Overview
Postpartum haemorrhage (PPH) is classically defined as blood loss of greater than 500 mL in vaginal delivery or 1000 mL at Caeserian. ACOG defines it as a 10% drop in hematocrit or need for transfusion. Most clinicians rely on clinical judgment to diagnose PPH since 500 mL is about average.
An estimated 5% of women lose > 1,000 mL in the first 24 hours.
Early PPH: “excessive” blood loss within 24 hours post-partum
Late PPH: “excessive” blood loss between 24 hours and 6 weeks post-partum
| Common cause | Dx | Tx | |
|---|---|---|---|
| Uterine atony | Precipitous labor, Overdistended uterus | Soft, boggy uterus | Tonics and massage |
| Lacerations | Uncontrolled labour | Visual inspection | Repair of tears, Tranexamic acid |
| Retained POC | Accessory lobe, Abnormal placentation | Sonography | Manual removal, Ultrasound-guided D&C |
| Coagulopathy | Abruptio placentae, HELLP Syndrome | Bleeding elsewhere, Labs | Blood products |
| Uterine inversion | Myometrial weakness | Visual inspection | Replacement under anaesthesia |
- Causes of PPH
- Tone – Uterine atony (MCC), Uterine inversion
- Trauma – Genital tract lacerations
- Tissue retention – Retained Products of Conception
- Thrombin – Coagulopathy
- Immediate Treatment
- Call for help and establish the cause
- Assess ABCs
- Supplemental Oxygen
- Insert bilateral wide-bore IV catheters and volume replacement with IV crystalloids
- Monitor vitals and catheterize for urine output
- Assess the need for blood transfusion
- Order labs: CBC, GXM, Coagulation panel
- Treatment of Intractable/unexplained postpartum bleeding
- Rule out lacerations
- Uterine massage and uterotonics
- Dilation and Curettage if lacerations have been repaired and there is no response to uterotonics and fundal massage
- Balloon tamponade if D&C fails
- Laparotomy if refractory to packing for:
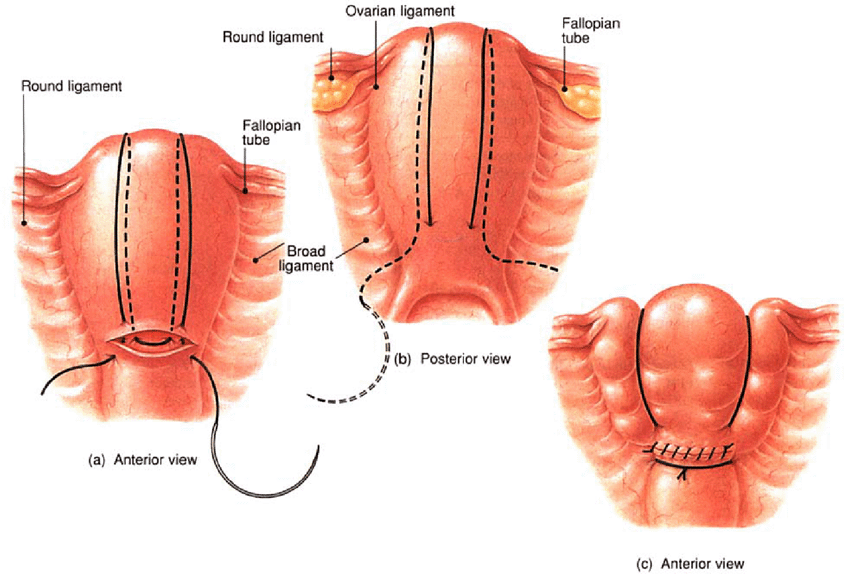
- Uterine compression sutures
- Uterine artery ligation
- Internal iliac artery ligation
- Subtotal Hysterectomy
- Complications of PPH
- Shock
- Sheehan syndrome: post-partum pituitary gland necrosis. Sx – failed resumption of regular periods, hypothyroidism, adrenal insufficiency
- Prevention of PPH
- Healthy practices prior to labour
- Prevention, early detection, and treatment of anemia
- The early detection and management of vaginal bleeding problems;
- Complication-readiness preparations.
- Active management of the third stage of labour (AMTSL)
- IM 10IU Oxytocin within 1 minute of delivering the child
- Controlled Cord Traction (CCT) and Counter-pressure to the uterus
- Uterine massage after delivery of the placenta.
- Preventing prolonged labor
- Preventing dehydration
- Early detection and management of vaginal bleeding problems
- Avoiding vaginal/perineal trauma
- Healthy practices prior to labour
Uterotonics
| Uterotonic | Dose | Route |
|---|---|---|
| Oxytocin | 20-40 IU | IV in 1L crystalloid |
| Ergometrin | 0.2 mg | IM or IV slowly |
| Misoprostol | 200-800ug | Sublingual or PR |
| Prostaglandin F2a | 0.25 mg | IM |

Uterine Atony
Uterine atony is a lack of proper uterine tone following delivery, resulting in insufficiently compressed vessels in the endometrium and myometrium, which then precipitates haemorrhage. Diagnosis is clinical.
- Causes of uterine atony
- Precipitous or Protracted labour
- Uterine overdistention (Multiple gestations, Macrosomia, Polyhydramnios)
- Grand multiparity
- Chorioamnionitis
- Medications (MgSO4, B-agonists, Halogenated anesthetics)
- Concealed placental abruption (Couvelaire uterus)
- Anaemia (uterine inertia)
- Signs and Symptoms
- The uterus is boggy/doughy, soft, enlarged, and palpable above the umbilicus.
- Treatment
- Uterotonics (Oxytocin, Ergometrine, Misoprostol, Carbetocin
- Fundal massage or compression
- Balloon tamponade
- B-lynch suture
- Ligation of the uterine/Iliac arteries
- Uterine artery embolization
- Peripartum subtotal hysterectomy
Genital Tract Lacerations
Lacerations may be d/t perineal tear, episiotomy, or laceration limited to the genital tract (e.g., uterus, cervix, vagina). You are always going to see some degree of lacerations. Experienced Obstetricians are usually able to detect and repair lacerations early. Uterine atony should always be ruled out even in the presence of lacerations.
- Causes
- Uncontrolled or difficult vaginal delivery
- Operative vaginal delivery.
- Signs and symptoms
- Bright-red blood in the presence of a well-contracted uterus
- Treatment
- Surgical repair
- Evacuation and repair of hematoma
- Tranexamic acid if bleeding continues
Retained Products of Conception
Retained POC is a common cause of both early and late PPH.
- Risk factors
- Accessory placental lobe
- Abnormal placentation (Previa, Accreta spectrum)
- Operative vaginal deliver
- Signs and symptoms
- Inspection of the placenta may reveal missing cotyledons (placental surface visible on the maternal side)
- Investigations
- Ultrasound
- Treatment
- Whole retained placenta
- Oxytocin
- Controlled Cord Traction (CCT)
- Intraumbilical vein injection (if there is no bleeding)
- The whole placenta still retained
- Manual removal with prophylactic antibiotics
- Pain medications
- Retained fragments
- Oxytocin
- Manual exploration to remove fragments
- Gental curettage or Aspiration or Ultrasound-guided D&C
- Whole retained placenta


Placenta with disrupted maternal surface

Placenta with succenturiate lobe
Coagulopathy
A rare cause of bleeding. We are particularly worried about DIC
- Causes
- Placental abruption (MCC of DIC)
- HELLP Syndrome
- Sepsis/septic shock
- Amniotic fluid embolism
- Dilutional coagulopathy
- Fetal death
- Signs and symptoms
- Bleeding elsewhere
- Well-contracted uterus
- Absence of lacerations
- Investigations
- CBC
- PT/PTT
- Ultrasound
- Treatment
- Admit to ICU
- Selective blood product replacement
Uterine Inversion
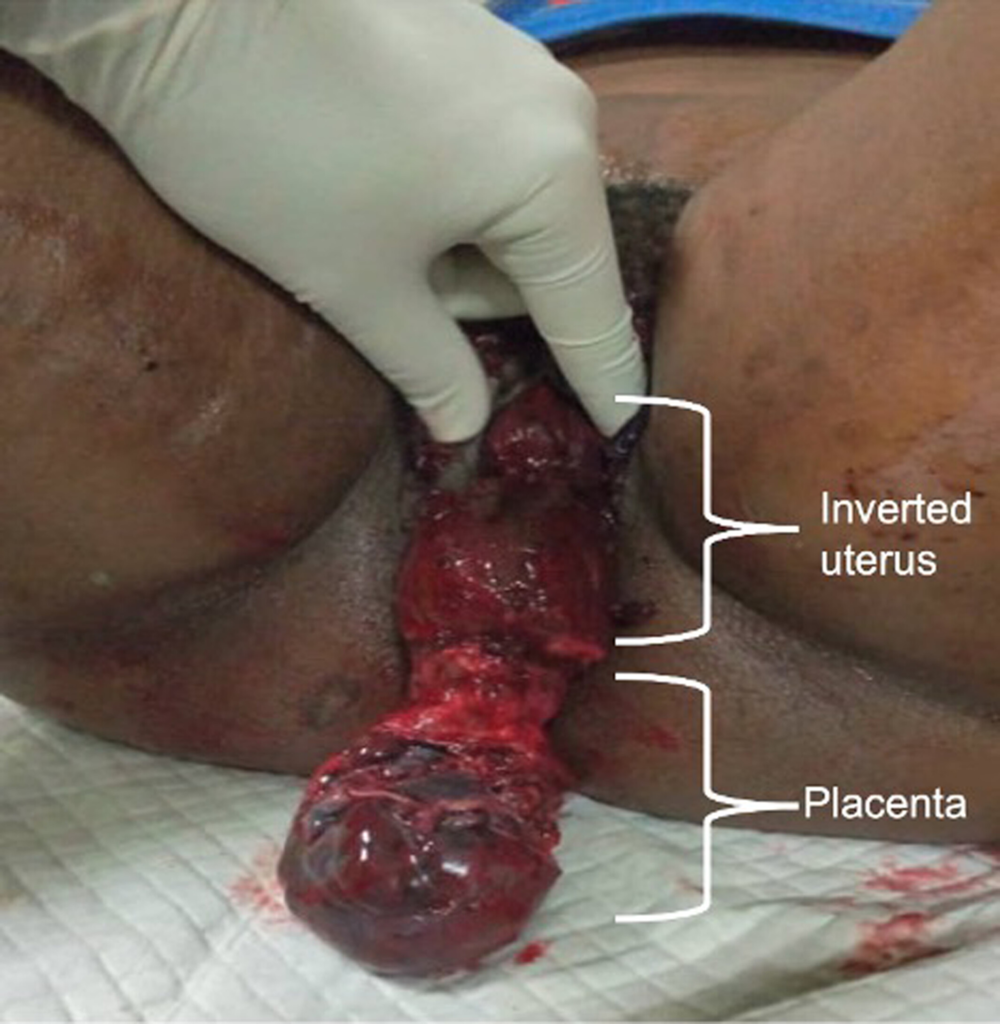
Uterine inversion is the inside-out collapse of the uterine fundus through the endometrial cavity, which may protrude through the cervix and into the vagina. A true obstetric EMERGENCY. Diagnosis is clinical
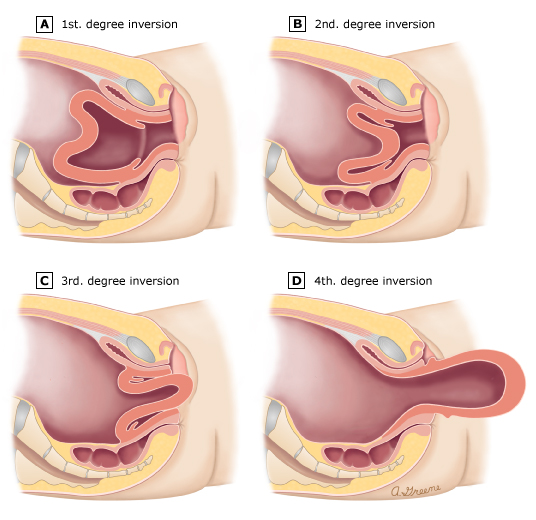
| Degree | Description |
|---|---|
| First-degree inversion | The fundus inverted up to the cervix |
| Second-degree inversion | The body protrudes through the cervix and into the vagina |
| Third-degree inversion | Inverted uterus prolapsed outside the vagina |
| Fourth-degree inversion | Prolapse of inverted uterus and vagina |
Degrees of uterine inversion
- Risk factors
- Uterine abnormalities
- Prolonged labor
- Previous uterine inversion
- Abnormal placentation (accreta)
- Fundal implantation
- Short umbilical cord
- Excessive traction
- Signs and symptoms
- Inability to palpate the endometrial cavity
- Beefy red, bleeding mass protruding into the vagina (occasionally)
- Treatment
- Manual replacement under anaesthesia
- Follow by oxytocin
