DSM-V Criteria
- Criteria for major neurocognitive disorder
- A. Evidence of significant cognitive decline from a previous level of performance in one or more cognitive domains (complex attention, executive function, learning and memory, language, perceptual-motor, or social cognition) based on:
- Concern of the individual, a knowledgeable informant, or the clinician that there has been a significant decline in cognitive function, AND
- A substantial impairment in cognitive performance, preferably documented by standardized neuropsychological testing or, in its absence, another quantified clinical assessment
- B. Cognitive deficits interfere with independence in everyday activities
- C. Cognitive deficits do not occur exclusively in the context of delirium
- D. Not better explained by another mental disorder or use of drugs(i.e., MDD, Schizophrenia, etc. Patients with other dementias will try to recall information while those with depression will be like IDK)
- A. Evidence of significant cognitive decline from a previous level of performance in one or more cognitive domains (complex attention, executive function, learning and memory, language, perceptual-motor, or social cognition) based on:
- Criteria for mild neurocognitive disorder
- A. Evidence of modest cognitive decline from a previous level of performance in one or more cognitive domains (complex attention, executive function, learning and memory, language, perceptual-motor, or social cognition) based on:
- Concern of the individual, a knowledgeable informant, or the clinician that there has been a mild decline in cognitive function, AND
- A modest impairment in cognitive performance, preferably documented by standardized neuropsychological testing or, in its absence, another quantified clinical assessment
- B. Cognitive deficits do not interfere with independence in everyday activities
- C. Cognitive deficits do not occur exclusively in the context of delirium
- D. Not better explained by another mental disorder or use of drugs(i.e., MDD, Schizophrenia, etc. Patients with other dementias will try to recall information while those with depression will be like IDK)
- A. Evidence of modest cognitive decline from a previous level of performance in one or more cognitive domains (complex attention, executive function, learning and memory, language, perceptual-motor, or social cognition) based on:
General Principles of Cognitive Disorders
Acute or insidious onset of disturbance in various cognitive and executive functions and/or in memory (amnesia).
Important to distinguish delirium from dementia first, then determine the cause
- Cognitive and executive functions
- Ability to speak
- Ability to execute motor skill
- Ability to recognize objects
- Ability to think abstractly and do daily activities in life
- Amnesia
- Loss of memory w/preservation of motor/executive functions
- Agnosia
- Failure to recognize familiar objects
- Aphasia
- Failure to produce or comprehend verbal speech
- Apraxia
- Failure to execute complex motor skills
- Disturbances in executive functioning
- Unable to think abstractly and having difficulty with activities of daily life
Types of Cognitive Disorders
- Classes of Cognitive disorders
- Delirium (acute and reversible)
- Dementia (chronic and irreversible usually)
- Amnesia
- Delirium
- As caused by General medical condition
- As caused by Substance intoxication
- Irreversible dementia
- Alzheimer’s type dementia
- Parkinson’s disease
- Vascular dementia
- Frontotemporal dementia (Pick’s)
- Huntington’s disease
- CJD
- AIDS Dementia Complex
- Wilson’s Disease
- Reversible Dementia
- Drugs
- Endocrine
- Metabolic
- Emotional (Pseudodementia)
- Nutritional
- Tumor or Trauma
- Infection
- Atherosclerosis
- Amnesia
- Wernicke-Korsakoff syndrome
Delirium
A disorder characterized by an acute confusional state. The patient is confused. Not a chronic state. Technically not a diagnosis but a syndrome (symptoms that coincide). Diagnosis is clinical. Circadian disruption is almost always present. Waxes and wanes. 10-30% of pts in general medical wards develop delirium. 44% of institutionalized elderly patients develop delirium.
- MMSE
- Disorientation (place/person/time)
- Memory impairment (recall of object)
- Reduced attention (serial 7s)
- Predisposing factors
- Age (older, >65y 1% can occur without precipitating factors, >85y 13%)
- Psychiatric comorbidities (mood disorders)
- Sensory impairment (blind, deaf)
- Nutritional problems (dehydration, malnutrition)
- Drug intoxication/dependence (keep an eye out on the surgery ward d/t anaesthesia)
- Most common causes
- Drugs (Anticholinergics, Opioids, Benzos, Anesthetics, Heroin)
- Dehydration
- Infection (especially CNS infections)
- Investigations
- CBC
- CMP
- Urine toxicology
- Differentials
- Dementia: chronic history, no acute medical problems
- Substance intoxication or withdrawal: cause of delirium. Notice and treat right away (urine tox screen and history)
- Delirium tremens: recent Hx of alcoholism, HTN and convulsions
- Management
- Correct underlying medical condition
- Haloperidol or atypical antipsychotic if agitated
Dementia
Chronic and progressive decline in cognitive function associated with actual CNS damage. Insidious onset (has been going on) and protracted. Personality changes are prominent
- MMSE
- Disoriented in time → place → person
- Investigation
- CBC
- CMP
- B12/Folate
- RPR
- TFT
- Differenitals
- Delirium: more acute onset, fluctuations, hallucinations more prominent
- Normal aging: occasional forgetfulness but it is not normal to lose orientation to person/place/time; no hallucinations)
- Pseudodementia: patients with depressive symptoms (less likely to fabricate answers questions, and more likely to talk about symptoms; pt with dementia fabricate answers and deny dementia
- Management
- Based on the underlying process (diagnosed by Hx and Labs)
Alzheimer’s Type Dementia
Chronic decline in MMSE score (slowly loses orientation to time → place → person). Dementia with no other symptoms (patient is otherwise healthy). The is often brought by fam. Diagnosis of exclusion
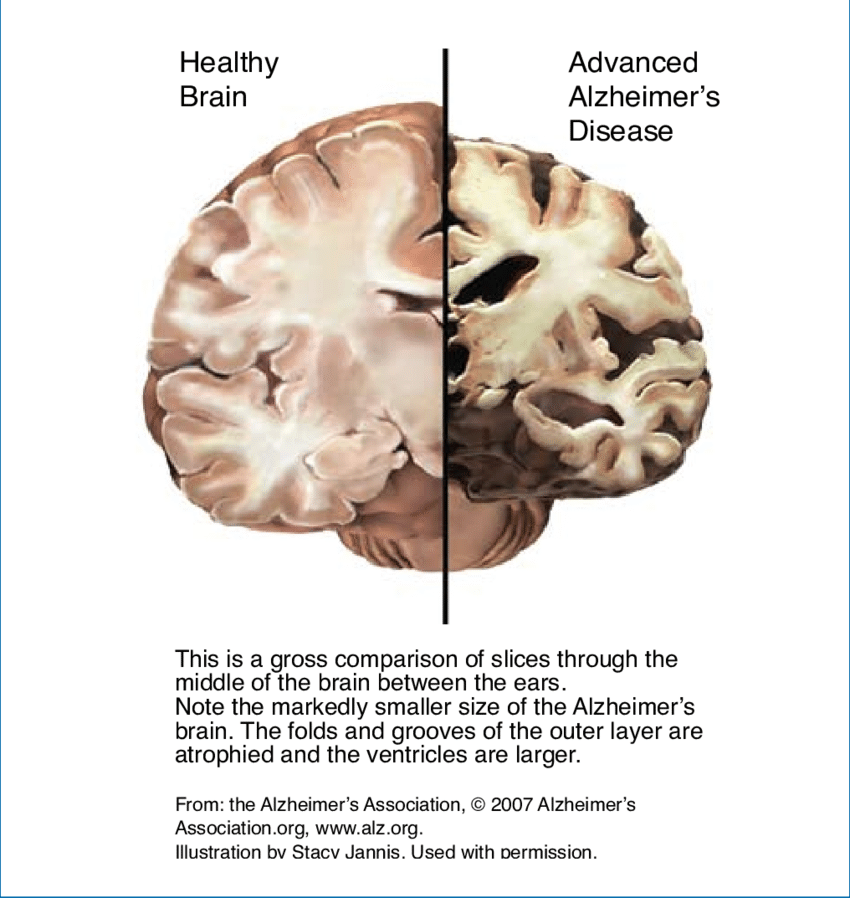
- Pathophysiology
- Cortical atrophy
- Reduction of ACh and NE synthesis
- Deposition of amyloid plaques
- Signs
- Unremarkable
- Focal defects = consider an alternate diagnosis
- Investigations
- CBC: Exclude infectious process
- CMP
- B12/Folate: alcoholism (
- TFT
- RPR: exclude neurosyphilis
- R/o depression
- Management
- Palliative, aimed at reducing symptoms
- AChE inhibitors (Donepezil, Galantamine, Rivastigmine, Tactine): Improves symptoms, does not shorten the course
- Antipsychotics (Risperidone, Haloperidol): if agitated
- Assisted living arrangements
Vascular Dementia
Dementia symptoms with FNDs in a non-linear course of progression (small, sub-clinical strokes happening at different times)
- Patient
- Hypertension
- Hypercholesterolemia
- Smoking
- DM
- FNDs that distinguish it from Alzheimer’s (demonstrated on neurological exam)
- Dysarthria
- Dysphagia
- Hemiparesis
- Focal weakness
- Ataxia
- Gait disturbances
- Hyperreflexia
- Pseudobulbar palsy (inappropriate display of emotion)
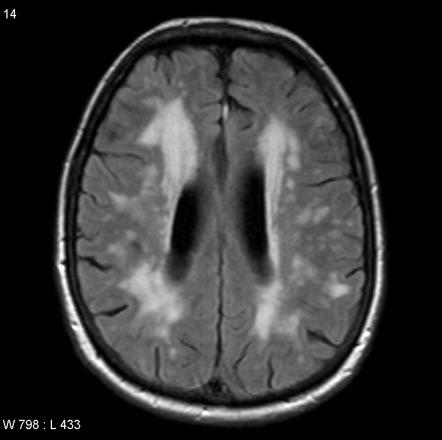
- Investigations
- CBC
- CMP
- B12/Folate
- TFT
- RPR
- CT/MRI: to look for focal infarcts
- Management
- Reduce risk factors for further infarcts
- Hypertension: ACEi or BB or Both
- Hypercholesterolemia: Diet and start a Statin
- Smoking cessation
- Diabetes management
Parkinson’s Disease/Lewy Body Dementia
Dementia in Patients with Parkinson’s disease. Can be mixed with Alzheimer’s dementia. No FNDs apart from those expected in Parkinson’s. Diagnosis is clinical (based on Hx of Parkinson’s disease). Labs are not necessary. Manage Parkinson’s disease
- Parkinson’s disease recap FNDs
- Resting tremor
- Pill-rolling tremor
- Bradykinesia
- Shuffling gait
- Masked facies
- Micrographia (small handwriting)
- Cogwheel rigidity
- Pathophysiology
- Idiopathic destruction of DA neurons at substantia nigra
- Dementia caused by Lewy bodies
- Management
- DA replacement (Carbidopa/Levodopa) – d/t destruction of dopaminergic neurons
- DA agonists (Benztropine, Pramipexole, Ropinirole) – pramipexole can lead to compulsive gambling. To increase activity of dopamine
- MAO-B inhibitors (Selegiline) – reduce the breakdown of dopamine
- Amantadine (antiviral, not first choice)
Pick’s Disease (Frontotemporal Dementia)
Difficult to distinguish from Alzheimer’s in a clinical situation (slow progression of cognitive decline). Has personality changes before memory impairment. Distinguished from Alzheimer’s at autopsy. Clinical diagnosis or diagnosis of exclusion
- Investigations
- CBC
- CMP
- B12/Folate
- TFT
- RPR
- Management
- Palliative. Alzheimer’s Meds are not effective
Huntington’s disease
Progressive dementia is accompanied by choreoathetosis and personality changes. Psychosis and suicidal thoughts are common. AD (parents are affected)
- Pathophysiology
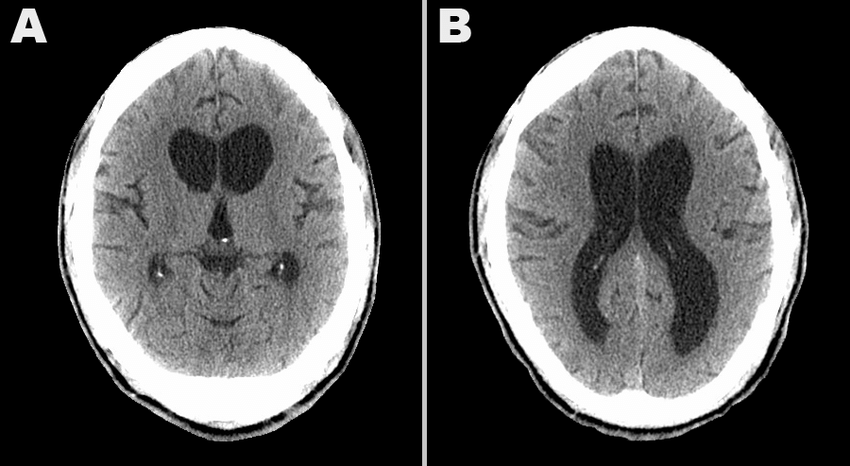
- Atrophy of the caudate nucleus (responsible for personality, learning, and movement along with the frontal lobe)
- Differential
- Schizophrenia: Earlier onset of illness, family Hx of schizophrenia, No family Hx of Huntington’s no choreoathetosis
- Investigations
- Genetic study
- CT head: mildly enlarged ventricles d/t caudate atrophy
- Management
- Palliative with emphasis on treating depressive and psychotic symptoms (SSRIs and Antipsychotics)
Creutzfeldt-Jakob Disease
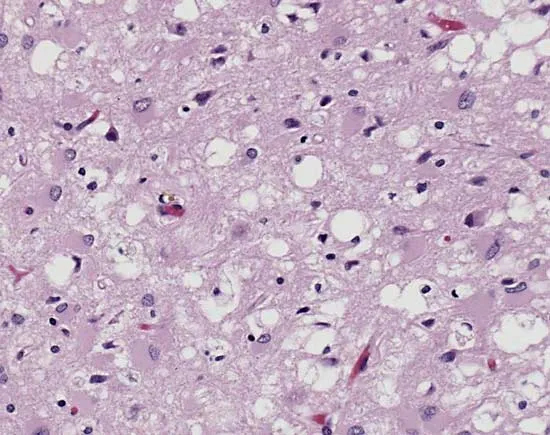
Rapidly progressive dementia that appears similar to Alzheimer’s and in some way to Huntington’s (chorea, gait disturbances). Progresses to death within months. Autopsy shows spongiform encephalopathy. EEG (if u suspect CJD) shows “sharp, triphasic synchronous discharge”. Management is palliative.
AIDS Dementia complex
Dementia and FDs in a patient confirmed with HIV infection. Mood/personality changes precede dementia. Consider in any patient with HIV who presents with psychotic symptoms. Pick’s dz + vascular dementia in an HIV-positive patient.
- Common FNDs
- Hypertonia
- Hyperreflexia (UMN damage)
- Snout reflex (frontal release)
- Management
- Adherence to HAART
Wilson’s disease
Very uncommon. Executive dementia is accompanied by psychotic disturbances, movement disorder disorder and prominent liver function. AR disorder of copper metabolism. Dementia might not be the presenting symptoms
- Presenting symptoms
- Psychosis
- Fatigue
- Executive dementia
- Inability to function in daily life (keep lists, hold job)
- Signs and symptoms
- RUQ pain
- Kayser-Fleischer rings
- Investigations
- LFTs: elevated
- Urinary copper: elevated
- Differential
- Schizophrenia: normal LFTs, normal urinary copper
- Management
- Chelate copper
- IV penicillamine
- Low copper diet (avoid nuts, shellfish, mushrooms, dried fruit)
- Chelate copper
Pseudodementia
This is not dementia. Symptoms of dementia (amnesia usually co-exist with MDD. Exclude when an elderly patient presents with symptoms of dementia. Patients with pseudodementia will bring themselves in and state the approximate onset of symptoms and elaborate on deficits
- MMSE
- PT says, “I don’t know” when testing memory (a patient with true dementia will confabulate)
- Management
- SSRIs and Psychotherapy
Amnestic Disorders
Wernicke-Korsakoff Syndrome
An amnestic disorder characterized by B1 deficiency. Wobbly Wernicke’s, Krazy Korsakoff’s. Classically seen in alcoholics.
- Wernicke’s encephalopathy
- Ataxia
- Nystagmus
- Ophthalmoplegia
- Confusion
- Sx of dementia
- Korsakoff’s psychosis
- Sx of dementia
- Psychosis
- Confabulation
- Memory loss is short-term
- Investigations
- B1 level: low
- Management
- IV thiamine replecement
- Supplement IV dextrose with thiamine in any patient with known or suspected Hx of alcoholism
