Overview
Labor is a physiological sequence of regular painful uterine contractions that results in progressive effacement and dilation of the cervix andvoluntary bearing-down efforts leading to delivery (expulsion per vagina of the products of conception). Cervical dilation w/o uterine contraction = cervical insufficiency. Uterine contractions w/o cervical changes = false labour (Braxton Hick’s contractions; disappears with IM opioids)
- Objectives of intrapartum care
- Improve outcome of labor and delivery
- Prevent, predict, diagnose, and appropriately manage fetal hypoxia and acidosis
- Assist the mother to enjoy the experience of childbirth and avoid unnecessary delay, pain, or trauma and prevent dehydration and infection
- Treatment of the parturient
- Admit when the cervix is dilated to 3cm or there is ROM)
- Orders
- IV access
- Clear liquid diet (in case of emergency C/S)
- Notify anaesthesia (ready for a spinal block or emergency C/S)
- Continuous Feral Monitoring and Partograph(to check for fetal distress)
- Encourage Left lateral decubitus position (relieve pressure on the IVC)
- Begin pushing (bearing down, at full dilation in coordination w/contractions)
- Administer IV oxytocin (immediately after delivery to reduce the risk of uterine atony and haemorrhage)
- Monitor for at least two hours after delivery
Fetal Orientation
Fetal Lie
Fetal lie is the relation between the fetal and maternal vertical axis. Women with an unstable fetal lie (fluctuating at term) should be routinely admitted as there is a risk of cord prolapse when the membrane ruptures.
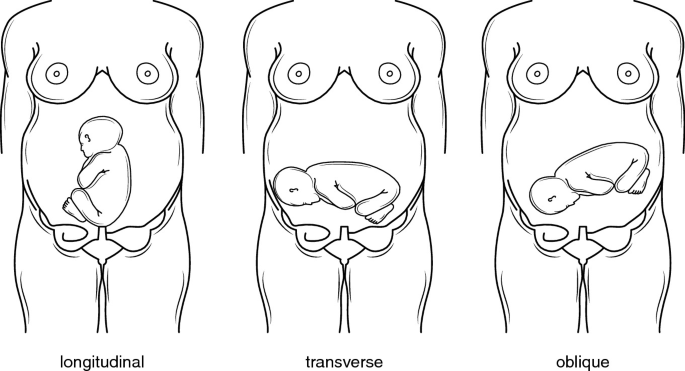
| Longitudinal lie | Fetal and maternal vertical axes are parallel |
|---|---|
| Transverse lie | The fetal and maternal vertical axes are perpendicular. Often presents with the shoulders |
| Oblique lie | Fetal and maternal vertical axes are diagonal |
Fetal presentation
Fetal presentation is the part of the fetus that is engaging at the pelvis. An external cephalic version can convert a breech to a cephalic presentation about half the time.
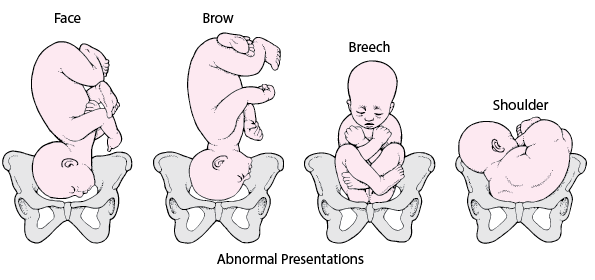
| Cephalic presentation | Head first. A hard, globular, independently ballotable mass in the presenting area. |
|---|---|
| Face presentation | Face presents first |
| Breech presentation | Buttocks/Sacrum with or without the legs present first. A broad, soft, irregular, non-ballotable bulky mass in the presenting area |
| Complete breech | Breech with the thighs and legs flexed |
| Frank breech | Breech with the thighs flexed and legs extended (feet in face) |
| Footling breech | Breech with the thighs and legs extended. Can be single or double footling. |
| Shoulder presentation | Shoulder presents first, commonly in transverse lie |
| Compound presentation | More than one presenting part e.g. shoulder + head |
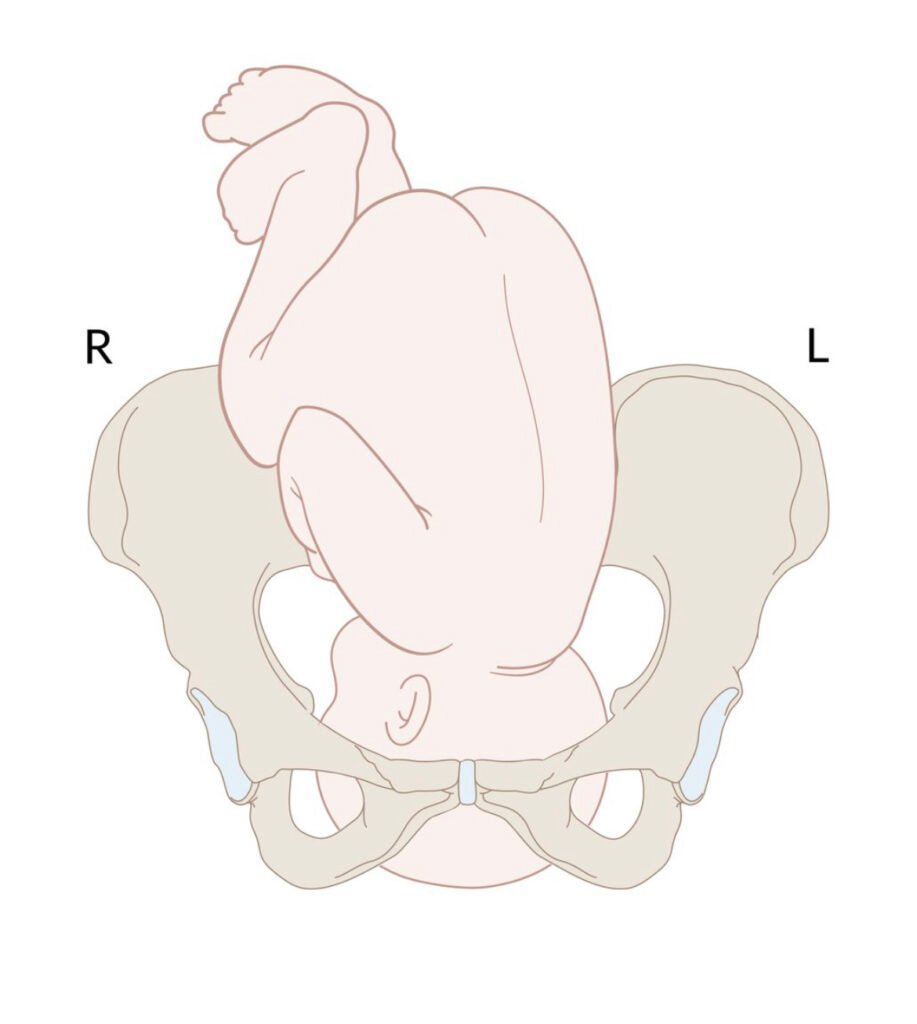
Fetal position
The fetal position is the position of the presenting part relative to the maternal pelvis. The presenting part may be occiput (cephalic), mentum (facial), or sacrum (breech). To determine the position, feel for the posterior fontanelle (three-sided, back of the head)
The convention goes (side) + (presenting part) + ant/post/trans
- Occiput anterior (OA)
- Occiput is directed anteriorly
- Left occiput anterior (LOA)
- Occiput is directed anteriorly, but slanted towards the maternal left
- Left occiput tranverse (LOT)
- The occiput is directed towards the maternal left
- Right occiput transverse (ROT)
- The occiput is directed towards the maternal right

Fetal attitude
This is the degree of flexion/extension of the fetal head in cephalic presentation
- Vertex attitude (ideal)
- Maximal flexion
- Military attitude (forehead attitude)
- Some flexion (anterior fontanelle presents first)
- Brow attitude
- Some extension
- Facial attitude
- Maximal extension
- Mentum anterior: chin faces the symphisis
- Mentum posterior: chin faces the coccyx
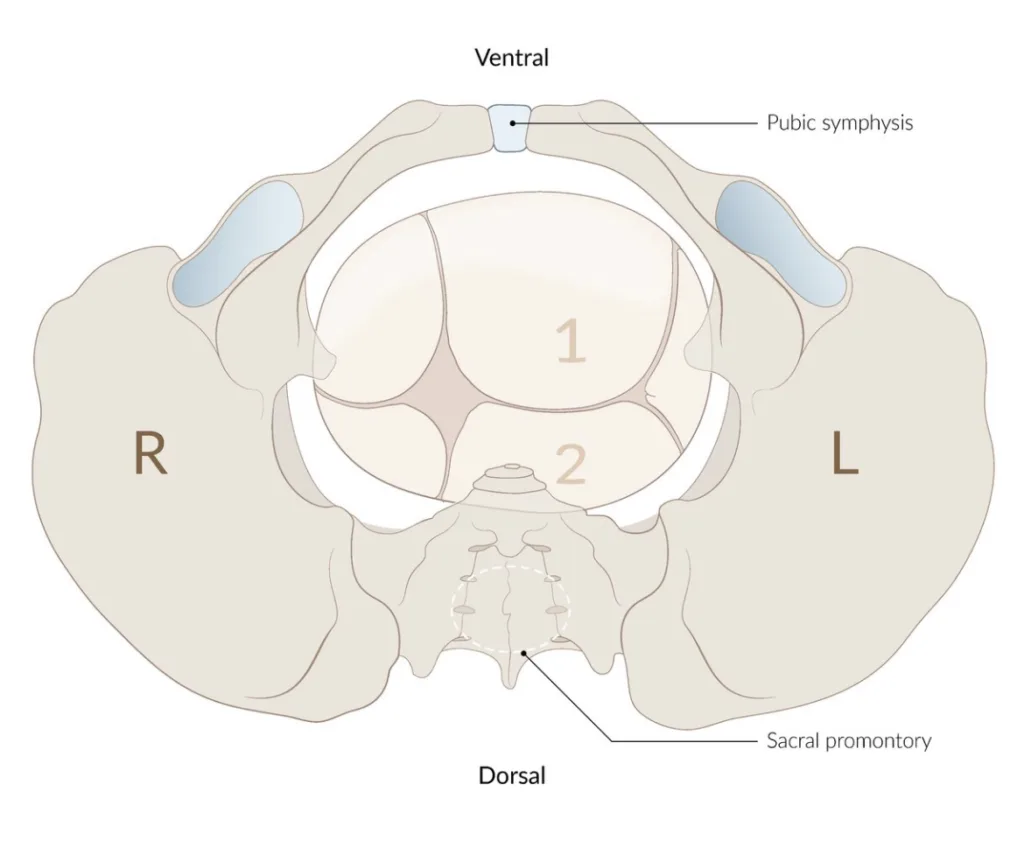
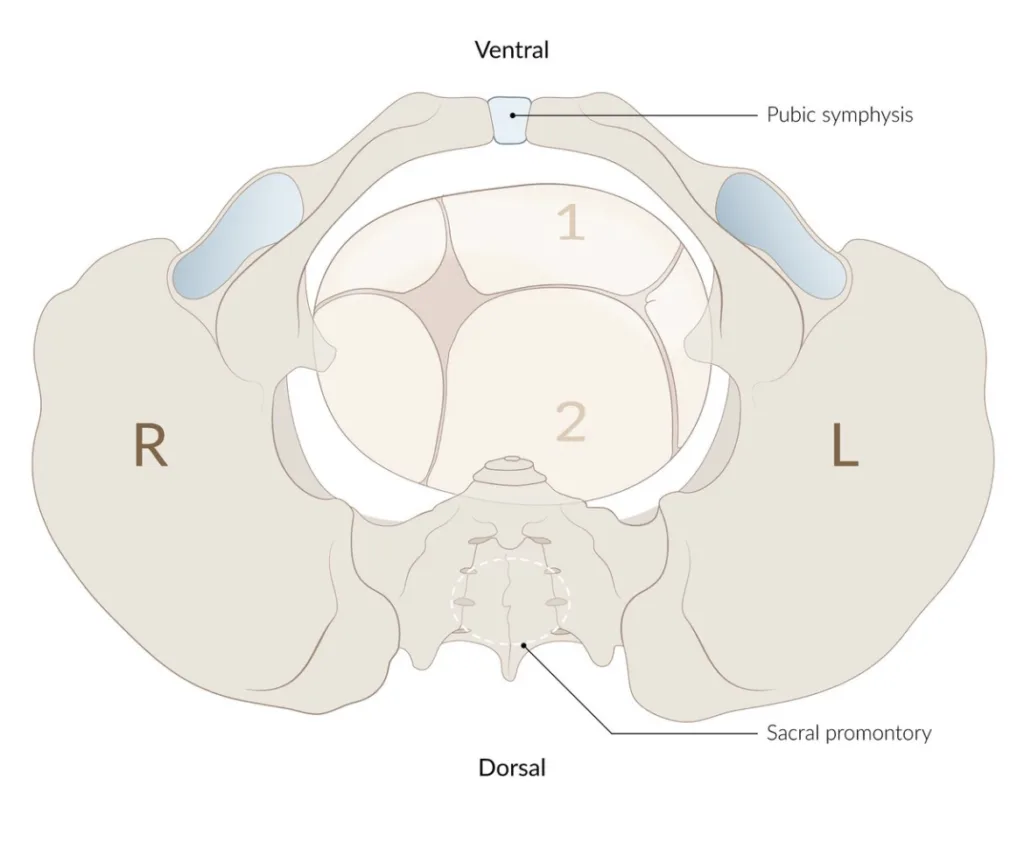
Synclitism
Synclitism is the relation between the pelvic inlet plane and the occipito-frontal plane (line from temple to temple).
- Normal Synclitism
- Parallel pelvic inlet plane and occipito-frontal plane
- Asynclitism
- The sagitta suture is in the transverse diameter of the pelvic inlet (not between the symphysis pubis and sacral promontory)
- Anterior asynclitism (Naegele obliquity)
- Sagittal suture tilts towards the sacral promontory. Anterior parietal bone presents first.
- Posterior asynclitism (Litzmann obliquity)
- Sagittal suture tilts towards the symphisis pubis. Posterior parietal bone presents first
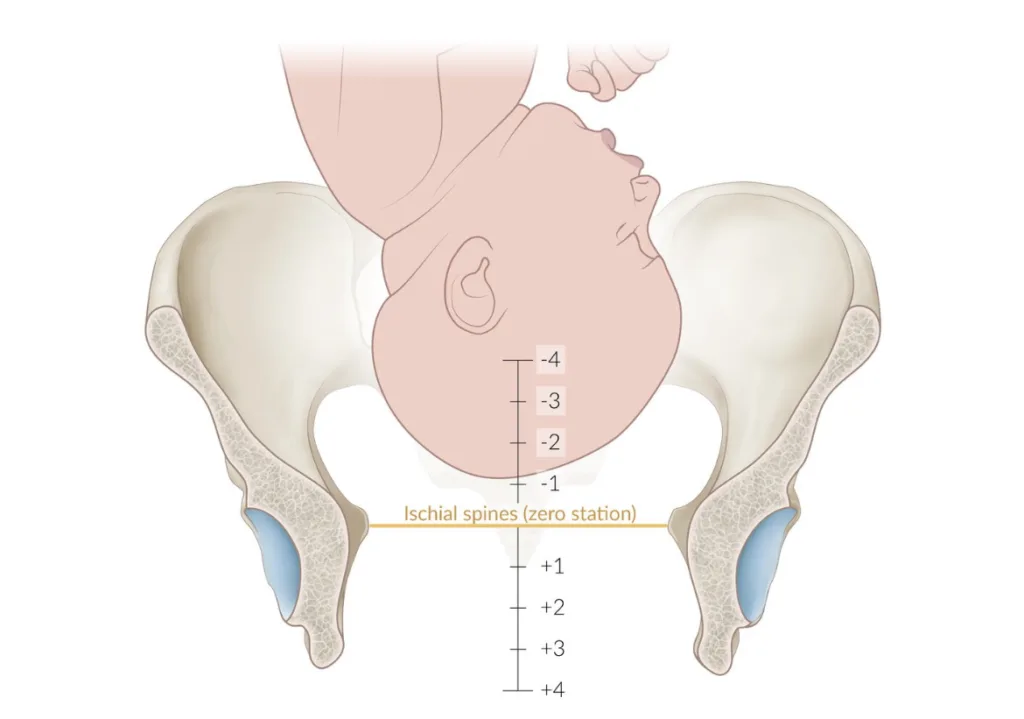
Fetal station
Fetal station is the descent of the fetal presenting part relative to the maternal ischial spine, expressed in cm above (minus) or below (plus).
Fetal station (AMBOSS)
Maternal changes
Cervical dilation
Cervical dilation is important in defining what stage of labor the mother is in. 10cm dilation is consistent with the beginning of the seconds stage of labor.
| Dilation | |
|---|---|
| 1 finger | 2cm |
| 2 finger | 3.5cm |
| 3 fingers | 5.5 cm |
| 4 fingers | 7.5 cm |
Cervical effacement
Effacement is essential for delivery. It is the shortening (thinning) of the cervix. Mediated by prostaglandins and oxytonin. Happens early on in labour (latent Phase I). Should be 100% by active labor, just below delivery. Cervica ripening agents can be used to move effacement along (e.g. Oxytocin, Misoprostol, Laminaria, Dinoprostone)
| 2cm | 0% effacement |
|---|---|
| 1cm | 50% effacement |
| Thin membrane | 100% effacement |
Stages of labor
Labor is regular contractions (every 5 mins lasting approximately 30 seconds), accompanied by cervical change
Braxton hicks contractions
Regular contractions without cervical change
| Primipara | Multipara | |
|---|---|---|
| Latent stage one | < 20 hours | < 14 hours |
| Active stage one | < 5-6 hours | <4-5 hours |
| Rate of cervical dilation | 1 – 1.2 cm/hr | 1/2 – 1.5 cm/hr |
| Stage two | < 2 hours | < 1 hour |
| Stage three | 30 min | 30 min |
***If mum has received spinal anaesthesia add 1 hour to stage 2 labor
Stage one
Closed to full dilation (10cm). Fetal assessment is done via Leopolds maneouver, fetal monitoring, and vaginal exam. Fetah HR is charted q30min on the partogram. Buscopan (Hyoscine) shortens the first stage of labor by accelerating cervical dilatation
Latent stage one: Closed to 4 cm dilated (very slow progress of dilation, effacement is going on)
Active stage one: 4 cm to full dilation (fully effaced, dilation accelerates). Fetal head is engaged and cardinal movements begin to occur
Tx Fetal monitoring
Fetal HR q30min charted on partogram
Transitory changes on cardiotocometry (Decelerations)
Early deceleration
Late deceleration
Variable deceleration
Tx Maternal monitoring
Pulse, Temp, and BP q1-2h
Uterine contractions q30min
Cervical dilation and station q4h
Meconium staining noted (Sx of fetal decompensation) – first, second, and third degree
Tx Sedation/Analgesia
IM Pethidine 100mg
IM Tramadoll 100mg
Antiemetics e/g/ IM Phenergan 25mg
Endonox (Nitrous oxide) inhalation
Epidural anesthesia (’Painless labor) – hypotension, vaccum deliveries, C/S
Stage two
Full dilation to delivery of the fetus.
Sensation of bearing down/gaping of the anal opening and vulva/distension of the perineum
Stage three
Delivery of the fetus to delivery of the placenta
Stage Four
Two hours following delivery.
Cardinal movements of delivery
These are important changes in the position and attitude of the fetus as it passess through the birth canal. The ischial spine narrows the transverse diameter as the fetus moves towards the mid-pelvis. We need the baby’s head to rotate from and OT position to OA position during descent. The cardinal movements allows this by making the maximal diameter of the fetal head (occipitofrontal diameter) correspond with the maximal diameter of the maternal pelvis.
| Engagement | Widest part of the presenting part has successfully passed through the pelvic inlet (OT). Clinically identified when ≤ 3/5 of the fetal head is palpable above the symphisis pubis |
|---|---|
| Descent | Fetal head descends in the pelvis (OT) |
| Flexion | Fetal head flexes to allow smalled diameter to present (OT) |
| Internal rotation | Fetal head rotates from a transverse position to a more AP position (OT → OA) |
| Extension | Fetal head exteds to facilitate delivery of the head |
| Restitution (External rotation) | The head immediately aligns with the fetal shoulders after delivery through the vulva (Body rotates such that the head is in a transverse position and the shoulders – biacromial diameter – are along the AP maternal axis, facilitating delivery of the shoulders. |
| Expulsion | Posterior shoulder is delivered. Fetal body is delivered. |
