Obstetric Fistula
An obstetric fistula is an abnormal opening between the woman’s genital tract and the urinary tract or rectum. It is commonly a result of neglected or prolonged obstructed labor.
- Risk factors for obstetric fistulaThe 3 delays
- First delay: delayed decision to seek care
- Low socio-economic status
- Early marriage
- Illiteracy and lack of formal education
- Low social status
- Harmful traditional practices e.g. FGM
- Inadequate family planning +/- short inter-delivery interval
- Labor onset at home
- Second delay: delayed arrival at the health facility
- Poor road conditions
- Poor transportation
- Poor communication
- Insecurity
- Third delay: delayed access to adequate care
- Insufficient skilled staff
- Lack of emergency obstetric services (e.g. C-section)
- First delay: delayed decision to seek care
- Causes of obstetric fistula
- Prolonged and Obstructed labour (MCC)
- Instrumental delivery
- Caesarean Section (with or without hysterectomy)
- Defibulation in women who have had FGM
- Symphysiotomy
- Episiotomy
- Types of obstetric fistula
- Vesicovaginal
- Vesiouterine
- Vesicocervical
- Ureterouterine
- Ureterocervical
- Ureterovaginal
- Urethrovaginal
- Rectovaginal
The obstetric labour injury complex
| Fistula | Vesico-vaginal fistula, Urethrovaginal fistula, Recto-vaginal fistula, Ureteric fistula |
|---|---|
| Vaginal steonosis | Due to healing by fibrosis |
| Nerve damage | Foot drop and paraesthesia caused by compression of the lumbosacral plexus and peroneal nerve damage due to prolonged squatting |
| Dyspareunia | Due to vaginal scarring and stenosis |
| Damage to the cervix | Causing incompetence and stenosis which can lead to hematometra |
| Renal damage | Due to pyelonephritis and hydronephrosis caused by obstructing strictures and stones. Can ultimately lead to renal failure |
| Urine dermatitis | Urine phosphates and nitrates cause chronic excoriation of the vulva |
| Bladder stones | Women with obstetric fistula tend to reduce water intake or insert clothes in the vagina. these practices promote stone formation |
| Socio-economic consequences | Depression, divorce or separation, malnutrition, ostracization |
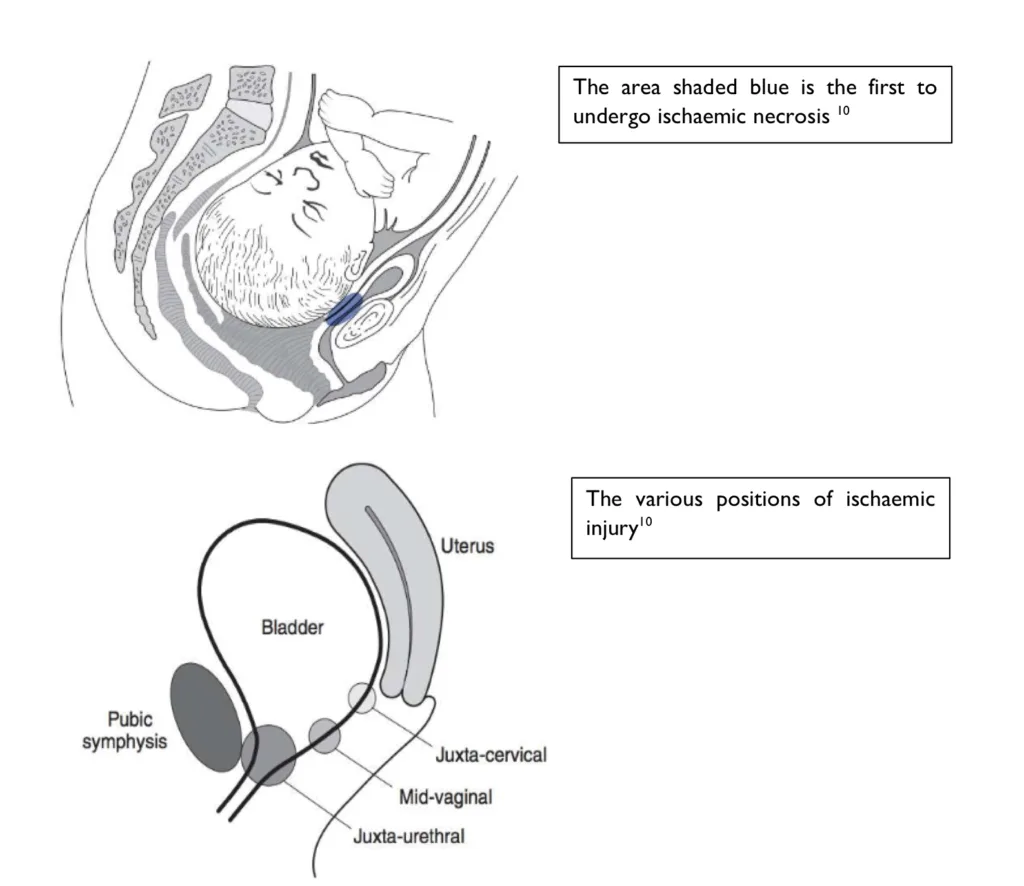
- Pathogenesis of obstetric fistula in obstructed labor
- During obstructed labour there is prolonged pressure exerted on the anterior vaginal wall and bladder neck by the foetal head and posterior pubic symphysis
- This causes ischemia and reduced venous outlfow ultimately causing pressure necrosis
- After delivery the necrotic tissue sloughs off leaving a direct communication between the genital tract (uterus, cervix, vagina) and the urinary tract (ureters, bladder, urethra), and/or the rectum.
- Ischemia can also involve other pelvic tissue resulting in a spectrum of injuries known as the obstetric labour injury complex
Waaldijik Classification of obstetric fistula
Type I: Fistulae ≥5 cm from the EUO and therefore not involving the closing mechanism. These have an excellent prognosis, because the all-important urethra and bladder neck are intact.
Type II: Fistulae that involve the closing mechanism (<5cm from the EUO):
A. Without (sub)total involvement of the urethra:
(a) without a circumferential defect
(b) with a circumferential defect
B. With (sub)total involvement of the urethra:
(a) without a circumferential defect
(b) with a circumferential defect.
Type III: Miscellaneous fistulae, e.g. uretero-vaginal and other exceptional fistulae.
NOTE:
- Circumferential defect – complete separation of the urethra from the bladder.
- Note there are other classification systems such as Goh’s system.
- Patient history
- History of female genital mutilation
- History stillbirth, cephalopelvic disproportion or obstructed labour
- Operative vaginal delivery – episiotomy, symphysiotomy or destructive surgery
- Caeserean section
- Signs and symptoms
- Urinary incontinence
- Constant leak
- Not dependent on activity
- Onset directly after labour and delivery
- Fecal incontinence
- Other problems with mobility and walking
- Urinary incontinence
- Physical exam
- Speculum exam
- Genital lacerations
- Urine draining through the anterior vaginal wall
- Site and number of fistula
- Speculum exam
- Investigations
- Double dye test: pack the vagina with sterile gauze and give dye intravesical via foley or Per Oral
- Instillation of methylene blue into the bladder: identifies vesicovaginal fistula
- Methyleneblue crosses from the bladder and into the vagina staining the gauze blue
- PO Phenazopydidine (Pyridium): identifies ureterovaginal fistula
- Pyridium crosses the uterus into the vagina staining the tampon orange
- Instillation of methylene blue into the bladder: identifies vesicovaginal fistula
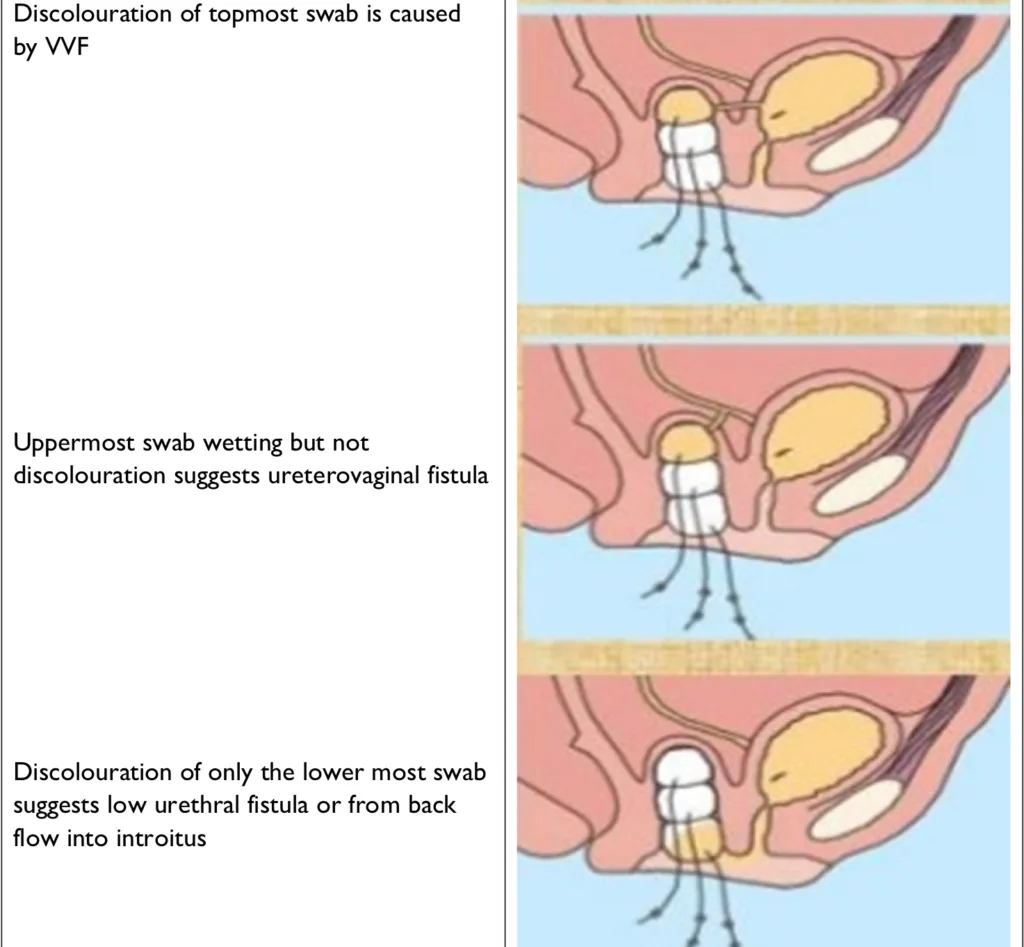
- 3 swab test: pack the vagina with 3 separate gauzes and fill the bladder with methylene blue die
- Ureterovaginal fistula: wetting of the uppermost swab
- Vulvovaginal fistula: discoloration of the uppermost swab (do you mean vesicovaginal)
- Urethrovaginal fistula: discoloration of the bottom-most swab
- CT KUBor IV pyelographyCystoscopyRetrograde pyelogram
- Retrograde pyelography is the most definitive test to diagnose a ureterovaginal fistula
- Urinalysis and culture: r/o concurrent UTI
- U/E/C: evaluate kidney function
- Double dye test: pack the vagina with sterile gauze and give dye intravesical via foley or Per Oral
- Treatment
- Surgical repair
- Prevention
- Educate communities on the cultural, social and physiological factors that increase the incidence of obstetric fistulas such a delaying child bearing and improving nutrition.
- Improve the social status of women by promoting education for young girls.
- Ensuring their is easy access to health facilities which are well equipped and staffed with professionals.