Overview
Antepartum hemorrhage is bleeding from late 2nd trimester to delivery (around 20-24 weeks and beyond). All causes of antepartum hemorrhage risk the complications of preterm delivery and fetal death.
Causes of Antepartum hemorrhage
| Cause | Bleeding | Blood | Diagnosis | Complications |
|---|---|---|---|---|
| Abruptio placentae | Painful | Maternal | U/S, FHT | DIC, maternal shock/death |
| Uterine rupture | Painful | Maternal | Loss of station, abnormal UCs, FHT | Hysterectomy |
| Placenta previa | Painless | Maternal | Sono, FHT | Malpresentation |
| Vasa previa | Painless | Fetal | Sono w/doppler, bright red blood, FHT | High risk fetal death |
| Abnormal placentation | Painless | Maternal | Sono | Hysterectomy, maternal shock/death |
| Risk factor | Predisposes to |
|---|---|
| Hypertension, trauma | Abruptio placentae |
| Uterine scarring | Abnormal placentation |
| Multiple gestation, ART | Placenta previa |
| Classical incision, overstimulation | Uterine rupture |
| Multiple gestation, succenturiate lobe, villametous cord | Vasa previa |
- Differentials for late pregnancy bleeding
- Cervical
- Cervicitis
- Cervical polyps
- Cervical cancer
- Vagina
- Lacerations (becomes more sensitive during pregnancy)
- Uterus
- Uterine rupture
- Placenta
- Abruptio placentae
- Placenta previa
- Vasa previa
- Others
- Hemorrhoids
- Cervical
- Investigations
- Obstetrics ultrasound
- CBC w/peripheral smear (to r/o DIC)
- PT/PTT
- D-dimer
- Fibrinogen
- Group and crossmatch (might need blood transfusion)
- Kleihauer-Betke to estimate RhoGAM dosage (if Rh negative)
- Apt test: to differentiate between fetal and maternal blood
- Fetal blood → pink
- Maternal blood → yellow-brown
- Immediate Treatment
- ABCs
- Insert 16-gauge IV catheter, start NS drip
- Foley catheter
- Speculum exam (to rule out differentials)
- Check fetal heart tones (with external Doppler)
- If in labor
- Tocolytics (extends labor)
- Betamethasone (to mature fetal lungs) and Magnesium Sulphate for neuroprotection
- ABCs
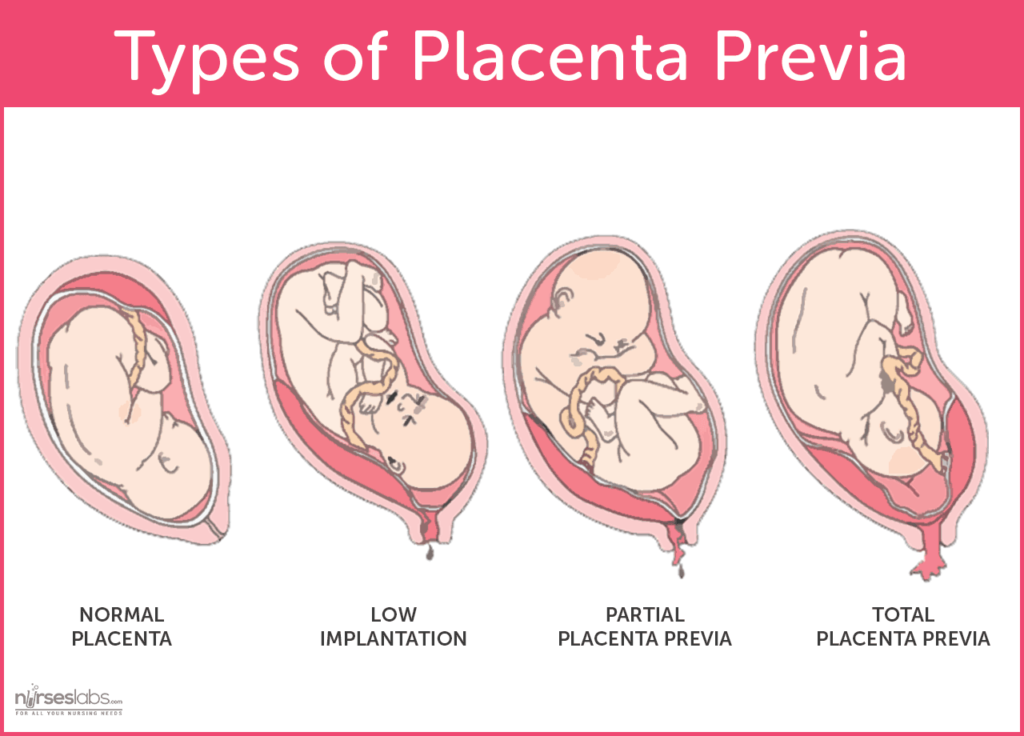
Placenta previa
Placenta previa is a common condition in which the placenta lies in the lower segment of the uterus. The placenta may avulse from the uterine wall as the lower segment begins to stretch at 28 weeks, classically resulting in painless bleeding PV. Diagnosis is through sonography. A vaginal exam SHOULD NOT be done with a suspected low-lying placenta as it can precipitate life-threatening hemorrhage!
Types of placenta previa
| Type | Description | |
|---|---|---|
| I | “Low implantation” | Lower margin dips into the lower segment of the uterus. It is within reach of the examining finger |
| IIA | “Marginal anterior” | Placenta is within 2cm of internal os when closed but does not cover it |
| IIB | “Marginal posterior” | Placenta is within 2cm of internal os when closed but does not cover it |
| III | “Partial” | Placenta covers the internal os when closed but not when fully dilated |
| IV | “Complete” | Placenta covers the os even when the cervix is fully dilated |
- Risk factors
- Previous placenta previa
- Multiple gestation
- Assisted Reproductive Technology (ART)
- Previous uterine surgery, insult, or injury e.g Caesarean delivery
- Previous or recurrent abortion
- Signs and symptoms
- Painless uterine bleeding
- Treatment if preterm (< 37 weeks) and stable
- Admit and observe
- Deliver at 36 weeks
- Treatment at term (≥ 37 weeks) and marginal os > 2cm (low-lying)
- Vaginal delivery
- Treatment at term (≥ 37 weeks) and stable and marginal os < 2cm (Type II, III, IV)
- Elective C-section
- Treatment if there is maternal or fetal jeopardy
- Emergent C-section
- Complications of placenta previa
- Preterm delivery
- Preterm Prelabor Rupture of Membranes
- Intrauterine Growth Restriction
- Malpresentation (commonly a transverse lie due to concurrent congenital uterine anomalies)
- Vasa previa
- Congenital anomalies
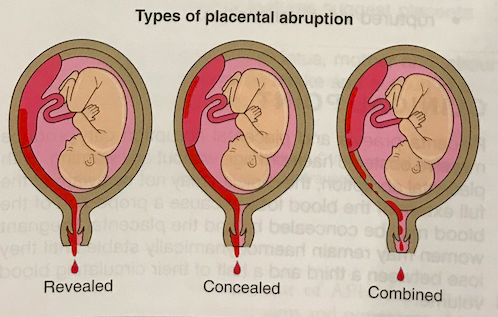
Abruptio placentae
Abruptio placentae is premature separation of the placenta from the uterus. Abruption is uncommon, and is not easy to treat. Abruption is difficult to pick up sonographically, but ultrasound is still done to rule out vasa previa.
- Risk factors
- Hypertension
- Blunt force trauma (avulses the placenta)
- Cocaine use (vasoconstriction)
- Previous abruption
- Signs and symptoms
- Painful late pregnancy bleeding
- Firm “woody-hard” and tender uterus
- Pain between contractions
- Fetal heart tone: bradycardia, late decelerations
- Principles of Treatment
- Replace blood loss
- Deliver without delay (preferrably vaginal)
- Prevent PPH, DIC, and renal failure
- Treatment is preterm (<37 weeks) and stable
- Admit and observe
- Treatment if term (≥ 37 weeks) and stable
- Vaginal delivery
- Treatment if there is severe abruption
- Emergent Caesarean delivery
- Indications for Caesarean delivery in abruption
- Previous scar
- Failure to progress despite AROM, Oxytocin and traction
- Bleeding to death with normal clotting factors
- Live foetus >2kg with signs of distress
- Transverse lie (vaginal delivery is impossible!)
- Complications of abruptio placentae
- Disseminated Intravascular coagulation
- CBC w/peripheral smear: Thrombocytopenia, schistocytes and helmet cells
- PT and PTT: prolonged
- D-dimer: High
- Fibrinogen: low or normal
- Preterm delivery
- Maternal and/or fetal shock
- Maternal renal failure
- Death
- Maternal (0.5-5%)
- Fetal (35-80%)
- Disseminated Intravascular coagulation
Types of abruptio placentae
Uterine rupture
Uterine rupture is complete separation of the wall of the uterus. It is more commonly associated with uterine scarring from a classical caesarean incision.
- Risk factors
- Uterine scarring
- Caesarean incision
- Trauma
- Instrumentation
- Elective abortion
- History of myomectomy
- Excessive uterine stimulation
- Uterine anomalies
- History of invasive molar pregnancy
- History placenta percreta/increta
- Malpresentation
- Fetal anomaly
- Cocaine abuse
- Uterine scarring
- Signs and symptoms
- Tearing uterine pain
- “Popping sensation” (relieving pressure within the uterus)
- Painful late pregnancy bleeding
- Cessation or abnormalities of contractions
- Loss of fetal station
- Fetal distress (late deceleration – most reliable sign)
- Treatment
- Emergent Caesarean delivery with repair or hysterectomy
Vasa previa
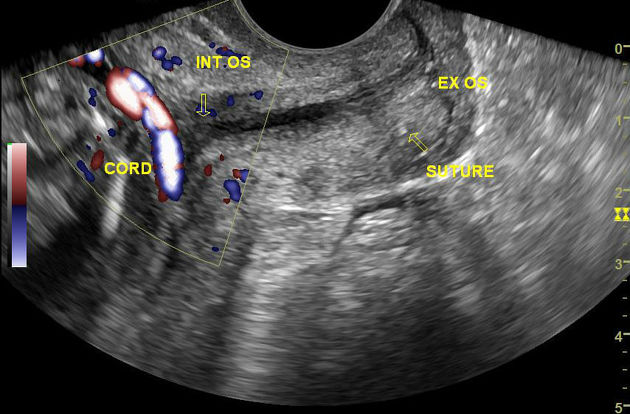
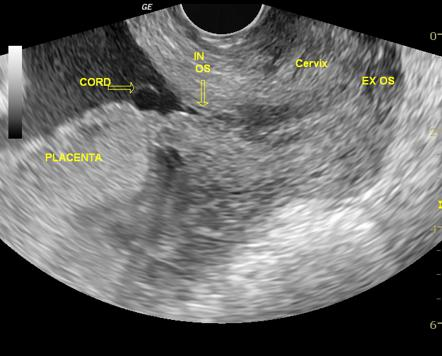
Vasa previa is a very rare condition where the fetal placental vessels cross the internal cervical os. It can be easily diagnosed via ultrasound with a color doppler.
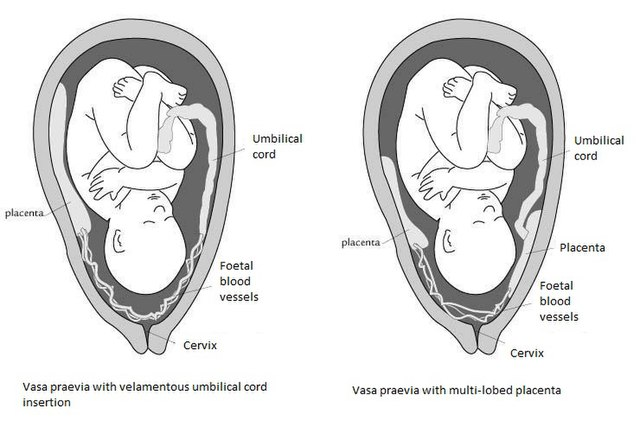
- Risk factors
- Velamentous cord
- Accessory (succenturiate) placental lobe
- Multiple gestation
- Signs and symptoms
- Bright red painless bleeding following Artificial ROM
- Fetal bradycardia
- Treatment
- Emergent Caesarean delivery
- Complication of vasa previa
- Fetal death due to exsanguination

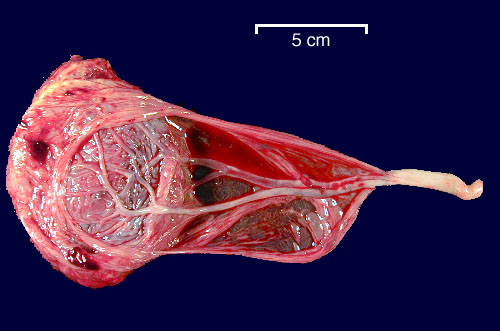
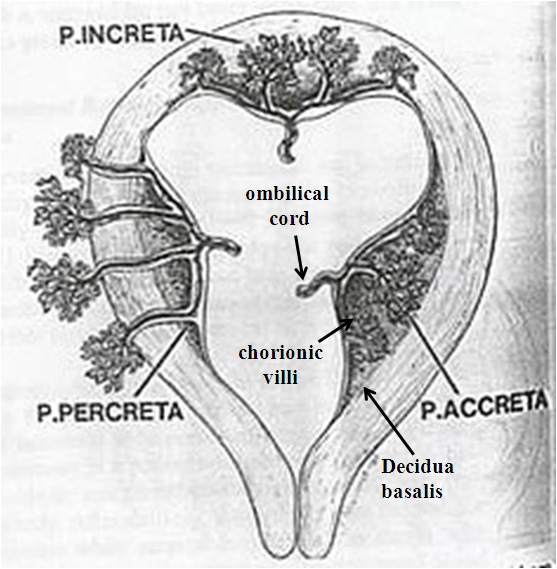
Abnormal placentation
Abnormal placentation is a condition whereby the placenta attatches too deeply into the uterine wall. 2/3 of the cases require Cesarean hysterectomy. And for these cases blood should be on hand since average blood loss is 3-5 L.
| Abnormal placentation | Frequency | Description |
|---|---|---|
| Placenta accreta | 75-78% | Placenta villi invade beyond Nitabuch’s layer and into the deep layers of the decidua basalis |
| Placenta increta | 17% | Placenta vili partially invade into the myometrium |
| Placenta percreta | 5-7% | Placenta vili invade completely through the myometrium and occasionally to the serosa and beyond (bladder) |