Overview
Chronic obstructive pulmonary disease (COPD) is defined as a disease state characterized by persistent respiratory symptoms and airflow obstruction. 75% of COPD patients are long-time smokers. COPD includes emphysema and chronic bronchitis and most patients have features of both. It has a wide age range for diagnosis but early symptoms can be apparent in the 30s. Diagnosis is clinical, but it is best to confirm with Pulmonary Function Tests (PFTs). Definitive diagnosis is via biopsy.
| Obstructive Pulmonary Disease | Description |
|---|---|
| Emphysema | Due to destruction of alveoli from chronic inflammation → loss of elasticity + decreased surface area for oxygen exchange (DLCO) |
| Chronic bronchitis | Excessive secretion of mucus with daily productive cough for at least three months in at least two consecutive years |
| COPD excacerbation | Acute worsening of symptoms often brought on by infection, heart failure, air pollution, or idiopathic factors. Defined as Increased dyspnea from baseline AND/OR increased sputum production |
- Risk factors for COPD
- Cigarette smoking
- Advanced age
- Race (White > other races)
- Exposure to air pollution
- Occupational exposure (dust, chemicals, pesticides, vapor, fumes, or gases)
- Symptoms
- Productive cough
- Shortness of Breath
- Progressive dyspnea on exertion
- Wheezing
- Physical Exam
- Barrel chest
- Hyper-resonance (due to air-trapping)
- Wheezing (emphysema)
- Coarse crackles (due to the mucus in chronic bronchitis)
- Late presentation
- Cyanosis
- Clubbing
- Loud P2 sound (due to pulmonary hypertension)
- Increased jugular venous pressure (Cor Pulmonale)
- Differentials
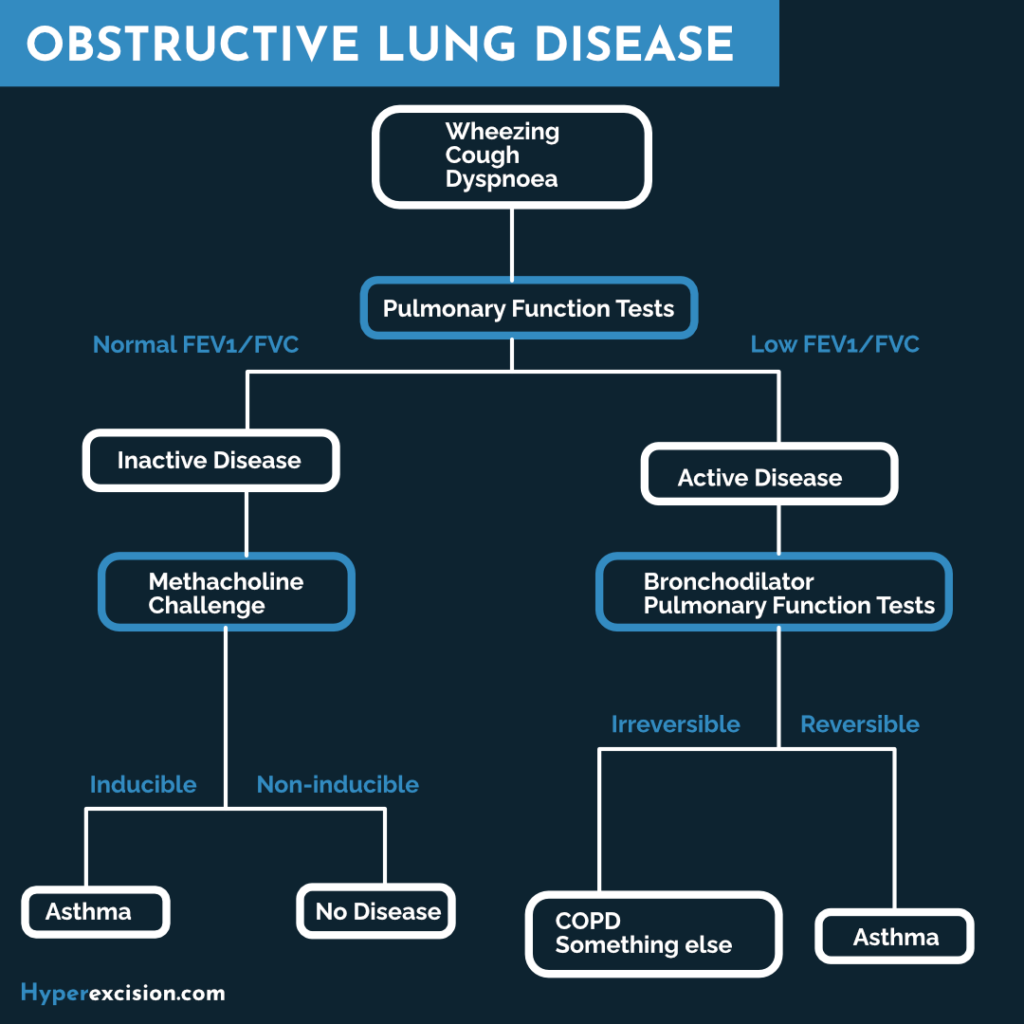
- Asthma: COPD is generally not reversible with a bronchodilator. Asthma presents younger
- Cystic fibrosis: suspect in a child. Meconium ileus, malabsorption
- Alpha-1 antitrypsin deficiency: Suspect in a non-smoker or patient under 40 years old. Get serum A1AT levels
- General investigations for a patient who presents with shortness of breath
- Chest X-ray
- Cardiac Enzymes
- Electrocardiogram
- Complete Blood Count
- BNP
- Echocardiogram
- Chest CT with Contrast
- RSV antigen
- D-dimer
- Investigations
- PFTs/Spirometry: Obstructive pattern
- FEV1: Low (prolonged expiratory phase)
- FVC: Normal/low
- FEV1/FVC ratio: Low (very characteristic of obstructive pattern)
- TLC: normal/high (due to air trapping)
- DLCO: Low (normal in asthma because they can still exchange oxygen fine)
- ABGs: +/- CO2 retention
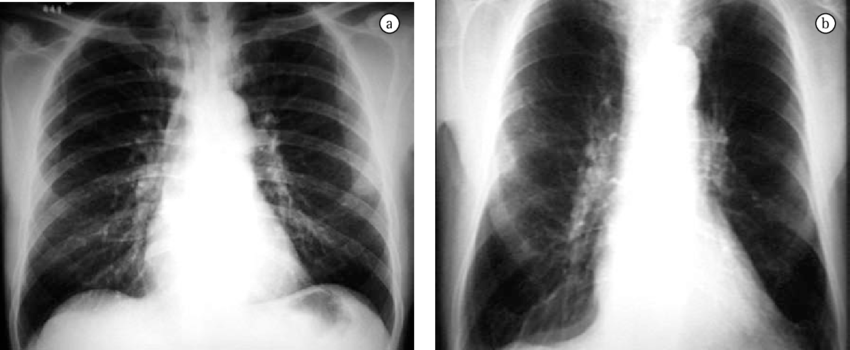
- Chest X-ray
- Diaphragmatic flattening
- Elongated heart (Right ventricle hypertrophy seen late
- Substernal air trapping (if you can see 10 ribs = hyperinflation)
- Chest CT
- Saber sheath trachea (trachea with coronal dimension ≤ 2/3 sagittal dimension – pathognomonic for COPD)
- Electrocardiogram
- Low QRS amplitude
- Signs of right ventricular hypertrophy (right axis deviation; late on your way to Cor Pulmonale)
- Echocardiogram: if there are signs of CHF
- PFTs/Spirometry: Obstructive pattern
- What is the first PFT parameter to change in COPD?
- FEV (25-75)
- Chest X-ray Findings in COPD
- Flattening of the diaphragm
- Elongated heart (right ventricular hypertrophy)
- Substernal air trapping
- Spirometry changes in COPD
- FEV1: low
- FVC: normal/ low
- FEV1: FVC ratio: low
- Total lung capacity: normal/ high
- DLco: low
Restrictive vs Obstructive lung diseases (spirometry)
| Obstructive | Restrictive | |
|---|---|---|
| FEV1 | Low | Normal/ low |
| FVC | Normal | Low |
| FEV1/ FVC | Low | Normal/ high |
| Total lung capacity | Normal/ high | Low |
Management
Treatment Goals and Methods in COPD
| Acronym | Component | Description |
|---|---|---|
| C | Corticosteroids | Inhaled maintenance, IV exacerbation. No change in mortality unless the patient has an infection. |
| O | Oxygen | When PaO2 < 55 or SpO2 <88%. Titrate to PaO2 55-60, SpO2 > 90% |
| P | Prevention | Vaccines: Pneumovax q5y and Influenza q1y. Smoking Cessation. These decrease mortality. |
| D | Dilators | Anticholinergics > Beta Agonists. Rescue inhaler → Nebuliser → Continuous (inpatient) |
| E | Experimental | Out of scope 😬 |
| R | Rehabilitation | Increased exercise tolerance, Reduced dyspnea and fatigue, No change in mortality |
Escalation of Therapy in COPD
| Step | Therapy |
|---|---|
| 1 | SABA |
| 2 | SABA + Tiotropium |
| 3 | SABA + Tiotropium + ICS |
| 4 | SABA + Tiotropium + ICS + LABA |
| 5 | SABA + ICS + LABA + DPE-4-inhibitor |
| 6 | … Add Oral Steroid |
- Treatment
- Smoking cessation
- Long-acting Beta Agonist (LABA) (salmeterol, formoterol) + Long-acting Muscarinic Agonist (LAMA) (tiotropium, ipratropium) inhalers
- Pneumococcal vaccine q1y
- Influenza vaccine q1y
- When should home oxygen be considered?
- PO2 <55mmHg, SpO2 < 88% (titrate to 90, do not exceed 95%)
- Cor Pulmonale + PO2 <60 mmHg, SPO2 < 90%
- What should you not do for patients with COPD?
- DO NOT administer expectorant or mucolytics (e.g. Guaifenesin)
- DO NOT administer cough suppressants (e.g. Dextromethorphan; we want them to cough and remove whatever is in their bronchi)
- Discharge instructions
- Smoking cessation
- Home oxygen if needed
- Pneumococcal vaccine q1y
- Influenza vaccine q1y
COPD Exacerbation
COPD exacerbation is a bread-and-butter case in internal medicine. They are episodes of acute worsening of symptoms associated with increased airway and systemic inflammation and physiological changes (especially the development of hyperinflation) mainly triggered by viral and bacterial infections. 30% are idiopathic. Always stabilize the patient first then treat with bronchodilators, systemic corticosteroids, and prophylactic antibiotics.
- Symptoms
- Sustained worsening of baseline symptoms:
- Dyspnea
- cough
- sputum production
- Sustained worsening of baseline symptoms:
- Physical exam
- Decreased breath sounds
- Wheezing
- Hyperinflation (Hyper-resonance)
- Assessing the patient’s stability
- Vital signs (SpO2, Temperature >30.5 C suggests bacterial pneumonia)
- Mental status (in a patient who is not oxygenating well)
- Respiratory distress (accessory muscles, feeling SOB)
- History of symptoms associated with chief complaints
- Differentials
- Pulmonary embolism: similar (acute dyspnea) but does not respond to supplemental oxygen, has jugular venous distention, and has risk factors (eg. prolonged sitting). Get CTPA
- Pulmonary edema: Generalized lung opacity on chest X-ray
- Investigation
- Continuous pulse oximetry: Monitor oxygenation (Decreased oxygenation)
- ABGs: important in any patient with SOB (Respiratory acidosis with compensatory metabolic alkalosis, normal pH, low PCO2, high HCO3-)
- CXR: possibility of Pneumonia, features of COPD (Hyperinflation, flattened diaphragm, consolidations if bacterial pneumonia)
- EKG: the possibility of RHF (Right-axis deviation)
- BMP: routine (elevated HCO3-)
- CBC: signs of infection (elevated HCT due to poor oxygenation, elevated WBC if bacterial infection)
- Treatment
- ABCs:
- Supplemental oxygen (90-95%, 95% is associated with poorer outcomes) via NC or BiPAP
- Inhaled bronchodilators (albuterol +/- ipratropium)
- Systemic corticosteroids (Methylprednisone)
- Empiric antibiotics (Azithromycin PO OR ampicillin/sulbactam IV; plus others)
- Sputum Culture (+ sensitivity)
- Other labs as by presentation
- ABCs:
- When to admit a patient with COPD exacerbation
- Sudden worsening of dyspnea at rest
- Severe tachypnea (>30/min; will eventually tire out)
- Acute respiratory failure (Hypercapnia)
- Deteriorating oxygen saturation
- Confusion or drowsiness (signs of AMS)
- Cyanosis or signs of CHF
- Failure to respond to initial management
- Serious comorbidities
- Insufficient support at home (older pts etc.)
Interventions in COPD
| Agent | Dose | Comment |
|---|---|---|
| Ipratropium | 0.5mg NEB q6h | First Line |
| Albuterol | 2.5mg NEB q6h | First Line |
| Corticosteroids | Methylprednisone 125mg IV or Prednisone 60mg PO or Prednisone PO taper x 2wk | Exacerbation, Following admission |
| Oxygen | Titrate to SpO2 90-93% or PaO2 55-60 | Home and In patient |
| Intubation and Ventilation | Last Resort |

