeal palsy
- Barking: croup
- Chronic: pertussis, Tuberculosis, foreign body, asthma
- Dry, chronic: GERD, ACEi
- Timing?
- Nocturnal: asthma
- Exacerbating factors?
- Sputum? (colour and amount)
- Blood? (hemoptysis)
- Hemoptysis
- Contact with persons with chronic cough? Night sweats and fever? (Tuberculosis)
- Weight loss? (malignancy)
- Mixed with sputum?
- Not mixed with sputum? (pulmonary embolism, trauma, bleeding into lung cavity)
- Vomiting blood?
- Dark stools? (can occur if a significant amount of coughed up blood is swallowed)
- Dyspnoea Subjective sensations of shortness of breath, often exacerbated by exertion
- Duration?
- Steps climbed or distance walked before onset?
- NYHA classification?
- Diurnal variation? (asthma)
- Circumstance in which dyspnea occurs?
- Chest pain
- SOCRATES
- Worse on inspiration (pleuritic)
- Respiratory risks
- Pets at home
- Foreign travel
- Exposure to asbestos
- Exposure to persons with cough
- VTE risk factors
- Calf swelling
- Recent surgery or travel
- OCPs or recent clots in the legs
- Cancer complications
- Hoarseness (laryngeal palsy)
- Back pain (metastasis)
- flushing or diarrhea (carcinoids)
- Associated symptoms
- Hoarseness
- Wheeze
- Constitutional symptoms
- Fever
- Weight loss
- Fatigue
- Loss of appetite
- Night sweats
Physical Examination
Is the patient in obvious respiratory distress? Is there cyanosis? Is there wasting? Does the patient use pursed lips when breathing? Is the patient on oxygen/nebulizer/inhaler/drip? Does the patient have pallor/cyanosis?
General Inspection
Look for a bedside sputum pot
| Sputum characteristics | Cause |
|---|---|
| Yellow/green | Infection |
| Copious amounts | Bronchiectasis |
| Blood in sputum | Infection, Cancer, Pulmonary embolism |
| Black carbon specks | Smoking |
| Clear | Probably saliva |
| Pink frothy | Pulmonary oedema |
- Respiratory distress in adults
- Use of accessory muscles of breathing
- Breathing through pursed lips
- “Tripod” (Orthopneic) position
- Respiratory distress in paedatric patients
- Flaring of alae nasi
- Central cyanosis + mouth breathing
- Tracheal tug
- Use of accessory muscle (head nodding)
- Stridor
- Lower chest wall indrawing (subcostal recession(
- Xiphoid retraction
- Intercostal recessions
- Where do you check for cyanosis?
- Central cyanosis: base of the tongue
- Peripheral cyanosis:
- How would you expect the expiratory time to change in lung disease?
- Prolonged
- Are audible breath sounds normal in healthy individuals?
- No…
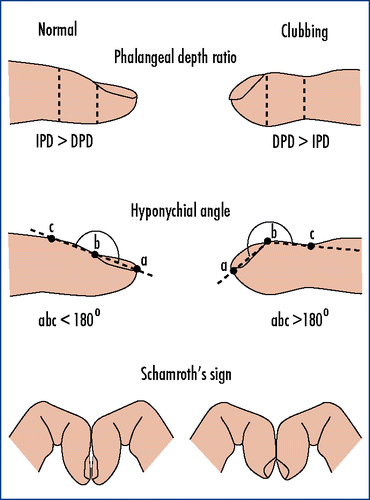
- Conditions associated with finger clubbing ***suppurative diseases
- Congenital cyanotic heart disease (95%)
- Pulmonary fibrosis (75%)
- Bronchiectasis (30%)
- Non-small cell lung cancer (25%)
- Empyema
- Abscesses
- Respiratory
- Suppurative disease: CF, empyema, bronchiectasis, non-small cell carcinoma, cryptogenic fibrosing alveolitis
- Rare: Lung abscess, mesothelioma, empyema, asbestosis
- Cardiac
- Common: Atrial myxoma
- Rare: Congenital cyanotic heart disease, infective endocarditis
- Gastrointestinal
- Common: IBD, Coeliac’s disease
- Rare: Cirrhosis
- Others
- Rare: Thyrotoxicosis, Familial, Pregnancy
Grading of finger clubbing
| Grade | Appearance |
|---|---|
| Grade I | Nail bed fluctuation |
| Grade 2 | Obliterated Lovibon |
| Grade 3 | Parrot beaking |
| Grade 4 | Hypertrophic Osteoarthropathy (HOA – looks like a drum stick) |
Inspection
Inspection of the hands
| Sign | Cause |
|---|---|
| Tar staining | |
| Dupuytren’s contracture | |
| Asterixis | |
| Coarse flap | CO2 retention |
| Fine tremor | Salbutamol (Beta 2 agonist) |
| Warm sweaty palms | CO2 retention |
| Koilonychia | Iron Deficiency Anaemia |
| Leukonychia | Hypoalbuminemia |
| Beau’s lines | Serious illness in the past 3 months |
| Splinter hemorrhages | Endocarditis, Trauma in manual labour |
Inspection of the face
Does the patient have cyanosis? Does the patient have conjunctival pallor? Does the patient have scleral jaundice?
| Sign | Cause |
|---|---|
| Horner’s sign | ***Drooped eyelids and anhydrosis – Ipsilateral Pancoast tumor |
| Corneal arcus | Old age, Wilson’s disease |
| Angular stomatitis | IDA, Pernicious anaemia |
| Glossitis | IDA, Pernicious anaemia |
| Acetone breath | Ketones |
| Dental state | |
| Thrush and leukoplakia | Immunosuppression, Linked with chest infections (Pulmonary tuberculosis, Pneumocystis pneumonia) |
| Freckles on the lips | Peutz-Jeghers Syndrome |
| Buccal pigmentation | Addison’s disease |
| Ochronosis | Alkaptonuria |
| General signs of swelling | SVC obstruction (thrombosis, lung carcinoma) – Loss of JVP, swollen head and neck, arms spared by collateral circulation, visible distended veins on the chest wall |
Inspection of the neck
| Sign | Cause |
|---|---|
| Hard lymphadenopathy | Malignancy |
| Soft, tender, rubbery lymphadenopathy | Tuberculosis, Mononucleosis, CMV, HIV, Local viral infection, Syphilis, Brucellosis, Local bacterial infection, Toxoplasmosis, Sarcoidosis |
Inspection of the Chest
- Respiratory rate: assess without the patient knowing as this can make them nervous
- Chest Shape
- Chest Size
- Chest Movement
- Scars and Masses
- Gynecomastia or Indentations of the breast
- Chest deformities
- Pectus excavatum: depressed sternum – Marfan syndrome; is cosmetic
- Pectus carinatum: Prominent sternum – Rickets; is cosmetic
- Kyphoscoliosis: idiopathic; quite severe and causes breathlessness in middle age
- Thoracoplasty: past treatment for TB where ribs were removed; reduced lung capacity and can cause breathlessness in old smokers
Palpation
- Chest expansion: Upper then lower chest, remember to check front then back, hands should go under the breasts
- Tactile fremitus: loudspeaker effect on consolidation
- Increased tactile fremitus: consolidation
- Decreased tactile fremitus: empyema, pneumothorax, pleural effusion
- Precordium: not useful in the respiratory exam but just palpate
- Crepitus: accompanied by tenderness in rib fractures, and may coexist with pneumothorax or hemothorax. Rarely pathological fractures from cancer
- Generalized swelling of the head and neck with crackling sensation under palpation: Subcutaneous emphysema
- Apex beat
- Right shift: Right lung collapse, Tension pneumothorax or large pleural effusion
- Left shift: Left lung collapse, Tension pneumothorax or large pleural effusion
- Axillary nodes: drain breast and pleura. >1cm is pathlogical
- Hard lump: breast Ca, rarely mesothelioma
- Firm lump: applies to other lymph node pathologies as well
Percussion
| Sign | Cause |
|---|---|
| Hyperresonant | Pneumothorax, Hyperinflation in COPD |
| Normal resonance | Normal chest |
| Dull | Consolidation, Collapse, Fibrosis |
| Stony dull | Pleural effusion |
Auscultation
Breath sound
| Sign | Cause |
|---|---|
| Vesicular breath sound | Rustling quality. Normal |
| Diminished (Quieter than normal) breath sounds | COPD and asthma, mild fibrosis, consolidation, collapse, pneumothorax, pleural effusion, obesity |
| Bronchovesicular | Bronchial breath sounds heard at the apices |
| Silent chest | Status asthmaticus |
| Bronchial breath sounds | Harsh breath sounds with a gap between inspiration and expiration. Consolidation, Fibrosis, Collapse |
| Wheeze | Due to air expired through narrow airways |
| Monophonic Wheeze (Rhonchi) | Tumor occluding airway, unilateral foreign body |
| Polyphonic Wheeze (Rhonchi) | Asthma, COPD, Cardiac asthma |
| Crackles (Crepitations) | Due to reopening of small airways on inspiration |
| Fine crackles | Pulmonary oedema |
| Coarse crackles | Bronchiectasis |
| Early inspiratory crackles | Small airway disease |
| Crackles that disappear after coughing | Insignificant |
| Pleural friction rub | Pneumonia, Pulmonary infarct, malignancy |
Vesicular vs Bronchial Breath Sounds
| Vesicular | Bronchial | |
|---|---|---|
| Quality | Quiet; Rustling | Harsh, Blowing |
| Origin of inspiratory sound | Alveoli | Bronchi |
| Origin of expiratory sound | Alveoli | Bronchi |
| Louder component | Inspiratory | Expiratory |
| Longer component | Inspiratory | Expiratory |
| Gap | Between expiration and inspiration | Between inspiration and expiration |