Cord Prolapse
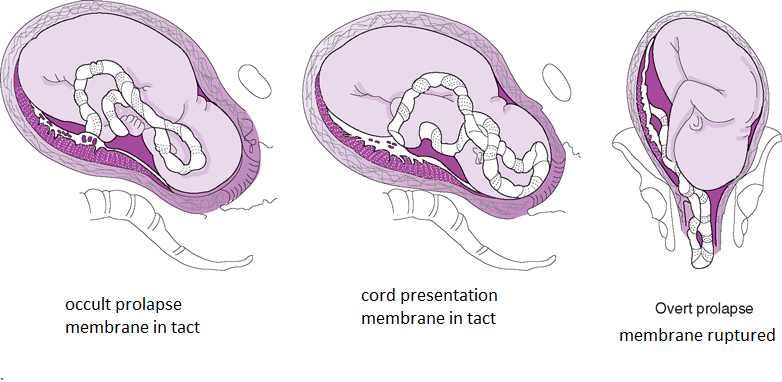
A prolapse umbilical cord is protrusion of the umbilical cord ahead of or alongside the presenting part of the fetus. Serious emergency if it is visible. Most common cause is ruptured membranes when the presenting part is not engaged. DO NOT touch the cord or try to return it into the uterus (will cause reflex vasospasm).
- Occult prolapse
- Cord prolapses alongside the head of the fetus (Can’t see, difficult to feel). Membranes are still intact
- Funic presentation
- Cord prolapses over the presenting part of the fetus i.e. the umbilical cord is the presenting part (different from vasa previa; a funic presentation is mobile). Membranes are still intact.
- Overt prolapse
- Visible cord prolapse (membranes usually ruptured)
- Risk factors
- Malpresentation
- Amniotomy (before presenting part engages)
- External cephalic version
- Fetal anomalies
- Cord abnormalitis
- Polyhydramnios (more room for the umbilical cord to move)
- Multiple gestation (more room, more cords)
- SROM
- PPROM
- Grand multiparity (≥ 5 P)
- Uterine anomaly
- Treatment
- Emergent C-section
- Put mom in knee-chest position and hold the fetal head in an elevated position
Shoulder dystocia
Shoulder dystocia is impaction of the anterior shoulder behind the maternal pubic symphisis.
- Risk factors
- Fetal macrosomia (big baby)
- Maternal diabetes (big baby)
- Post-term pregnancy (big baby)
- Maternal obesity
- Prolonged second stage (d/t shoulder dystocia)
- Operative vaginal delivery
- History of shoulder dystocia
- Turtle sign
- Baby’s head comes out with contractions and returns when contractions stop
- Treatment
- Suprabupic pressure + McRobert’s maneuver (causes cephalad rotation of the pubic head)
- Corkscrew maneuver (rotates the shoulder to a more diagonal/transvere position)
- Episiotomy
- Attempt to deliver posterior shoulder
- Break clavicle
- Emergent C-section
- Complications
- Erb’s palsy (waiter’s tip deformity; arm adducted and pronated)
- Fractures (e.g. clavicular)
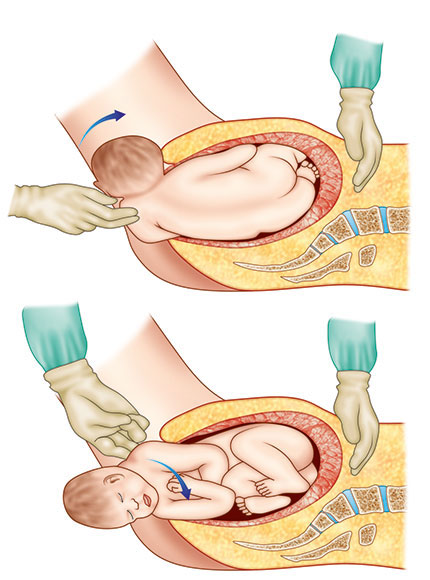
McRobert’s Maneuver
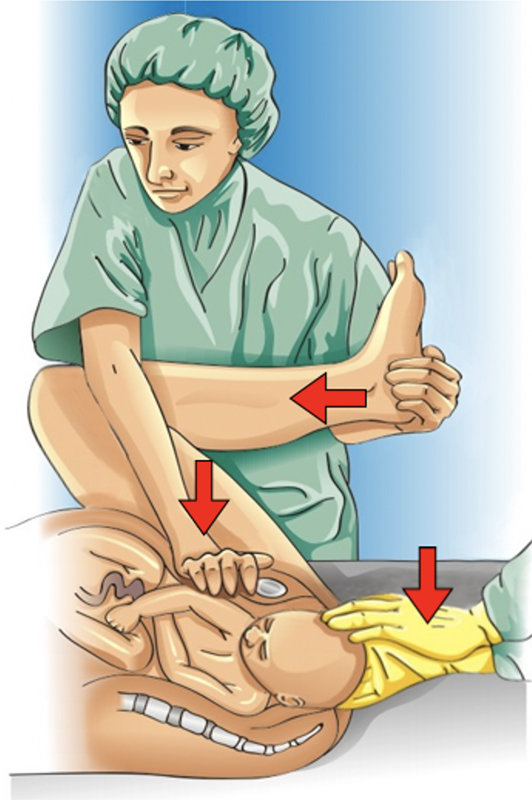
Cockscrew maneuver
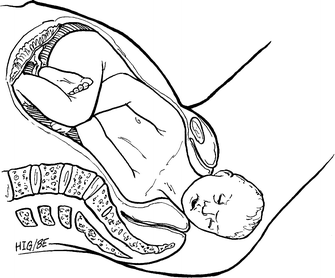
Uterine rupture
Uterine rupture is complete separation of the wall of the uterus. One of the chief causes of late pregnancy bleeding. Most commonly associated risk factor is scarring from a classical (vertical) Caesarean incision.
- Risk factors
- Uterine scarring (C-section, trauma, instrumentation – D&C, D&E, elective abortion)
- Hx of myomectomy
- Excessive uterine stimulation
- Uterine anomalies
- Hx of invasive molar pregnancy
- Hx placenta percreta/increta
- Malpresentation
- Fetal anomaly
- Cocaine abuse
- Signs and symptoms
- Tearing uterine pain
- “Popping sensation”
- Hemorrhage
- Cessation or abnormalities of contractions
- Loss of fetal station
- Fetal distress (most reliable sx)
- Treatment
- Emergent C-section w/repair or hysterectomy
Obstetrical laceration and Episiotomy
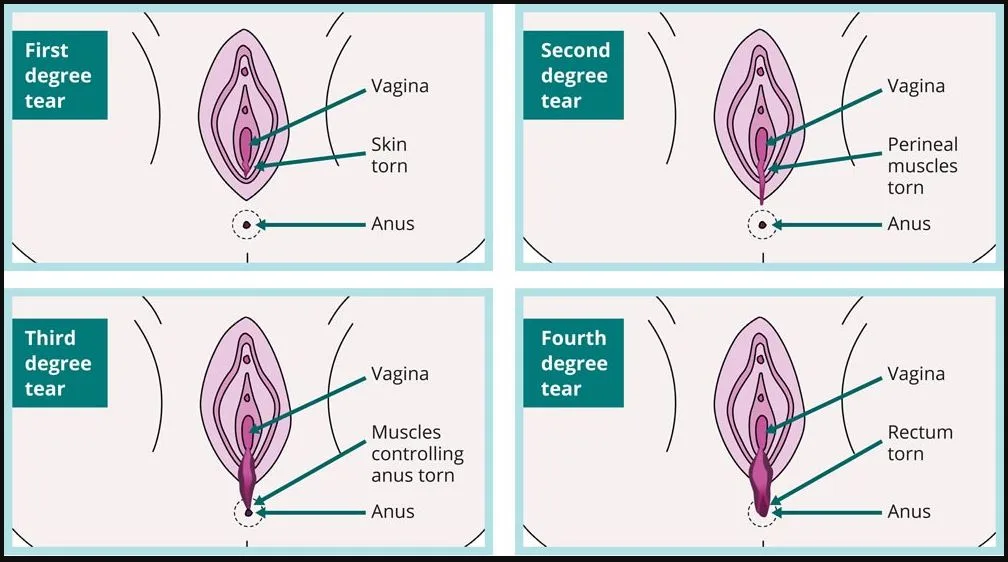
Obstetric lacerations are injuries to the perineum during vaginal delivery. Common, and occur spontaneously. Classified according to their extent.
Tab
| Tear | Extent |
|---|---|
| First degree | Perineal mucosa only |
| Second degree | Perineal body musculature but not extending to the rectal sphincter (most common) |
| Third degree | Extends to the rectal sphincter but not to the rectal mucosa |
| Fourth degree | Full tear extending to the rectal mucosa |
Perineal tears grading
- Treatment
- Repair in layers (via careful suturing under sterile conditions)
- Pain management
- NSAIDs
- Sitz baths
- Complications
- Rectovaginal fistula (if fourth-degree tear is not repaired adequately)
- Incontinence
- Dyspareunia
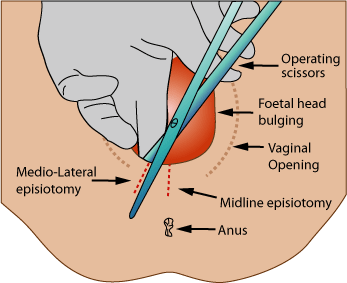
Episiotomy
An episiotomy is a surgical incision of the posterior vaginal wall and perineum to reduce the incidence of perineal tears. For breech presentation, episiotomy should only be cut once the anterior buttock has been delivered and the anus is visible at the fourchette. Medio-lateral episiotomy is usually preferred to midline episiotomy (which is too close to rectal sphincter = increased risk of 4th degree laceration; however it is less painful and bleeds less)
- Benefits of a midline episiotomy
- Muscles are not cut
- Less blood loss
- Easy repair
- Superior healing
- Rare dyspareunia
- Demerits of a midline episiotomy
- Extension may involve the rectum
- Benefits of a mediolateral episiotomy
- Safety from rectal involvement from extension
- The incision can be extended if needed
- Demerits of a mediolateral episiotomy
- More blood loss
- Dyspareunia
Episiotomy