Overview
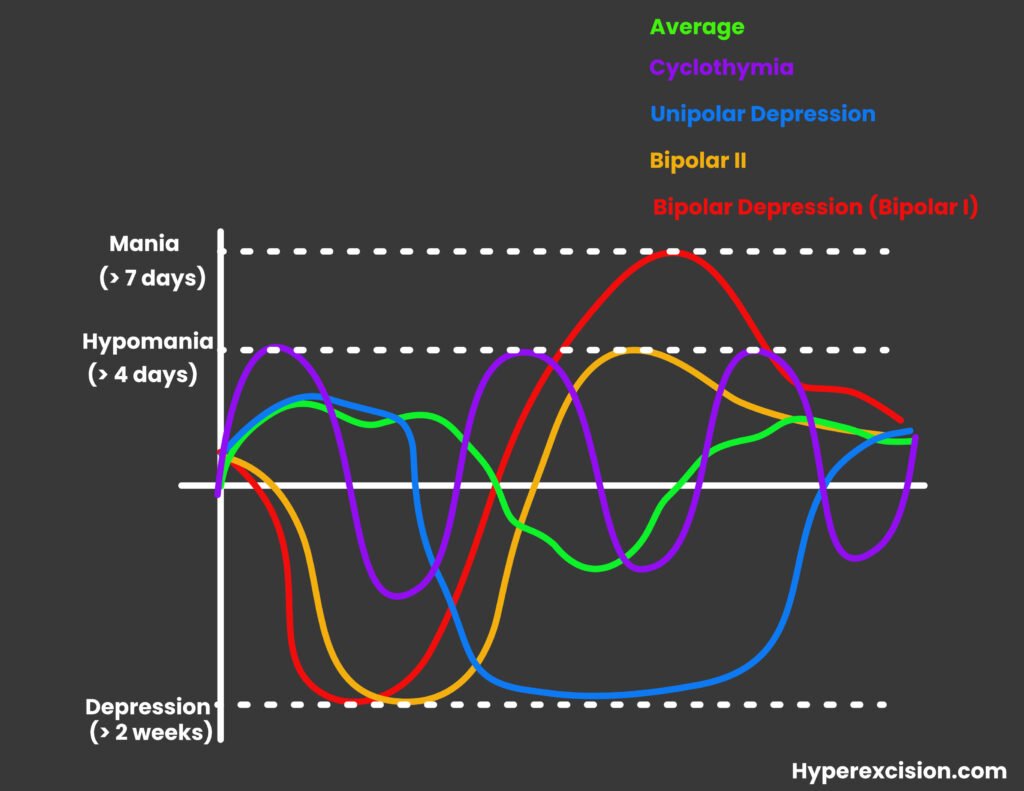
Variations in mood are normal. Mood can fluctuate from day to day and very few people will be the same on a day-to-day basis. Mood disorders (as defined by the pattern of mood episodes) happen when the patient’s mood becomes uncontrollable and causes impairment in daily life. They include major depressive disorder (unipolar depression, MDD), bipolar 1 disoder (bipolar depression), bipolar 2 disorder, cyclothymia, persistent depressive disorder (formerly dysthymia), among others. Some mood disorders can present with psychotic features (delusions, hallucinations)
Definition of terms
| Term | Definition |
|---|---|
| Mood | A description of one’s internal emotional state. This is how the patient feels. It is pervasive and sustained and usually influences a person’s behavior or influences their perception of the world. Can gauge by asking the patient to rate their mood on a scale of 1-10. |
| Affect | The external display of one’s mood. This is how you perceive the patient. It is varies over time and changes according to the patient’s emotional state. Can be mood congruent or mood incongruent. |
| Mood episode | A distinct period ot time in which an abnormal mood is present |
| Mood disorders | A pattern of mood episodes. Some may be accompanied by psychotic features. |
- Why do mood disorders seem to affect women more than men?
- Cultural bias
- In most cultures women tend to be more open about their feelings
- Clinicians tend to be more attentive to feelings in women than in men
- Men are more likely to complain about things that surround their mood (”I can’t sleep at night”) rather than the mood itself (“I’m feeling down”)
- Mood disorders
- Major Depressive Disorder (Unipolar Depression)
- Bipolar I Disorder (Bipolar Depression)
- Bipolar II Disorder
- Persistent Depressive Disorder (PDD)
- Cyclothymia
- Premenstrual Dysphoric Disorder
- Puerperal Depression
- Depressive disorder due to medical condition
Mood Episodes
Major Depressive Episode
- ≥ 5 of SIG E CAPS for at least 2 weeks (symptoms must include low mood and anhedonia)
- Sleep changes (Hypersomnia or insomnia)
- Interest (Loss thereof; Anhedonia = loss of pleasure )
- Guilt (feelings of worthlessness rather than guilt in the elderly)
- Energy (Lack of energy; can be related to sleep changes)
- Concentration (Lack of concentration; distractibility)
- Appetite (Change in appetite – can be eating less or more)
- Psychomotor (Agitation or retardation)
- Suicidality (Passive or active suicidation. Passive suicidal ideation is more common. Active suicidal ideation the patient has a plan and needs to be hospitalized. Pre-occupation with death)
- Cardinal Symptoms (the big 2)
- Depressed Mood
- Anhedonia
Manic Episode
- DIG FAST for at least 7 days (at least 3 symptoms, 4 if the mood is irritable)
- Distractability (easily distracted)
- Insomnia
- Grandeur (Arrogance)
- Flight of ideas (tangiental, can’t stay focused)
- Activity (increase in activity, increase in activity)
- Sleep (decrease in sleep. Does not cause fatigue)
- Talkativity
- Signs and symptoms of mania
- Racing thoughts (Manifests as Flight of ideas in speech)
- More talkative (Manifests as Pressured speech)
- Extremely “high” (Manifests as Euphoric mood/affect)
- Easily irritated
- Easily distracted
- Decreased need for sleep (sleep 2-3hours, wake up energized)
- Inflated self-esteem (Grandiosity – unrealistic beliefs in one’s ability and power)
- Excessive energy with increased activity (goal-directed or purposeless)
- Poor judgement
- Excessive pleasurable activity (Libido, Drugs, Deals, Spenging)
- Delusions or Hallucinations (in severe cases. Insight I/II – never VI; mood congruent, usually auditory hallucinations)
- Clues pointing to mania
- Clothing may reflect mood (Colouful and excessive – the patient may have a lot of accessories, colourful hair)
- Self-neglect in severe cases (untidy/dishveled)
- Exhausted
- Unfinished tasks
- Increased appetitie
- Increased sexual drive
Hypomanic Episode
A mild form of mania (requires at least 3 DIG FAST) that DOES NOT cause disturbance in the patient’s life. No psychosis. Mild impairment of performance or judgement.
Requires at least 3 DIG FAST symptoms for 4 days
- Why do patients with hypomania ( or BPIID) have a worse prognosis than BPID
- They rarely seek treatment and relapse frequently into MDD
Mania vs Hypomania
| Mania | Hypomania | |
|---|---|---|
| Severity | Severe | Mild |
| Social function | Marked impairment in social function | Mild impairment in social function |
| Mood disorder | Bipolar I disorder | Bipolar II Disorder, Cyclothymia |
| Duration | Lasts at least 7 days | Lasts at least 4 day |
| Hospitalization | Hospitalized | Treated as outpatient |
| Psychosis | Yes. Delusions and hallucinations | No psychosis |
| Electroconvulsive therapy | ECT plays a role in treatment | ECT does not play a role in treatment |
| Pharmacotherapy | Antipsychotic +/- mood stabilizers | Mood stabilizers are enough |
Disruptive mood dysregulation disorder
This diagnosis reserved for children who exhibit persistent irritability (>12 months) – particularly temper outbursts and anger more than 3 times per week in more than two settings



