Tidy vs Untidy wound
| Type of wound | Characteristic | Examples | Healing |
|---|---|---|---|
| Tidy wound | Incised, Clean, no tissue loss | Surgical incision, Stab, Cuts | Primary intention |
| Untidy wounds | Irregular, tissue loss, devitalized tissue, contaminated | Crush, Avulsion/Degloving, Burn | Secondary intention |
Open wounds
The skin has been breached and underlying tissue is exposed
| Wound | Description |
|---|---|
| Clean incision | Tidy, simple, clean cut wound with linear edges |
| Cut | Wound with uneven edges due to a combination of sharp and blunt forces |
| Abrasion | Shallow, irregular wound involving superficial skin layers that results from skin contact with a rough surface or any surface at high speed |
| Laceration | Deeper, tear-like wound, often with irregular edges, typically caused by sharp trauma or focused blunt trauma |
| Avulsion | Tissue is forcibly detached from its normal attachment or insertion |
| Puncture | Small rounded wound that results from thin, pointed objects |
| Penetrating wound | Wound caused by any object that breaks through the skin to underlying tissue or organs |
Closed wounds
The skin is intact, but the underlying tissue has been damaged
| Wound | Description |
|---|---|
| Contusion | Wound caused by direct blunt trauma that causes damage to small vessels and capillaries producing bruising (skin discolouration) in subcutaneous tissue |
| Hematoma | Wound caused by trauma that damages small vessels and capillaries allowing blood to collect in a potential space |
Mechanism of injury
| Mechanism | Examples |
|---|---|
| Mechanical wound | Abrasion, puncture, incision, cut, crush, tear, bite wound, gunshot wound |
| Chemical wound | Due to acids and alkali |
| Radiation wound | Due to radiation exposure |
| Thermal destruction | Burn or frostbite |
Primary, Secondary, and Tertiary intention
Types of wound healing
| Type of healing | Description | Example of wound |
|---|---|---|
| First intention | Wound edges are approximated by suturing, staples, or adhesive | Surgical wound, clean incision |
| Secondary intention | The wound heals slowly by granulation tissue and scar formation and closes by re-epithelialization | Traumatic wound, highly contaminated wound, extensive soft tissue loss |
| Tertiary intention (Delayed primary closure) | The wound is treated by repeated debridement and finally approximated | Traumatic wound with high infection risk |
Healing by primary vs secondary intention
| Primary intention | Secondary intention | |
|---|---|---|
| Tissue deficit | Smaller | Larger |
| Mechanism of healing | Epithelial regeneration | Granulation tissue. Pale, avascular scar formation |
| Myofibroblast contraction | Minimal | Marked |
| Fibrin clot | Smaller | Larger |
| Inflammation | Less intense | More intense |
| Secondary inflammation mediated damage | Less potential | More potential |
| Granulation tissue | Small amounts | Larger amounts |
| Scar tissue | Smaller mass | Greater mass |
| Exudate | Less exudate | More exudate |
| Necrotic debris | Less | More |
Ulcer
An ulcer is a chronic wound that is defined as a break in the continuity of the covering epithelium in either skin or mucous membranes due to molecular death. The most common ulcers are venous, arterial, or mixed ulcers. These three account for 70% of all ulcers while 50% are caused by venous stasis alone.

Location of ulcers based on etiology
| Ulcer | Description | Common Location |
|---|---|---|
| Neuropathic and Traumatic ulcers | Due to loss of sensation → inability to withdraw from painful stimulus or trauma → repeated trauma → ulceration | Pressure bearing regions |
| Venous (Varicose) ulcers | Due to hypoxia. Painful, easily recur and persist for many years. | Medial and lateral malleoli |
| Arterial ulcer | Due to ischemia caused by atherosclerosis or peripheral arteries. Appear punched out and well demarcated with round shape and pale, non-granulating, often necrotic base | Dorsum of the toes, dorsum of the foot, and in-between toes |
| Diabetic ulcer | A mixed ulcer due to ischemia + neuropathic changes + systemic metabolic dysfunction + immune dysfunction causing ulceration and impaired healing | No particular site since any ulcer with imaired healing (neuropathic/arterial/traumatic/varicose) due to diabetes is termed a diabetic ulcer. However bullae tend to appear in the nape and back. |
| Decubitus (Pressure) ulcers | Mechanical pressure compresses arterioles and venules causing ischemia and hypoxia | Back of head, shoulder, elbow, hip, sacrum, ischial tuberosity, greater trochanter, medial and lateral condyles, malleoli, and heels |
- Features suggestive of malignancy in ulcers
- Margins: Irregular with nodules
- Egde: Everted edges
- Floor: red and bleeds easily on palpation
- Surrounding skin: inflammed and indurated (hard)
- Investigations for patients with chronic ulcers
- CBC: look for anemia
- ESR: monitor for infection
- RBS and HbA1C: for glycemic control
- U/E/Cs: for uremia
- VDRL: for syphillis
- HIV: for HIV
- Chest X-ray: for TB
- EKG: to rule out IHD if atherosclerosis is suspected
- Local smear for culture
- X-ray of the affected part
- 4 quadrant edge biopsy
- Stigmata of Tuberculosis to look out for in a patient with an ulcer
- Phlyctenular conjunctivitis
- Matted Lymphadenopathy
- Scars and Sinuses in the neck
- Stigmata of Leprosy to look out for in a patient with an ulcer
- Hypopigmented, anesthetic patches
- Thickened ulnar posterio tibial, and great auricular nerves
- Trophic ulcers (pressure ulcer)
- Deformed phalanges
- Leonine facies (due to collapse of the nasal bridge and lateral 1/3 of eyebrows)
Diabetic ulcer
- 4 ways in which diabetes impairs healing of ulcers
- Hyperglycemia promotes the proliferation of bacteria and glycosylates collagen making it brittle
- Decreases blood supply to the ulcer due to small and large vessel disease
- Ulcer is prone to repeated, unnoticed trauma as a result of neuropathy
- Deficient fibroblast reaction
Wagner Grading of diabetic foot ulcers
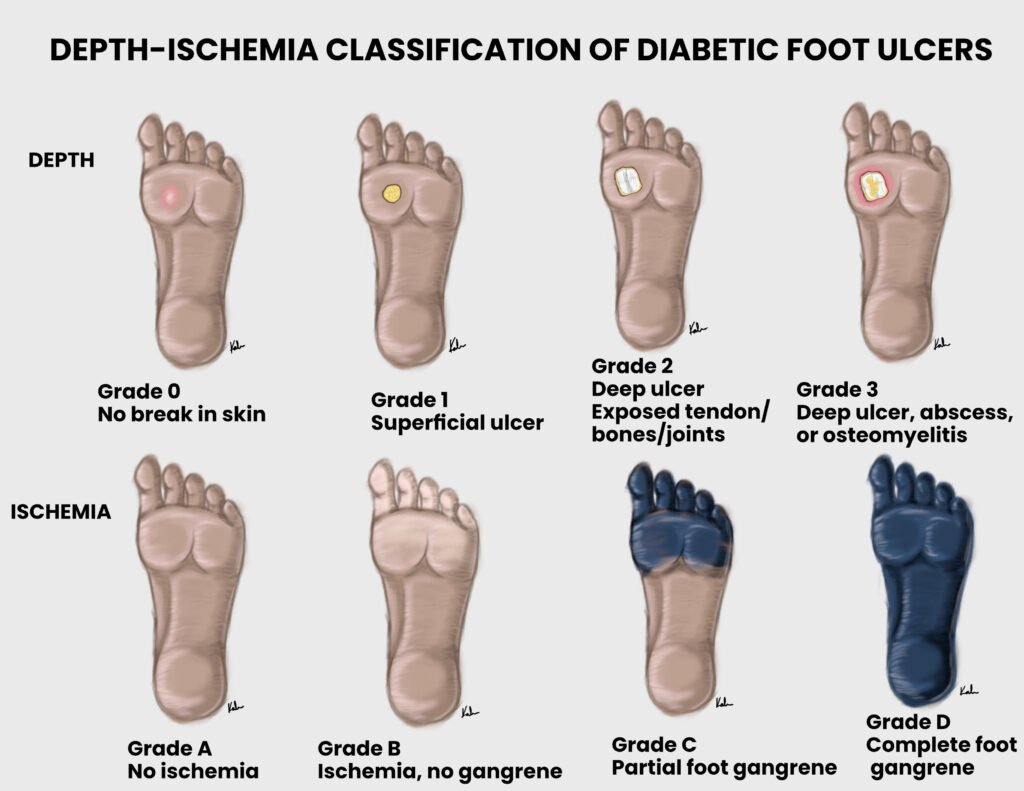
| Grade | Description |
|---|---|
| Grade 0 | Intact skin |
| Grade I | Superficial ulcer |
| Grade II | Deep ulcer |
| Grade III | Ulcer with abscess or bone involvement or osteomyelitis |
| Grade IV | Forefoot gangrene (localized) |
| Grade V | Full foot gangrene (extensive) |
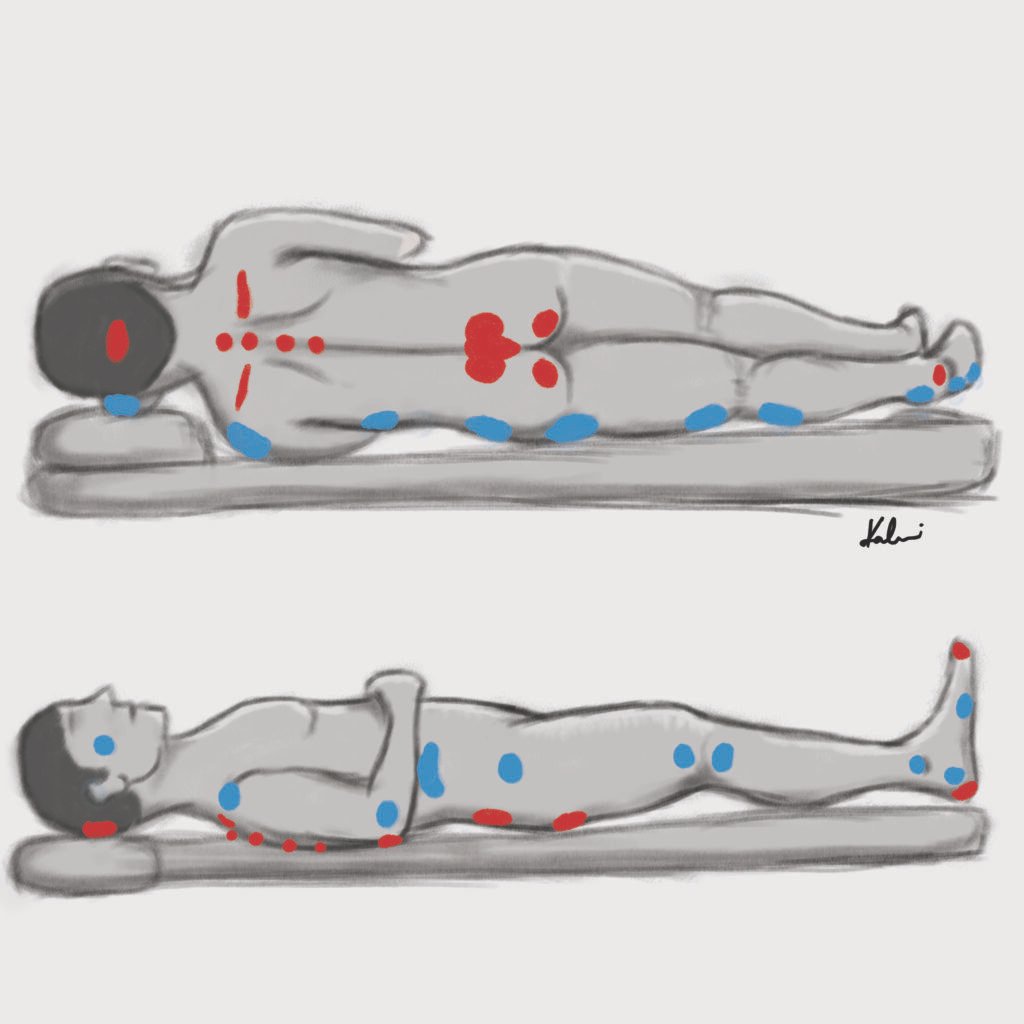
Decubitus (Pressure) ulcers

Staging of decubitus ulcers
| Stage | Description |
|---|---|
| Stage I | Intact skin. Change in color, consistency, or temperature |
| Stage II | Partial-thickness loss of skin involving the epidermis and dermis |
| Stage III | Full-thickness skin loss including subcutaneous tissue but not fascia |
| Stage IV | Damage to muscle, bone, and other supporting tissue, may have undermining of tissue |
- Risk factors for development of pressure ulcers
- Sensory deficits
- Moisture
- Immobility
- Inactivity
- Malnutrition
- Friction and shear
- Prevention of pressure ulcers
- Reduce external pressure
- Reposition every 2 hours
- Pillows or thick padding areas at risk
- Keep the skin clean and dry
- Adequate pain relief to allow for activity and mobility
- Manage systemic conditions that place the patient at risk of developing pressure ulcers
- Reduce external pressure
Gunshot Wound (GSW)
The higher the projectile velocity of a missile, the greater the damage. Low velocity missiles from pistols drill only narrow tracks with little damage around them. in addition to causing extensive cavitation, high velocity missiles form a partial vacuum in their path that sucks in debris. Missile wounds may take curious paths. They may be deflected by bone, or be influenced by the position of the patient at the time of injury. A multi-disciplinary care team is required for GSW. GSW should not be closed primarily. Delayed primary closure after initial debridement, or healing by secondary intention is preferred. Bullets and fragments are removed only where indicated. Gunshot wounds are discussed more in depth in the forensic medicine cheat sheets.
Types of injury
| Type of injury | Weapon | Projectile velocity |
|---|---|---|
| Low velocity | Handgun, some rifles | < 350 m/s (1200 fps) |
| Medium velocity | Shotgun: potential for massive soft tissue destruction. The wad may stay in the wound and form a nidus of infection | 350 – 650 m/s (1200 – 2100 fps) |
| High velocity | Military or Hunting rifles | > 600 m/s (>2000 fps) |
- Complications of GSW
- Compartment syndrome: common after high velocity wounds. More common with proximal fractures of the forearm
- Vascular injury: findings include pulsatile bleeding, absent pulse, bruit, thrill. ABI and angiography can be performed if there is concern.
- Spinal injury: GSW is the 3rd most common cause of spinal injury. Cervical spine GSW can be associated with airway compromise (84%)
- Infection: GSW tracts are non-sterile. 24 hours IV antibiotics (1st gen cephalosporins) for low-velocity injuries (Gustillo I/II) and 72 hours IV antibiotics (1st gen cephalosporin + gentamicin) for high-velocity injuries (Gustillo III)
- Fractures: Low velocity injuries can be treated as Gustilo I/II while high velocity injuries can be treated as Gustilo III. GSW has increased comminution and greater soft-tissue stripping and bone loss.
- Retained projectiles and fragments: retained fragments can be left in situ. Indications for removal include: intra-articular, intra-vascular, subcutaneous, lead toxicity, peri-spinal and peri-neural
- Compartment syndrome
- Common after high velocity wounds due to soft-tissue trauma/bleeding/oedema
- More common with proximal fractures of the forearm
- Vascular injury and hemorrhage
- Findings include pulsatile bleeding, absent pulse, bruit, thrill
- Damage control surgery e.g. shunting can be performed
- ABI and Angiography can be performed if there is concern
- Peripheral nerve injury
- Majority of nerve dysfunction is neuropraxia, particularly in low velocity wounds
- Life-saving interventions in GSW
- Hemorrhage control and resuscitation
- Chest tubes (even bilateral chest tubes)
- Laparotomy
Classification Surgical Wounds
Colonized body cavities = respiratory, alimentary,, genital, or urinary tracts
| Wound | Description | Example | Infective rate | Need for prophylaxis |
|---|---|---|---|---|
| Clean wound | Elective wound. Primarily closed withour drain. No opening of colonized body cavities. No break in sterile technique. | Hernioplasty, Excisions, Thyroidectomy, Brain surgery, Joint surgery, arterial and venous surgery, heart surgery | 1-5% | No |
| Clean contaminated wound | Elective wound. Controlled opening of normally colonized body cavities. Minimal spillage. No break in the sterile technique. | Appendicectomy, Gastrojejunostomy, Pancreaticobiliary surgeries, Lung resection, Cholecystectomy, Gastrectomy, Prostatectomy | 3-11% | Prophylaxis may be required |
| Contaminated wound | Acute, non-purulent inflammation. Break in sterile technique or spillage from hollow organs. Open, fresh accidental wound. | Penetrating trauma < 4h from injury, Chronic open wound, acute abdomen, removal of acute appendicitis, open cardiac massage during a case | 10-17% | Prophylactic antibiotics required – 1 hour prior to incision, 2nd and 3rd dose q8h |
| Dirty wound | Purulent abscess. Traumatic wound from a dirty source with retained, devitalized tissue. Surgical wound involving existing infection or free perforation. | Penetrating trauma > 4 hours from injury, abscess, perforated viscus with peritonitis, fecal peritonitis | 27-40% | Treatment required instead of prophylaxis |



