Overview
The nursery exam is done in the nursery or NICU within 24 hours of birth to identify any abnormalities or anomalies that may impact the infant’s current or future well-being. Some anomalies may not be visible grossly so blood screening tests are performed as well. The APGAR score done during deliver is not a comprehensive physical exam (ensures stability of the baby). 20% of babies will have one or more anomalies. Presence of one or two isolated anomalies is not unusual. Sequences or constellations of anomalies are associated with various congenital illnesses.
Babies do not have good temperature regulation. Make sure to rub the palms of your hand together quickly to create friction and warmth
Babies do not like having their face, eyes and ears touched. Be kind. Save this part for last so you don’t have a crying baby while auscultating.
Clean your hands and disinfect stethoscope before examining the baby
General exam
Introduce yourself, explain, get consent, and sanitize. Start the exam with general observation.
- Modified Paediatric GCS/ AVPU
- How is the baby lying in bed (attitude)
- Look for gross anomalies without touching
- Skin colour
- Breathing quality
- Anthropometric measurements
Modified Paediatric GCS
Eye opening
| Spontaneous | 4 |
|---|---|
| To speech | 3 |
| To pain only | 2 |
| No response | 1 |
Best verbal response
| Coos and babbles | 5 |
|---|---|
| Irritable cries | 4 |
| Cries to pain | 3 |
| Moans to pain | 2 |
| No response | 1 |
Best motor response
| Moves spontaneosly and purposefuly | 6 |
|---|---|
| Withdraws to touch | 5 |
| Withdraws to response in pain | 4 |
| Abnormal flexion to pain | 3 |
| Abnormal extension to pain | 2 |
| No response | 1 |
Vitals
| Heart rate | 120-160 bpm |
|---|---|
| Respirations | 30-60 rpm |
| Blood pressure | 50-70 mmHg systolic |
| Temperature | 36.1 – 37.9 C |
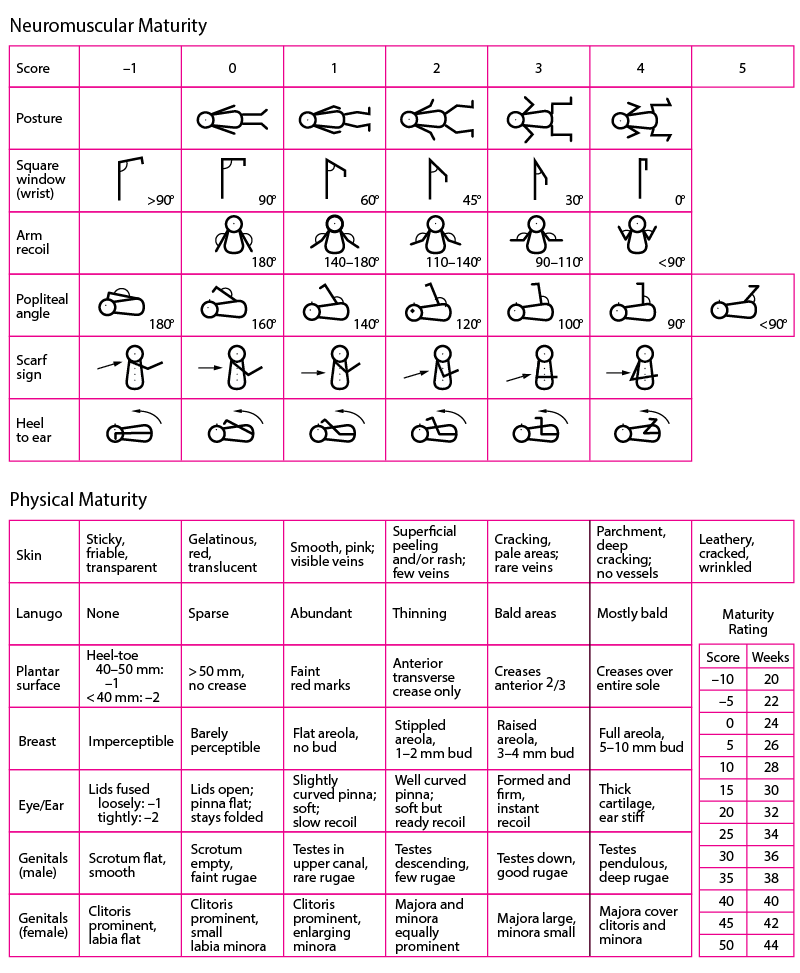
Simplified comparison based on typical Ballard’s Score results for preterm and term neonates:
| Characteristic | Preterm Neonate (Premature) | Term Neonate |
|---|---|---|
| Skin Texture | Usually smoother and less mature skin | Skin is typically well-textured |
| Lanugo | Abundant lanugo (fine hair) often present | Lanugo may be sparse or absent |
| Plantar Surface | Fewer creases on the sole of the foot | More defined creases on the sole |
| Breast Development | Less developed breasts (both genders) | More developed breasts (if female) |
| Eyes and Ear | Eyelids may be less fused, soft ears | Eyelids are well-fused, firm ears |
| Genitalia Development | Male genitalia may be less developed, female genitalia less mature | Male and female genitalia typically fully developed |
| Physical Maturity | Less subcutaneous fat, less muscle tone | Typically good subcutaneous fat and muscle tone |
Skin
Normally pink (baby may have blue or purple extremities immediately after delivery
- Jaundice
- Abnormal in the first 24 hours
- Haemolytic process
- Rh isoimmunization
- Congenital Hepatitis
- Get a CBC and LFTs
- Pallor
- Suggests acute or chronic blood loss
- Acidosis
- Cyanosis
- Poor cardiac output (warrants immediate investigation)
- Cold baby (usually put in warm environment)
- Plethora
- Polycythemia
- Texture
- Cracking or peeling is typical of post-term infants
- Edema
- Is it generalized or localized?
- Bruising or petechiae
- Birth trauma
- Bleeding disorder
- Cutis marmorata
- Lacing of mottling of the skin because babies have poor temperature regulation. “Capillaries seen through the skin”. Temporary (will go away)
- Vernix caseosa
- Curdy, greasy (”cheesy”) white stuff on term babies at delivery. Totally normal
- Erythema toxicum
- Migratory pink, maculopapular rash seen after the first 24 hours. It’s the immune system asserting itself. Normal and goes away after a few weeks
- Staphylococcal scalded skin syndrome (SSSS)
- Diffuse red rash, burn-like w/denuded skin + Nikolsky sign
- Needs broad-spectrum ABX and fluids stat
- Subcutaneous fat necrosis
- Idiopathic or d/t birth trauma. Erythematous, indurated, circumscribed nodules
- Does not require treatment. But check Calcium periodically.
- Capillary hemangioma
- Does not usually present within the first 24 hours. Red spots (papular) on the head or face. Grow like a mole but involutes later
- Port wine stain
- Flat red birthmark.
- Sturge-Weber syndrome (unilateral facial port wine stains)
- Mongolian spots
- Blackish blue spots on the buttocks. Clearly demarcated (unlike a bruises)
- “Melanocytes on steroids”
- Cafe-au-lait spots
- Light brown spots
- ≤ 3 is normal in white infant
- ≤ 5 is normal in a black infant
- ≥ 6 = various disease (NF-1, Tuberous sclerosis)


Head
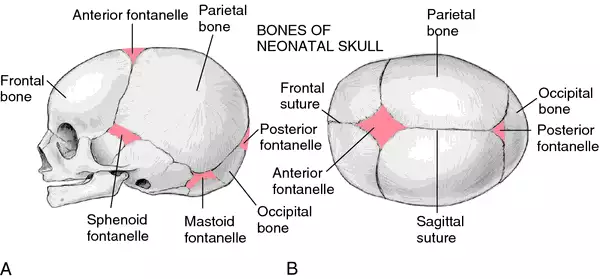
Put your hand behing the occiput. Look for scalp abnormalities. Gently palpate fontanelles. 6 fontanelles
| Anterior fontanele | 1-4 cm |
|---|---|
| Posterior fontanelle | < 1cm |
Scalp layers
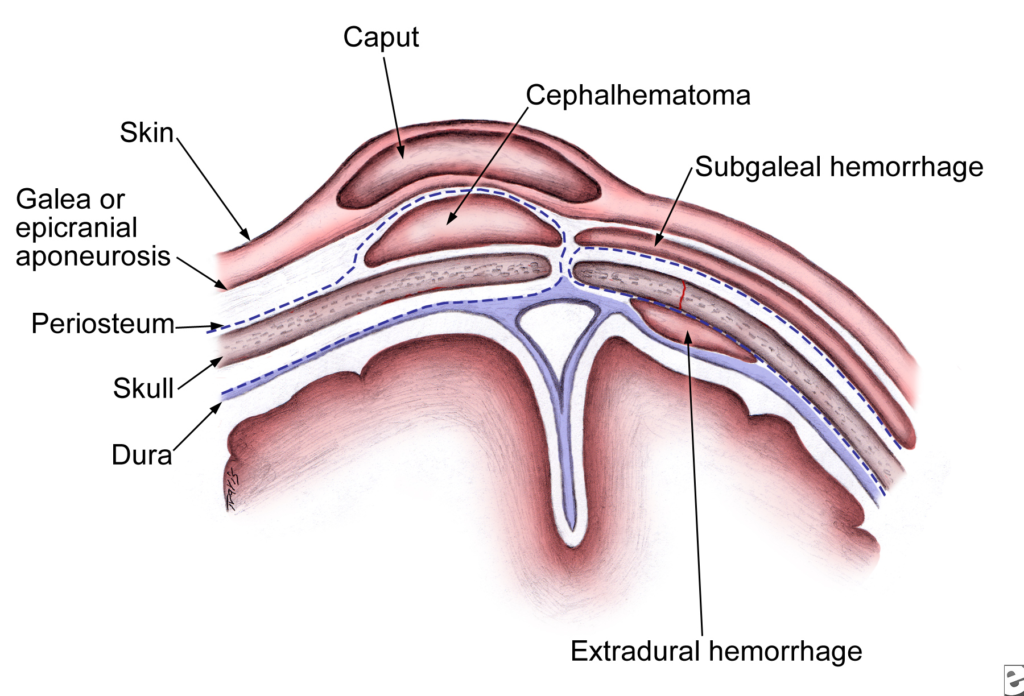
- Cephalohematoma
- Swelling of the head limited by suture lines. Blood collects between skull bone and periosteum. Observe.
- May follow with Jaundice.
- May have underlying linear skull fracture (treated conservatively)
- NEVER aspirate the blood
- Caput succedaneum
- “Cone head” swelling ot the head that crossess suture lines as it is superficial to the periosteum (between the scalp and subgaleal aponeurosis)
- Common in babies delivered SVD (d/t pressure)
- Resolves within a few days
- Subgaleal hemorrhage
- Potentially massive bleed noted as a fluctuant, boggy mass w/supericial skin bruising. May obscure suture lines (superficial to the periosteum)
- Associated w/vaccum-assisted deliver (90% of babies)
- Monitor for hypotension/tachycardia (scalp can hold a lot of blood. Baby may bleed out – perfuse with fluids and blood products if develops)
- Meningocele
- Located in the midline; occipital
- Associated with underlying bony defects
- Third fontanelle (along the sagittal suture)
- Associated with various congenital syndromes esp. Down syndrome
- Bulging fontanelle
- Elevated ICP (Meningitis, Encephalitis)
Eyes
Babies are born with 20/400 vision (legally blind, can conveniently see from mother’s breast to face). Rapidly improves. Should be able to track horizontally within about 9 inches.
- Subconjunctival haemorrhage
- Common (due to stress of birth. Mother may also have them)
- Coloboma
- “Latch-key” defect of the iris associated with CHARGE syndrome
- Aniridia
- Severe hypoplasia or absence of the iris. Has visiual implications. Associateed with WAGR syndrome.
- Hyphaema or cloudy cornea
- Opthalmology consult
- Leukocoria (white reflex) ***When checking red reflex. Needs immediate attention.
- Retinoblastoma
- Cataract
- Glaucoma
- Secretions
- Conjunctivitis – check mum’s TORCH titres for congenital inectious diseases
Ears
Malformed or malpositioned ears are associated with various congenital anomaies.
- Microtia
- Severely malformed ear
- Get CT to see if inner ear is developed
- Preauricular pits and tags
- Familal, patient is usualy normal
- May be associated w/GU defects or hearing abnormalities
- Tags may be associated w/cleft palate
Nose
Examine the shape of the nose
- Abnormally flattened nose
- d/t Intrauterine compression
- Flaring of nasal alae
- Respiratory distress
Examine the patency of the nares (important becuase babies are obligate nose breathers). Can do this by looking for steam collection on a chilled reflex hammer placed under the baby’s nose. Can also shine a light or try to insert a nasogastric tube.
- Choanal atresia
- Obstructed nose
- “A” in CHARGE syndrome
- Sx: Baby becomes cyanotic during feeding (will cry, breathe trhough mouth then become pink again
- Nasal secretions
- Congenital syphillis (careful coz secretions are full of syphillis…)
Mouth/Throat
Examine the mouth using a gloved index finger. Examine the sucking and rooting reflexes.
- Flat philthrum and thin lips
- Fetal alcohol syndrome
- Natal teeth
- May be present can be removed (risk of aspiration
- Epstein pearls (epithelial retention cysts)
- Along the gum margins. Resolves in a month.
Examine the tongue
- Macroglossia
- True macroglossia: Beckwith-Wiedman syndrome, Congenital hypothyroidism, Micropolysaccharidosis
- Apparent macroglossia: Down syndrome (d/t small mouth)
- Ankyloglossia
- An unusually short frenulum that reduces mobility of the tongue
Examine the palate. Examine the mandible (if chin is small, mandible is small).
- Cleft palate.
- Micrognathia (small mandible)
- Multiple syndromes eg. Pierre-Robin sequence
- Subglottic hemangioma
- May block airway
Neck
Look for webbing and masses. Important to find massess ASAP as they can get infected.
- Webbing
- Excessive nuchal skin
- Turner’s syndome
- Midline neck mass
- Thyroglossal duct cyst (moves with swallowing or tongue protrusion)
- Neck mass anterior to SCM (lateral to midline)
- Branchial cleft cyst
- Neck mass posterior to SCM
- Cystic hygroma
- Congenital torticollis
- Problem with SCM itself. Might feel resistance when turning the baby’s head to the opposite direction. Needs physical therapy.
Chest/Lungs
- Bones
- Fractures (esp of the clavicle) particularly in babies born during traumatic or surgical deliveries
- Air entry
- Should be bilateral
- If not, get CXR for possible pneumothorax
- Breath sounds
- Periodic breathing
- Grunting
- Added sounds: stridor, wheeze
- Absent on the left: pneumothorax OR congenital diaphragmatic hernia (get CXR, point of maximal impulse displaced to the right in case of hernia)
- Elevated Rr (>60 RPM) or Adventitious breath sounds: respiratory distress (get CXR)
- Decreased breath sounds: hyaline membrane disease
- Breast hypertrophy
- Normal. As a response to circulating maternal hormones
- Some milk may even be produced
- Supernumerary nipples
- Looks like moles
- Can be removed later on
- Pectus carinatum
- Bulging sternum
- Pectus excavatum
- Indented sternum
- Can compress the mediastinum if severe enough
Heart
Heart rate should be 120-160 bpm. Palpate pulses on all 4 extremities
- Murmurs
- Normal in first few hours after birth
- Murmurs + cyanosis: consider CHD (get echo)
- Muffled heart sounds: Pneumomediastinum
- Point of maximal impulse
- Displaced PMI to the right: CDH,
- Displaced PMI to the left: cardiac enlargment
Abdomen
Assess it’s shape. Inspect and auscultate first before palpating or percussing the abdomen.
- Scaphoid abdomen
- Congenital diaphragmatic hernia
- Distended abdomen
- Excess gas
- Mass
- Peritoneal fluid
- Umbilical stump
- Should not be bleeding or infected
- Bowel sounds
- Herniations
- Umbilical hernia
- Omphalocele: midline defect with contents covered w/membrane. Beckwith-Wiedman syndme
- Gastroschisis: defect lateral to midline contents w/o membrane covering. Usually Dx in-utero. Increased risk of malrotation and ischemia
- #1 true abdominal mass in neonates
- Polycystic kidney
- Palpate the liver and abdominal mass
Genitals/anus
Check for patency of the anus, position of the urethral orifice, descension of the testicles
- Imperforate anus
- Associated w/VACTREL complex
- Hypospadias
- Urethral orifice displaced ventrally
- Epispadias
- Urethral orifice displaced dorsally
- Undescended testes
- Clitoral enlargement
- Temporary.
- Was a response to maternal hormones
- Enlarged bladder (Confirm with U/S)
- Posterior urehral valves
Extremities
Are there ten fingers and 10 toes? Check for Developmental dysplasia of the hip, spinal alignment, webbing, fusion and polydactyly of the hands and fingers, and feet and toes. Ensure there are no absent bones (radius)
- Positive Ortolani and Barlow manoeuvers
- “Click” or “thump” = DDH
- Webbing
- 2 bones but skin fused together
- Fusion (syndactyly)
- Bones fused together
- Congenital absence of the radius
- Congenital absence of the fibula
- Club foot
Back
Neurological
Test the newborn reflexes
- Moro (”startle”) reflex
- Hold baby supine over the bed while supporting the head. Allow the head to drop an inch. Baby should abuct arm at shoulder and extend at elbow, spread fingers
- Disappears at 3 months
- Abnormal: Erb’s palsy
- Palmar grasp reflex
- Baby grasps finger in palm
- Disappears at 4 months
- Abnormal: Klumpke’s palsy
- Sucking reflex
- Baby will suck gloved finger/nipple when placed in mouth.
- Rooting reflex
- Baby turns head towards side cheek is touched
- Tonic neck reflex
- Baby assumes “fencin position” on opposite side when neck is passively turned on one side
- Babinski reflex
- Upgoing (extensor) plantar
- Normal in babies
- Abnormal past 1/2 years of age.
