TORCH infections
| Specific Sx | Dx | Definitive Tx | |
|---|---|---|---|
| Toxoplasmosis | Diffuse calcifications on MRI, hydrocephalus | Toxo titers (IgM) | Pirimethamine and Sulfadizine + Leucovorin |
| Syphilis | Palm/sole rash, periostitis | VDRL-RPR; FTA-ABS, CSF analysis | Penicillin G |
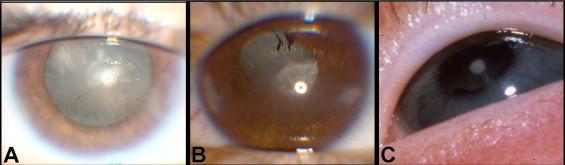
| Rubella | Cataract, deafness, heart defects (PDA), blueberry muffin rash | Rubella titres (IgM), Echo | Supportive |
| CMV | Periventricular calcification on MRI, TCP; more ill | Urine CMV PCR | Ganciclovir |
| HSV | Skin vesicles esp. eyes and mouth; encephalitis in some cases, septic appearance | Serum and CSF HSV PCR and culture | Acyclovir |
Congenital toxoplasmosis
Infection w/Toxoplasma gondii, acquired through acute maternal infections. Infections in immunocompetent adults are usually subclinical. Fetal damage is most likely to occur if infection is acquired during 2nd-6th month of gestation. Mothers who are exposed to toxoplasmosis or who work in high-risk environment can be given Spiramycin to reduce risk of transmission.
70% of infants are either asymptomatic or undiagnosed at birth. May go on later to develop sequelae (learning disability, mental retardation, and visual impairment)
- Sources of Toxoplasma gondii
- Handling undercooked meat
- Cat feces
- TORCH Signs and Symptoms
- IUGR/SGA
- Jaundice
- Hepatosplenomegally (HSM)
- Hydrocephalus
- Microcephaly
- Seizures
- Cataracts
- Chorioretinitis
- Visual impairement
- Investigations
- Toxoplasma antibody titres (IgM) from blood and CSF
- Blood and CSF cultures
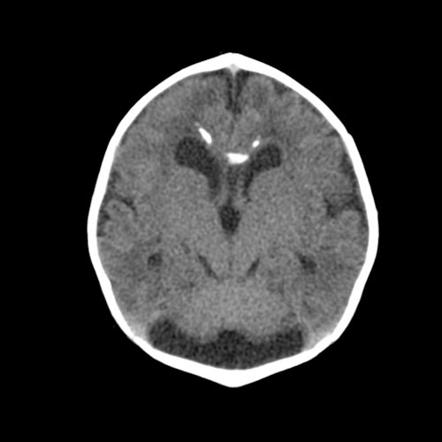
- MRI: diffuse intracranial calcifications
- Opthalmology exam
- Treatment
- Pyrimethamine and Sulfadizine+ Leucovorin

Congenital Syphilis
Infection with the spirochete Treponema pallidum in mothers who acquired syphilis during pregnancy, or had syphilis prior to pregnancy but wasn’t adequately treated.
- Early manifestations
- Jaundice
- HSM
- Coomb’s negative HA
- Snuffles
- Muocutaneous lesions of the palsm and soles
- Periostitis
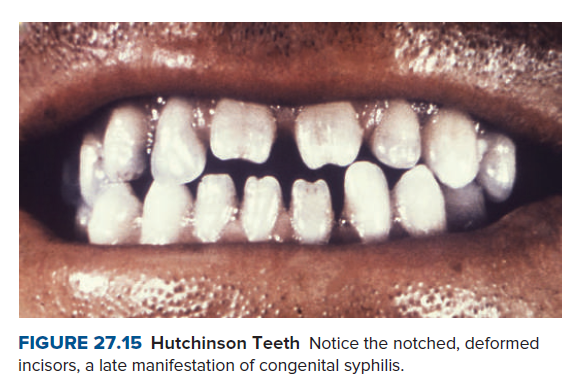
- Late manifestations (≥ 2yoa)
- Hutchinson’s teeth
- Saddle nose
- Frontal bossing
- Knee synovitis
- Interstitial keratitis
- Deafness
- Investigations
- VDRL-RPR of serum and CSF: best initial
- FTA-ABS: most accurate test, to confirm positive VDRL
- Treatm
- Penicillin G (higher dose if CSF diseae +)
- Treat mom too

Congenital rubella
Infections w/Rubella virus when mother contracts the virus during pregnancy (particularlyparticularly the first trimester). Less common d/t mass immunization. Ask mom if she has been vaccinated and how long since vaccination then ask if she might have had any possible infection (Sx rash, arthritis, adenopathy, fever)
- Manifestations
- IUGR/SGA
- HSM
- Jaundice
- Papular rash (”Blueberry muffin rash”)
- Cataracts
- Retinopathy
- Congenital Heart Defects (esp. PDA – ‘machine-like murmur)
- Sensorineural deafness
- Investigations
- Rubella titres
- Know mom’s immune status against Rubella
- Echocardiogram
- Opthalmologic exam
- Treatment
- Supportive
- No Tx for rubella infection
Congenital CMV infection
Infection w/ the cytomegalovirus (CMV). A vast majority of the population carries CMV and it’s associated antibodies. In immunocompetent patients, infection is inconsequential as antibodies are readily produced and can be shared with the fetus. It is problematic is a pregnant woman is exposed to CMV for the first time during her pregnancy (particularly the first half of pregnancy)
- Manifestations
- Baby looks ill at or within hours of birth
- IUGR/SGA
- Microscephaly
- HSM
- Jaundice
- Petechiae/rash (looks similar to blueberry muffin rash seen in cong. rubella)
- Sensorineural deafness
- Chorioretinitis
- Long-term sequelae including learning disabilities and MR
- Investigations
- Urine for CMV
- Cranial MRI: periventricular calcifications
- Treatment
- Prolonged Ganciclovir (reduces progression to deafness)
Congenital HSV infection
Infection w/HSV, that is causing or has caused genital herpes in the mother. Herpes lesions are very contagious with skin-skin lesions. A big red flag is when the mother is experiencing her first HSV outbreak (antibodies will not be sufficiently passed down to baby).
- Indications for C-Section in a mother with HSV
- Mother w/active infection
- Mother w/Histroy of HSV who has genital lesions suspicious of HSV
- Manifestations
- Cutaneous (40%): Localized eye, mouth, and skin lesions (present in first couple of weeks)
- CNS (30%): Herpes encephalitis, apnea, seizures (present in the first month)
- Disseminated (25%): Multiorgan disease, septic presentation (presents shortly after birth)
- Investigations
- Serum and CSF HSV PCR
- Treatment
- Acyclovir (60mg/kg/d)

Other newborn infections
Congenital varicella
Infection w/Varicela Zoster Virus. Most of the population is immune to VZV (received the disease or vaccinated) and would be highly unlikely to be infected again. Similar to CMV, fetal problems occur when the mother contracts the virus for the first time during pregnancy.
The timing of when during pregnancy the mother contracts VZV is very important
Fetal varicella syndrome: infection during 7-28 weeks of gestation. Affects CNS and MSK development. Can be dx clinically based on mother’s Hx of VZV infection (VZV embryopathy). Bbay is born stable (has acquired mom’s antibodies) but insults from the virus in utero will manifest.
- Manifestation of Fetal varicella syndrome
- Limb hypoplasia (clavicle, scapula)
- Rib anomalies
- Scoliosis
- Umbilical hernia
- Microcephaly
- Cortical atrophy
- Seizures
- Chorioretinitis
- Mircropthalmia
- Hypoplasia of the optic disk
- Circatrical cutaneous scarring (in a dermatomal distribution)
- Investigations
- VZV titres: positive indicate exposure.
- Treatment
- Supportive (there is no active viral infection)
- 30% die in the first month of life

Neonatal varicella syndrome: infection within 2 weeks prior to delivery (highest risk at 5 days prior to or 2 days after deliver). Involves a progressive vesicular rash (baby was not in utero enough to obtain maternal antibodies). Dx is clinical.
- Manifestation of Neonatal varicella syndrome
- Progressive vesicular rash
- Ill-appearing
- Temperature instability
- Treatment
- VZIG (best treatment)
- IV Acyclovir

Group B Strep (GBS) infection
GBS is carried by 10-30% of women of child-bearing age as part of their normal vaginal flora. Most of these women have circulating IgG antibodies against GBS. Problem comes in when women who carry GBS in their vaginal flora do not have circulating anti-GBS IgG (their babies won’t have passive immunity against GBS even though they will be exposed in the birth canal) Sequalae of infection can occur early (<7 days) or later (>7days – 4 months) . Culture for Dx of GBS infection is paramount.
- Screening
- Culture all women at 35-37 wog (rectal and vaginal for GBS)
- If positive treat w/ IV antibiotics during labor and delivery process to reduce the chance of neonatal infection.
- Risk factors for GBS infection.
- GA <37 wog (Premature)
- ROM . 18 jours
- Young maternal age
- OBHx of previous baby w/GBS infection
- Signs and symptoms of Early onset neonatal GBS infection (<7 days)
- Onset typically within 48 hrs of birth
- Apnea
- Ill-appearing
- Irritable
- Temperature instability
- Sx consistent w/shock
- Signs and symptoms of Late onset neonatal GBS infection (7days – 4 months)
- Ill-appearing
- Meningitis
- Pneumonia
- Sepsis
- Other focal infections (eg. cellulitis, AOM, Conjunctivitis)
- Investigations
- CXR: diffuse, homogenous, ground glass infiltrates (may look like NRDS)
- CBC: leukopenia w/left shift
- Blood cx, CSF cx: Positive
- Treatment
- Broad spectrum ABX (Benzyl-penicillin and either Gentamicin OR Cefotaxime)
- When to consider Cefotaxime over Gentamicin
- Meningitis
- Spinal tap suggestive of Meningitis
Neonates born to mothers with HIV
All mothers should be screened for HIV as part of their routine prenatal care. Elective C-Section may reduce the risk of transmission. Recommended to breastfeed up to 2 years with protection (still exclusively breastfed up to 6 months).
- When can elective C-section reduce the risk for transmission
- C-section before rupture of membranes
- Neonatal HIV testing (Rapid antibody test and HIV DNA PCR)
- HIV testing can be conducted at birth or at first contact (within 2 weeks of birth)
- Follow-up testing is conducted at 6 weeks during immunization (HIV DNA PCR)
- Neonatal HIV prophylaxis
- AT + NVP for 6 weeks
- NVP is then continued up to 6 weeks after cessation of breastfeeding
- HAART (if mother was not on HAART during pregnancy)
Neonates born to mother with Hepatitis B
All mothers should be screened for HBsAg as part of routine antenatal care. 95% of transmissions occur during delivery. Hepatitis B is not a contraindication to breastfeeding.
- Risk factors for increased transmission
- HbeAg positive and HbeAb negative
- High serum levels of HbcAb
- High serum levels of HBV DNA
- Treatment of neonates born to HBsAg+ others
- Hepatitis B immune globulin within 24 hours of birth
- Hepatitis B vaccine as per schedule
Neonates born to mothers with gonorrhoea or chlamydia
Gonorrhea and Chlamydia can be tested for during routine antenatal screening. Neonates get infected as the pass through the birth canal.
- Manifestation
- Conjunctivitis
- Ophthalmia neonatorum (Gonococcal conjunctivitis): purulent and copious
- Chlamydial conjuncitvitis: less purulent, more hyperemia
- Pneumonia (caused by Chlamydia)
- Wheeing
- Stacatto cough
- No fever
- Sepsis, Arthritis, AND Meningitis (for N. gonorrhea)“
- Conjunctivitis
- Investigations
- CXR
- Hyperinflation
- minimal infiltrates
- Rapid Antigen Detection test for nasopharyngeal secretions
- CXR
- Prevention of conjunctivitis
- Tetracycline Eye Ointment or Doxycycline Ointment
- Treatment of pneumonia
- Oral Erythromycin for 2 weeks
