Table Of Contents
Hypothermia
Hypothermia is defined as a core body temperature less than 36 degrees Celsius. Core body temperature can be measured in the nasopharynx, distal eosophagus, tympanic membrane and pulmonary artery. Skin is generally much cooler than core temperature.
- Pathway of thermoregulation
- Afferent nerves travel along A-delta (cold) and C (warm) fibres via the spinothalamic tract → pre-processing occurs in the spinal cord and brainstem → thermal inputs ultimately reach the pre-optic anterior hypothalamus
Mechanisms to control body temperature
| Response | Examples |
|---|---|
| Behavioral | Seeking shelter or clothing, voluntary movement |
| Autonomic | Shivering, Sweating, Modulating vascular tone |
Interthreshold range: the core temperature range between cold-induced and warm-induced responses, usually as narrow as 0.2 C.
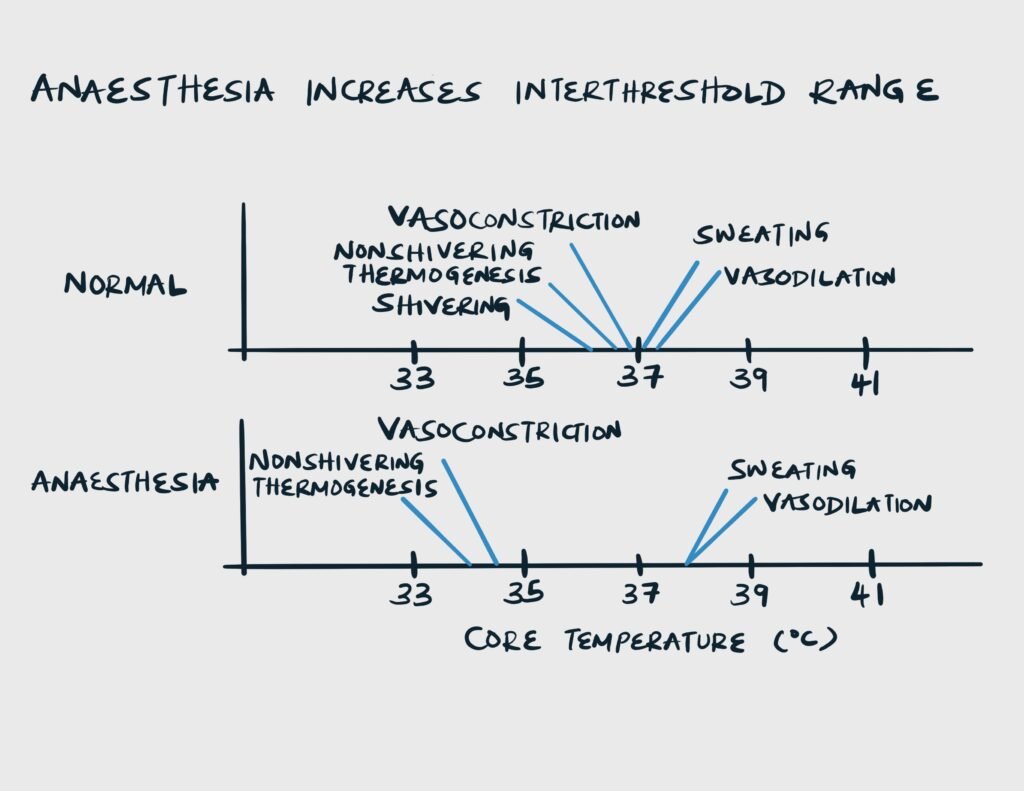
Effects of Anaesthesia on the interthreshold range
| Anaesthesia | Effect |
|---|---|
| General anaesthesia | inhibits thermoregulation globally. Increases interthreshold range 20-fold to around 4 C. |
| Regional anaesthesia | inhibits thermoregulation to the lower half of the body. Increases interthreshold range 4-fold (around 0.8 C) |
Phases of Anaesthetic impaired thermoregulation
| Phase | Event |
|---|---|
| Phase I | Redistribution hypothermia |
| Phase II | Heat loss > heat production |
| Phase III | Heat loss – heat production. Heat balance is at steady state |
- Heat transfer in the operating room (in order of importance)
- Radiation
- Convection
- Evaporation
- Conduction
- Benefits of hypotehrmia
- Decreases metabolic rate by 8% per 1 C decrease in body temperature: myocardial protection
- Partial protection to the CNS from ischemic and traumatic injuries: improved neurologic outcome after cardiac arrest and allows deep hypothermic circulatory arrest for certain cardiac surgeries (complex aortic arch repair)
- Protection against malignant hyperthermia
- Disadvantages of Hypothermia
- Increases infection rates up to 3 fold
- Delays wound healing and increases risk of surgical graft failure
- Induces coagulopathy (part of the trauma lethal triad)
- Delays emergence from general anaesthesia
- Impairs oxygen delivery by causing left-shift of the oxygen-hemoglobin dissociation curve
- Negative effect on ionotropy and chronotropy, increases EKG interval, leads to dysrhythmias, and increased systemic vascular resistance
- Increases systemic stress response
- Increases post-operative shivering rates
- Prolonges PACU stay
Warming strategies – prevention of hypothermia is more effective than treatment
| Strategy | Examples |
|---|---|
| Active warming | Forced air, Heating pad with circulating water, Breathing circuit heating and humidification, IV Fluid Warmer, Bladder Irrigation with warm fluids, Heating lamp, Raise room temp |
| Passive Insulation | Cotton blanket, surgical drapes, heat-reflective “space” blanket |
Shivering
- Causes of shivering in PACU
- Hypothermia (keep in mind that lack of shivering does not mean the patient is hypothermic. Remember opioids and anesthetics can increase the interthreshold range)
- Uncontrolled pain (non-thermoregulatory driven shivering)
- Other differentials for rhythmic muscular activities
- Pure clonic movements (seen in patients as volatile MAC drops to 0.15 – 0.3 range regardless of temperature)
- Fevers
- Seizures
- Effects of shivering
- Increases Oxygen consumption (upto 500 % increase)
- Increases CO2 production (this increases minute ventilation requirment)
- Associated with trauma, elevated intraocular pressure, and elevated intracranial pressure
- Can be distressing or painful
- Disrupts monitoring (oscillometric BP measurement and pulse oximetry)
- Treatment of shivering
- Warm the patient aggressively (forced air and blankets)
- Meperedine 12.5 – 25 mg IV (note that meperedine can accumulate in renal insufficiency leading to seizures)
- NDMB (only in anaesthetized and mechanically ventilated patients)
- Ensure pain is well controlled
- Ensure the patient is not seizing
- What is the most effective way to reduce the amount of heat lost due to redistribution from core to periphery during the first 30 minutes after induction?
- Pre-operative forced air warming to torso and legs 30 min before induction




