Infectious disorders of Pregnancy
- Infections specific to pregnancy
- Chorioamnionitis
- Septic pelvic thrombophlebitis
- Episiotomy and lacerations
- Infections more common in pregnancy and puerperium
- Pyelonephritis
- Endomyometritis
- Mastitis
- Toxic shock syndrome
- Infections whose complications increase in pregnancy
- UTIs
- Bacterial vaginosis
- GBS
- Infections that affect the fetus
- Neonatal sepsis
- Viral (HSV, VZV, Parvo B19, CMV, Rubellla, HIV, Hep B, Hep C)
- Bacterial (Gonorrhea, chlamydia, syphilis)
- Toxoplasmosis
Group B Strep
Group B strep aka Streptococcus agalactiae is a gram positive commensal bug of the GIT and GUT tract in up to 30% of asymptomatic adults (hence the need for universal screening). Commonly responsible for UTIs, Chorioamnionitis, and Endometritis during pregnancy. A major cause of neonatal sepsis! Women should be screened via recto-vaginal culture at 35-37 weeks gestation for GBS. GBS prophylaxis (Penicillin) is given IV during labor.
50% of exposed infants will be colonized. 1 in 500 (0.2%) will develop symptoms. Mortality rate if symptomatic from vertical infection (early-onset group B sepsis) is 50%.
- Indications for GBS prophylaxis
- Previous infant with GBS infection
- GBS bacteriuria with this pregnancy
- Preterm delivery (< 37 weeks gestation)
- Membrane rupture ≥ 18 hours
- Intrapartum temperature ≥ 38 C (100.4 F)
- When should you give penicillin in PROM
- Ideally if membrane rupture ≥ 18 hours. Err on the side of giving Penicillin to a GBS-unknown PROM pt uness delivery is imminent and ROM < 18 hours
- Which antibiotics given during PPROM are sufficient to cover GBS
- Antibiotic including Ampicillin
- Complications of GBS
- Early onset neonatal GBS infection: fulminant PNA and sepsis d/t vertical infection, manifesting within 7 days of delivery. Mortality of 50%. Risk factors include prematurity, previous baby affected, positive urine cx
- Late onset neonatal GBS infection: meningitis, cellulitis or PNA manifesting after 7 days of life. May be acquired from the environment. Less common. Mortality of 25%
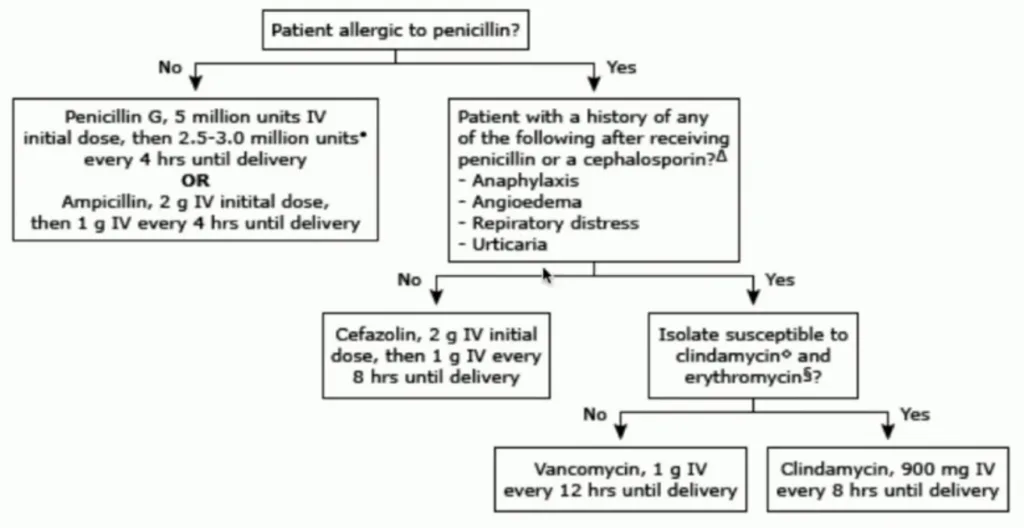
Intrapartum prophylaxis algorithm for mothers with positive screen or unknown GBS status
UTI in pregnancy
UTI is caused by an ascending infection of the urinary tract from existing flora. It is defined as the presence of ≥ 100,000 organisms/mL of urine if asymptomatic or > 100 organisms/ml of urine with pyuria (> 7WBC/mL) in symptomatic. MCC is Escherichia coli. Others include Klebsiella, Proteus etc. Risk of UTI increases in pregnancy mainly d/t urinary stasis (elevated progesterone relaxing detrusors, gravid uterus makes it difficult to void) and glycosuria. UTI is associated with adverse fetal risk and the biggest risk for development of symptomatic UTI is asymptomatic bacteriuria (20-30x increased risk; hence screened during first ANC visit and third trimester visit).
| Asymptomatic bacteriuria | Acute cystitis | Pyelonephritis | |
|---|---|---|---|
| Urine culture | Positive | Positive | Positive |
| Urgency, frequency, burning | No | Yes | Yes |
| Fever | No | No | Yes |
| CVA tenderness | No | No | Yes |
- Primary prevention of UTI in pregnancy
- Avoid bathing. Shower instead
- Wash hands before using toilet
- Wipe front to back
- Use liquid soap (less likely to have bacteria growing on it)
- Clean urethral meatus area first
Urinary tract change in pregnancy
- Renal pelvis and ureters
- Progesterone reduces ureteral tone, peristalsis and contraction pressure→ vesicoureteral reflux
- Gravid uterus applies pressure on the bladder and compresses the ureters
- Compression of ureters by enlarged vessels in the suspensory ligaments o the ovary
- Relative immunosuppression
- Right ureter is more affected than the left because it is affected by dextrorotation of the uterus by the sigmoid colon, as well as kinking as it crosses the right iliac artery
- Bladder
- edematous and hyperemic mucosa
- progesterone induces bladder wall relaxation and increases the capacity
- enlarged uterus displaces the bladder superiorly, anteriorly and flattens it, which can decrease capacity
- increased incidence of microhematuria
- Intermittent vesicoureteral reflux
- Due to incompetence of the vesicoureteral valve from bladder flaccidity
- increased intravesical pressure
- decreased intraureteral pressure
- Postpartum changes from trauma during labor and delivery
- mucosa congestion and submucosa haemorrhage
- decreased bladder sensitivity/ sensation
- detrusor atony
- postvoidal residual volume
- bladder overdistension
- urinary retention
- Impaired tubular function
- reduced fractional reabsorption of glucose, amino acids, and beta microglobulin
Asymptomatic bacteriuria
All women are screened for bacteriuria at their first ANC visit.
Approximately 10% of women have positive culture. 30-50% with ASB will develop symptomatic UTI (Pyelonephritis) if not treated.
- Risk factors
- Lower SES
- Diabetes
- History of UTI
- Multiparity
- Anatomic or functional urinary tract anomalies
- Sickle cell trait
- Symptoms
- None…
- Physical exam
- Unremarkable
- Investigation
- Urinalysis and culture
- Grows E. coli
- Urinalysis and culture
- Treatment
- Nitrofurantoin 100mg BD 7-10 days.
- Repeat culture after Tx and q1mos thereafter
- Daily suppression Tx if persists after two courses (Nitrofurantoin or Cephalexin
Acute cystitis
- Symptoms
- Burning urination
- Sensation of incomplete voiding
- Urinary urgency
- Frequency
- Suprapubic discomfort
- Physical exam
- Tenderness on pelvic exam with manipulation of bladder
- Investigation
- UA and culture
- Positive nitrites
- Positive esterase
- Increased WBCs, RBCs
- Proteinuria
- +/- bacteria
- Positive culture
- UA and culture
- Treatment
- Nitrofurantoin 100mg BD 7-10 days
- Repeat culture after Tx
- Daily suppression Tx for women with two or more UTIs and for women with increased risk of UTI (Diabetes, sickle cell trait)
Pyelonephritis
Women with pyelonephritis look sick (systemic infection)
- Symptoms
- Malaise
- Fatigue
- Chills
- Anorexia
- Sx of acute cystitis along with systemic sx
- Physical exam
- CVA tenderness
- Flank tenderness
- Sick-looking
- Investigations
- UA and culture
- Blood culture
- CBC
- BMP
- Treatment
- Admit
- IV antibiotics
- 2nd or 3rd generation cephalosporin (Ceftriaxone) or Ampicillin/Gentamicin
- Transition to PO after afebrile for 24-48 hours (try not to give antipyretics to monitor fever)
- Suppression therapy for remainder of pregnancy
- Control nausea (if woman is deH20 will put fetus at risk)
- Doxylamine/B12 or others
- Judicious use of IV fluids (inflammatory response puts at risk of ARDS
- Complications of pyelonephritis
- SIRS
- ARDS: pulmonary edema, injury
- Renal dysfunction
- Septic shock → hypoxic fetal events
- Spontaneous abortion
- Preterm delivery
- IUGR/LBW infant
Bacterial vaginosis in pregnancy
Bacterial vaginosis is the most common lower genital tract infection in women of reproductive age. Exact mechanism is unknown but likely due to disturbance of the vaginal flora.
- Obstetric complications of bacterial vaginosis
- Preterm labour
- Preterm delivery
- Preterm prelabor rupture of membranes
- Miscarriage
- Chorioamnionitis
- Endometritis
- Wound and surgical infections
- Subclinical pelvic inflammatory disease
- Risk factors
- Vaginal douching
- Oral sex
- Sex during menses
- New or multiple sex partners
- Early sexual debut
- Sexual activity with other women
- IUD placement
- Smoking
- Signs and symptoms
- “Fishy” grey vaginal discharge without vaginal discomfort
- Physical exam
- Unremarkable
- Adherent gray discharge
- Investigations
- Saline prep: “Clue cells”
- Positive amine “whiff”” test (after adding KOH to the discharge sample)
- Elevated vaginal pH
- Treatment
- Metronidazole
- Alternatively may use Clindamycin
Endometritis
Endometritis is an ascending polymicrobial infection of the uterine lining, which may invade the underlying wall(endomyometritis). Most common cause of postpartum fever. More common after C-section. Can occur after vaginal delivery esp. after manual delivery of the placenta. Common sites of infection are the implantation site or incision site. Should do a good physical exam to r/o other causes of post-partum fever.
Early postpartum endometritis: < 48 hours, usually after C-section
Late postpartum endometritis: 48 hours to 6 weeks, usually after vaginal
- Risk factors for endometritis
- C-section
- Prolonged labor (higher risk for endometritis and chorioamnionitis; more cervical exams done)
- Number of cervical exams
- HIV+
- GBS+ (MCC of endometritis manifesting in the first 24 hours)
- Adolescent
- Chlamydia infection(CC of late onset endometritis)
- Signs and symptoms
- Fever
- Tachycardia
- Foul smelling lochia
- Pelvic tenderness (Exquisite uterine tenderness that has gotten worse)
- Investigations
- Pelvic sonography: look for retained POCs
- CBC: elevated WBC w/left shift
- U/E/Cs: hyponatremia in sepsis
- UA + culture: r/o UTI
- Blood culture: variable
- CXR: unremarkable
- Treatment
- Admit
- Clindamycin + Gentamicin.
- May transition to PO Doxycycline 100mg BD after afebrile for 24-48 hours for 11-14 days (advice not to breastfeed)
- US-guided D&C to remove RPOCs
- Monitor WBC for normalization
- Complications of endometritis
- Sepsis
- Peritonitis
- Pelvic abscess
- Hematoma
- Septic pelvic thrombophlebitis

Retained Products of Conception on Ultrasound
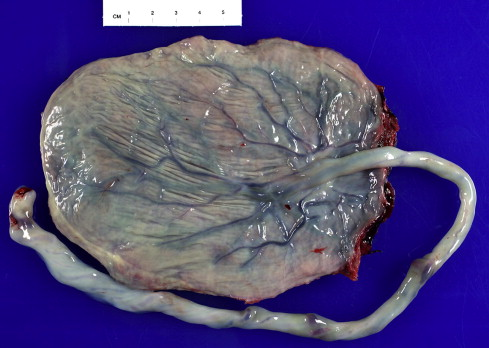
Chorioamnionitis
A common cause of maternal fever, and big complication of premature and prolonged ROM. Chorioamnionitis is an ascending bacterial infection of the membranes surrounding the fetus, which can extend into the amniotic fluid. The infection is typically polymicrobial (GBS used to be the most common isolate. Currently GNs are more common isolates since they aren’t covered by penicillin) and can affect intact or ruptured membranes. Dx is clinical (risk factors + Fever + two other sx). The goal of treatment is to reduce maternal and fetal complications (esp. NNS), by balancing
- Risk factors for chorioamnionitis
- Prolonged ROM
- Prolonged labor
- PPROM and prematurity
- Multiple digital exams with membrane rupture (use sterile gloves, not worth it to do more than an hour)
- GBS+
- Epidural anesthesia (controversial…)
- Cervical insufficiency (less space between vagina and membranes)
- EtOH and tobacco use
- Nulliparity
- What are the major concerns for the neonate when there is chorioamnionitis
- Cerebral palsy (d/t decompensation of brain tissue)
- Early-onset neonatal sepsis (EOS, within the first few days to weeks)
- Sx
- Maternal fever (> 38 C)
- Significant maternal tachycardia (HR > 120)
- **Fetal tachycardia (**FHR 160-180)
- Uterine tenderness
- Purulent/foul smelling amniotic fluid discharge
- Maternal leukocytosis
- Differentials
- Epidural-associated fever
- DDx for fever/abdominal pain
- UTI
- Appendicitis
- Influenza
- Pneumonia
- Investigations
- Amniocentesis: Traditionally the gold standard, to analyze and culture the amniotic fluid (takes 3 days). Profile similar to CSF analysis in Bacterial meningitis.
- Glucose: Low
- WBC: high
- Protein: high
- Gram stain: positive
- Esterase: positive
- IL-6: positive
- Culture: positive
- Amniocentesis: Traditionally the gold standard, to analyze and culture the amniotic fluid (takes 3 days). Profile similar to CSF analysis in Bacterial meningitis.
- Tx
- Fetal monitoring
- Expedite delivery
- Intrapartum IV antibiotics until delivery
- Ampicillin and Gentamicin (can be given in late late pregnancy when benefits outweight the risk)
- Add Clindamycin if performing C-section
- Antipyretics (reduces fetal HR and distress, reduces risk of encephalitis)
- Acetaminophen
- Notify pediatrics
- Maternal complications of chorioamnionitis
- Increased risk of C-section
- Endometritis
- Wound infection
- Pelvic abscess
- Bacteremia
- Postpartum hemorrhage
- Fetal complications of chorioamnionitis
- Fetal Inflammatory response syndrome
- Chronic lung disease
- Multi-organ damage
- Brain damage
- Preterm birth
- Perinatal death
- Neonatal infection and sepsis
- Respiratory distress due to pneumonia
- Cerebral palsy
- Intraventricular hemorrhage
- Necrotizing enterocolitis
- Fetal Inflammatory response syndrome