Table Of Contents
HIE is basically caused by perfusion-reperfusion injury. It is a major cause of morbidity in preterm infants and is the MCC of neonatal seizures. In severe cases, ischemic injury can extend beyond the brain to involve the heart, liver, etc. Diagnosis is clinical. Look out for multiorgan dysfunction – Hepatic (80-85%), pulmonary (71-86%), cardiac (43-78%), hematologic (32-54%)
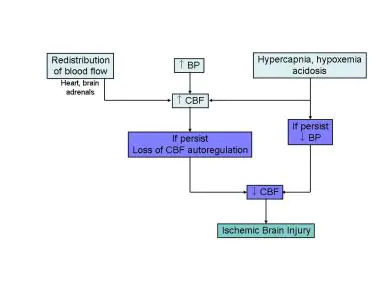
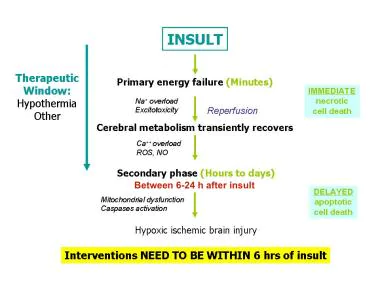
- Cause of HIE
- Neonates lack extensive autoregulatory mechanisms of cerebral blood flow regulation
- Respiratory (birth hypoxia), blood pressure, and metabolic disturbances affect brain oxygenation and require compensation of the cerebral vasculature to regulate perfusion
- Sufficient disturbances overwhelm the ability to autoregulate leading to ischemic injury
- Which part of the neonatal brain is most susceptible to hypoxic injury
- Subependymal germinal matrix: precursor to glial cells. These are packed full of mitochondria
Manifestation of HIE
- Patient History
- Preterm neonate
- Required resuscitation
- Acidotic
- Show neuroogical sequelae (hypotonia, seizures, lethargy/coma – within 24 hours)
- Cross-cutting Signs and symptoms
- Poor feeding
- Irritability
- Crying and lethargy
- Mild Signs and symptoms
- Increased muscle tone
- Brisk DTRs
- Moderate Signs and symptoms
- Hypotonia
- Diminished DTRs
- Diminished neonatal reflexes
- Seizures
- Possibly apnea
- Severe Signs and symptoms
- Comatose
- Hypotonia
- Diminished DTRs
- Diminished neonatal reflexes
- Apnea
Management
- Investigations
- Metabolic profile, including liver enzymes
- Cardiac enzymes
- ABGs
- Coagulation studies (PT/PTT/fibrinogen)
- Cranial ultrasound, diffusion weighted MRI
- Echocardiography.
- Treatment
- Resuscitation of fluid and electolyte imbalances. Stabilize BP: keep MAP >40 mmHg to prevent hypoperfusion
- Emergent neonatology consultation
- Feeding
- EEG: to monitor for asymptomatic seizures; appropriate tx
- Management of any concurrent complications
- Umbilical artery catheter placement; confirm w/XR
- Routine lab checks
Complications
- Immediate complications
- Seizures
- Intraventricular hemorrhage
- Long-term complications
- Cerebral palsy
- Epilepsy
- Cognitive deficits
- Blindness
- Hearing Impairment
