Changes from DSM-IV to DSM-V
- Sleep disorders related to another mental disorder/medical condition have been removed from DSM-V (e.g. insomnia d/t depression, Which makes the diagnosis of sleep disorder more specific)
- Primary insomnia has been renamed insomnia disorder (avoids the differentiation between primary insomnia and secondary insomnia, which is technically not a sleep disorder according to the DSM-V)
- DSM V distinguishes narcolepsy from other forms of hypersomnolence (the basis of narcolepsy has been found)
- Breath-related sleep disorders
- Obstructive sleep apnea-hypopnea
- Central sleep apnea
- Sleep-related hypoventilation
- Circadian rhythm sleep-wake disorders
- Advanced sleep phase syndrome
- Irregular sleep-wake type
- Non-24 hour sleep-wake type (90% in completely blind patients)
- Jet-lag type has been removed
- REM sleep behaviour disorder and restless leg syndrome are recognized as independent clinical entities (primary diagnoses) rather than collapse under the sleep disorders NOS category
Organization of Sleep
Brain wave patterns
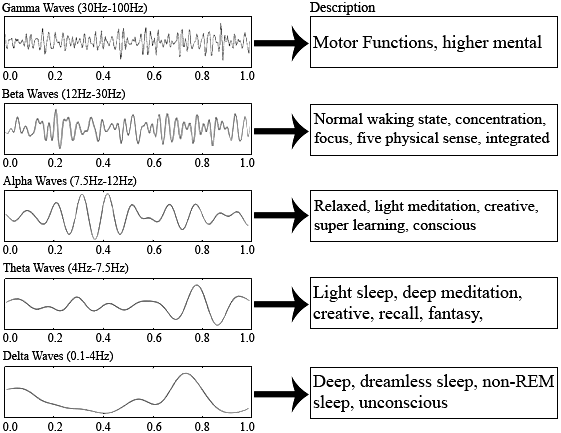
- Beta waves
- Awake
- Alpha waves
- awake-drowsy/sleepy/relaxed
- Theta waves
- light sleep (NREM 1)
- K waves and sleep spindles
- sleep NREM 2
- Delta waves
- Deep Sleep (NREM 3 and NREM 4)
Stages of Sleep
- Hypnogram
 Hypnogram
Hypnogram
- Time between REM episodes decreases
- Duration spent in REM increases
- Stage 4 sleep is the longest stage
- NREM sleep (75%)
- Body active (muscular tone), High muscular tone, Brain inactive (no conscious thoughts), No eye movement
- NREM 1: theta waves, 5%
- NREM 2: K waves and sleep spindles, 45%
- NREM 3: delta waves appear, 12%
- NREM 4: delta waves continue, 13%
- REM sleep (25%)
- Body inactive, Brain active (dreams), Rapid eye movement, No muscular tone
- Sawtooth waves
- Length of REM episodes increases through the night
- The frequency of REM increases through the night
- Delta sleep
- NREM 3 and NREM 4. Have delta waves
- Hardest to arouse
- Duration decreases with age
- REM latency
- Time measured between falling asleep and onset of REMThe averagege is 90 minutes
- Shortened in:
- Depression
- Narcolepsy
- Sleep latency time it takes to fall asleep average is 15 minutes
- Time it takes to fall asleep average is 15 minutes
- Lengthened in:
- Insomnia
- Shortened in:
- Narcolepsy
Neurochemicals involved in sleep
- Serotonin (Increased)
- Involved in sleep initiation
- Hence some SSRIs will make you drowsy
- Acetylcholine (increased)
- Involved in REM sleep
- Norepinephrine (decreased)
- Involved in REM sleep
- Dopamine (increased)
- Involved in **arousal and wakefulness (**but is increased during sleep)
- DA agonists (Parkinson’s agents – bromocriptine, pramipexole): produce arousal making it harder to sleep
- DA antagonists (Antipsychotics – haloperidol, risperidone etc.): reduce arousal making it easier to sleep (sedating)
- Alcohol and barbiturates (reduce REM sleep)
- REM rebound: increased REM sleep on acute withdrawal
Relationship between depression and sleep
- Reduced REM latency
- A greater percentage of sleep time is spent in REM
- Less percentage of time spent in Delta sleep (NREM 3-4)
- Multiple awakenings throughout the night
- Early awakening
Sleep Changes with age
- Less time spent sleeping overall (6-7 hours of sleep by 60s)
- Delta sleep (NREM 3-4) decreases until vanishing
- Time spent in REM decreases
- The majority of time sleeping will be in NREM 1-2
Insomnia (initiation)
Characterized by an inability or difficulty initiating sleep OR staying asleep, which affects the patient’s level of functioning or leads to daytime sleepiness. Very common and may be chronic/situational (test in the morning etc.)
- Symptomatic occurrence
- MDD
- Mania (has decreased need for sleep, will not have daytime sleepiness)
- Anxiety
- Comorbidities
- Anxiety disorders (GAD)
- Differentials
- Any psychiatric disorder that may cause insomnia: MDD, GAD, mania (will not have daytime sleepiness)
- Hyperthyroidism: will not complain of daytime sleepiness. Have symptoms such as tremors, weight loss, decreased appetite
- GERD: will have GERD sx
- Treatment
- Behavioural modification (Sleep hygiene)
- Benzodiazepine-like drugs (Zolpidem)
- Sleep hygiene
- Keep the room as dark as possible (no TV, close curtains)
- Environmental control (comfortable sleeping temperature, clothes or lack thereof etc.)
- Minimize distractions (keep work material etc. out of the bedroom)
- Do not work, read, watch TV etc. in bed (reserve bed for sleep & sex only)
- Avoid daytime naps
- Avoid eating 1-2 hours before sleep
Obstructive Sleep Apnea (all phases)
Characterized by cessation of airflow through respiratory passages during sleep (associated with snoring with long pauses). Diagnosed on a formal sleep study.
- Risk factors
- Obesity
- Male
- High “Mallampati” score
- Sx
- Daytime sleepiness
- Headaches in the morning (acidotic, low pO2)
- Dry mouth (use mouth to breathe)
- Dry nasal passages
- Sleeping partner complains of loud snoring or restlessness
- Treatment
- Home CPAP
- Weight loss (diet and exercise)
- ENT surgery (if indicated, class III and class IV mallampati)
Parasomnias
Sleepwalking
Self-explanatory. May perform mental activities (opening cupboards, opening windows, turning things on/off etc.) Occurs during NREM 3-4 (body active, muscle tone, no conscious activity): Common in men and starts at a young age
- Pt
- Can go back to bed OR Awaken during the walk and become confused
- Agitated when woken by someone else
- Treatment
- Ensure patient safety (alarms etc. as needed)
- Benzodiazepines (reduce length of NREM 3-4 hence reducing the frequency and duration of sleepwalking)
Night terrors
Primarily a paediatric disorder. Characterized by inconsolable, loud shrieking and general fearful demeanour (patient appears awake but is sleeping). Remits in minutes, pt immediately returns to sleep and has no memory of the event. Occurs during NREM 3-4.
- Treatment
- Rarely indicated
- Benzodiazepines (if frequent, taken before bed)
Nightmares
Unpleasant dreams. Occurs during REM and memory of the episode is usually intact.
- Comorbidities/Occurrence
- PTSD
- Depressive mood
- Anxiety disorders (esp. anticipatory anxiety)
- Treatment
- Generally not indicated
- Alpha-blocker (Prazosin; especially in PTSD)
- TCA (Imipramine)
Narcolepsy
Disorder of REM where the patient complains of excessive daytime sleepiness accompanied by sleep attacks and sudden loss of muscle tone (cataplexy). Hypnagogic and hypnopompic are common (these never qualify as psychotic; quite common in normal individuals too). Diagnosis is confirmed if the patient has had symptoms for ≥ 3 months
- Cataplexy
- Pathognomonic for narcolepsy
- Triggered by: intense emotions, loud sounds, flash of light
- Treatment
- Forced naps at regularly scheduled times(s) throughout the day.
- Stimulants (Modafinil) to increase wakefulness
- TCAs (imipramine) for cataplexy prophylaxis (suppresses REM)
