Antepartum Fetal Surveillance
Antepartum fetal surveillance is done after 24 weeks for high-risk pregnancies or mothers concerned about reduced fetal movements. It should not modify an otherwise normal pregnancy and should not provide a false sense of well-being or impending danger.
- Antepartum fetal surveillance
- Fetal movements (kick charts)
- Non-stress test
- Biophysical profile score
- Doppler U/S of umbilical artery
- Doppler U/S of fetal vessels (MCA vasodilation, AA vasoconstriction)
- Amniotic fluid index measurement
- Fetal lung maturity
Fetal Movements (”Kick” charts)
Maternal perception of fetal movements can be used to monitor fetal well-being. A decrease in movements can precede fetal death. A kick is defined as full movement of extension of flexion (sensation of “playing” around). There is a wide range of normal but < 10 kicks in 12 hours should be evaluated further.
- Keeping a fetal kick chart
- Get a plain paper and pen
- First kick: note the time and tick on the paper
- Subsequent kicks: tick on the paper
- 10th kick: note the time and tick on the paper
- Note how many hours it took to get to the 10th kick.
Electronic Fetal Monitoring (Non-stress test, NST)
Electronic fetal monitoring is used to assess fetal well-being during labour. The terms “REASSURING” vs “NON-REASSURING” are preferred to describe fetal status due to high false positive rates. A uterine tocometer and external fetal heart monitor are used for cardiotocometry (measuring heart rate and uterine pressure). The mother should be positioned comfortably in a left-lateral or semi-recumbent position and recordings should be made for at least 30 minutes. A CTG can be combined with ultrasound to form the Biophysical profile.
- Indications for NST
- Post-term
- High-risk pregnancy
- Decreased or loss of fetal movements
- IUGR
- Rh isoimmunization
- What do we want (REASSURING)
- 2 or more FHR Acceleration in a 30-minute CTG (15 beats above baseline, lasting 15 seconds, in 20 minutes)
- Normal baseline FHR (110 – 160 bpm)
- Moderate variability
- No decelerations or early decelerations
- What we fear (NON-REASSURING)
- Severe, persistent tachycardia or bradycardia (<110 bpm)
- Absent variability
- Severe variability
- Repetitive Severe variable decelerations, or Late decelerations
- Interventions for non-reassuring Fetal heart pattern
- Consider non-hypoxic causes (Anaesthesia/ medications)
- Intrauterine resuscitation procedures
- Discontinue oxytocin
- High-low oxygen facemask
- Change position from supine (to raise CO)
- Vaginal exam (one of the causes of bradycardia is cord prolapse)
- Scalp stimulation (to get fetal heart rate up)
- Reassess EFM/CTG strip
- Consider fetal scalp pH assessment
- Prepare for prompt delivery if normalization does not occur

Baseline fetal heart rate (FHR)
Normal FHR is between 110-160 bpm and contractions are ≤ 5 per 10 minutes (≥ 200 MVUs). The baseline is where the heart rate hovers around (excluding accelerations and decelerations. Round off to the nearest 5). An abnormality of the FHR is usually benign if there is good variability
| Fetal bradycardia (<110) | Fetal Tachycardia (> 160 bpm) | |
|---|---|---|
| Normal | Fetal sleep | Fetal movement/stimulation |
| Maternal factors | Supine position, Hypotension, Hypoglycemia | Stress/Anxiety, Fever/infection, Thyrotoxicosis, Anemia, Hypoxia |
| Maternal-fetal interface | Poor uterine perfusion, Umbilical cord prolapse | Chorioamnionitis, Abruptio placentae |
| Fetal factors | Arrhythmia (congenital heart block), Vagal stimulation | Arrhythmia, Anemia/acute blood loss |
| Medications | Opioids, Anesthesia, MgSO4, Beta-blockers | Anticholinergics, Sympathomimetics, Illicit drugs e.g, cocaine |
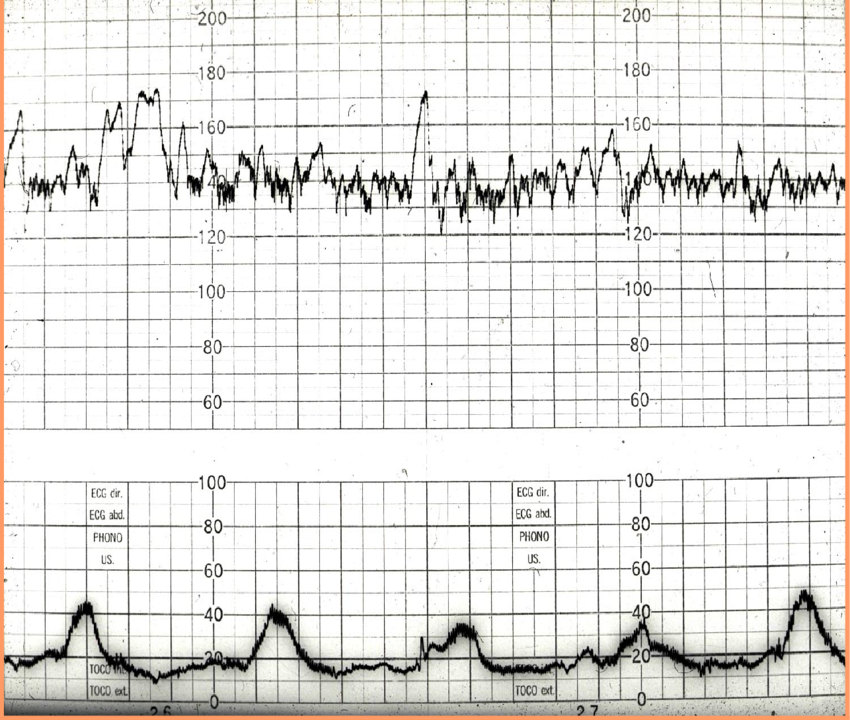
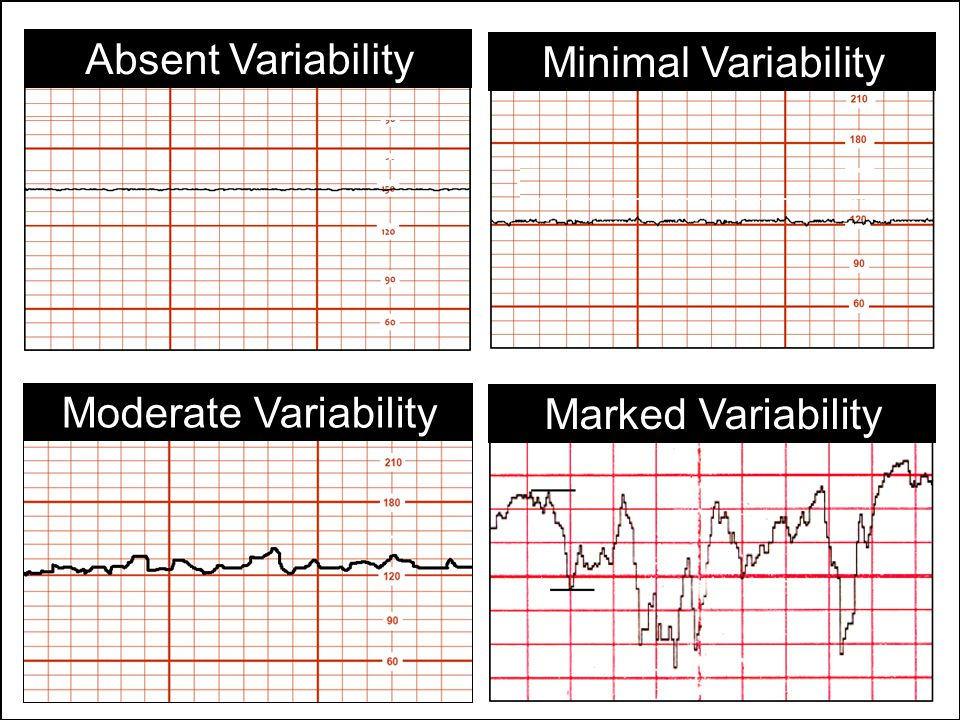
Variability
Variability is the fluctuation of the baseline in amplitude and frequency of ≥ 2 cycles/min. Variability comes about due to the interplay of the parasympathetic and sympathetic nervous system. It is modified by gestational age, fetal sleep status, activity, hypoxia and drugs (all of which reduce baseline variability)
Absent variability: undetectable variability. NON-REASSURING.
Low variability: difference of ≤ 5 bpm
Moderate variability: difference of 6 – 25 bpm. REASSURING.
Marked variability: difference of > 25 bpm. (Associated with fetal hypoxia)
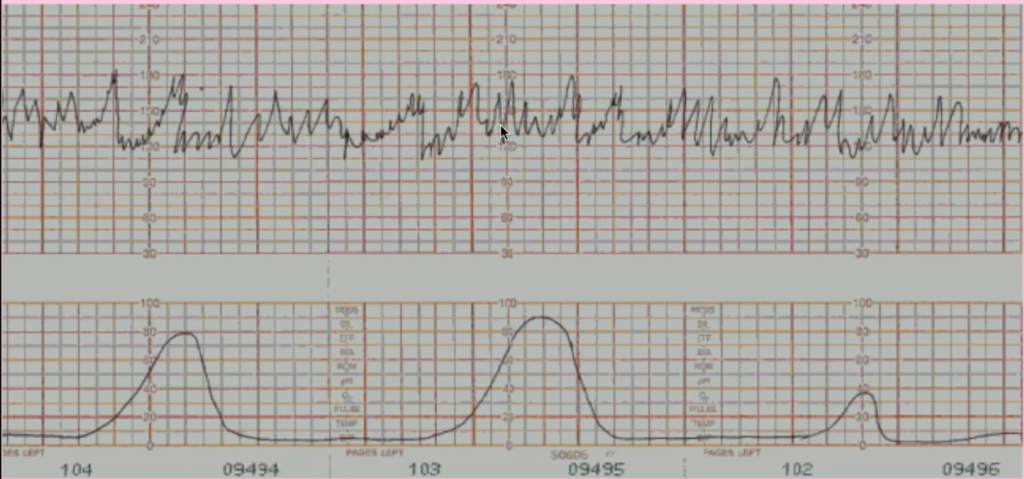
Accelerations
Accelerations are periodic increases in FHR of 15 bpm, sustained for at least 15 seconds (15 x 15). We like to see accelerations (A reactive trace = 2 or more accelerations on a 20-30 minute CTG). They are always REASSURING. Accelerations may coincide with contractions (periodic) or be independent of contractions (aperiodic).
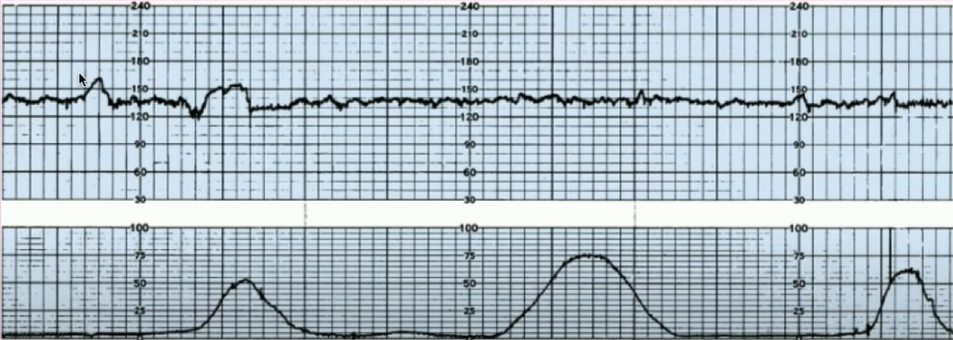
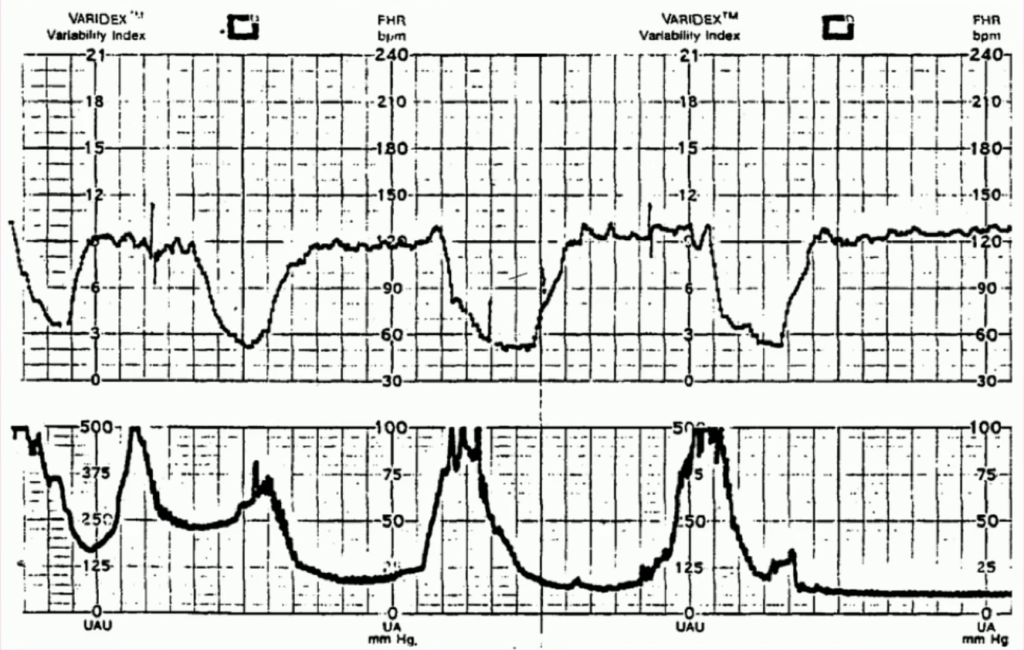
Decelerations
A deceleration is a drop in FHR of >15 bpm with onset to nadir of > 30 secs duration (applies to early and late decels).
Early decelerations: Decelerations coinciding with contractions. Associated with vagal stimulation due to fetal head compression. Smooth and gradual. INCONSEQUENTIAL.
Variable decelerations: Decelerations variable about contractions. Associated with cord compression (mild or moderate decels) or acidosis (severe decels). Abrupt changes and reach a nadir in < 30 seconds. May last longer or not. More jagged and irregular. NON-REASSURING WHEN SEVERE.
| Types of variable deceleration | Drop | Association |
|---|---|---|
| Mild variable decelerations | 15 – 40 bpm | Cord compression |
| Moderate variable deceleration | 40 – 60 bpm | Cord compression |
| Severe variable deceleration | > 60 bpm or below 70 bpm | Fetal acidosis |
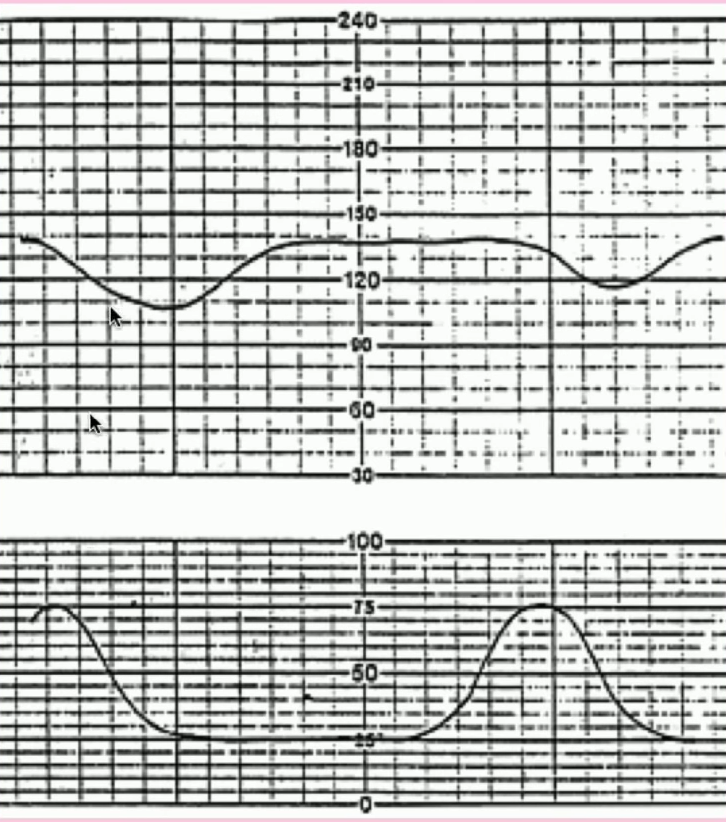
Late decelerations: Decelerations after contractions. More gradual and shallow than variable decels. Associated with uteroplacental insufficiency when the uterus is contracting. ALWAYS NON-REASSURING.
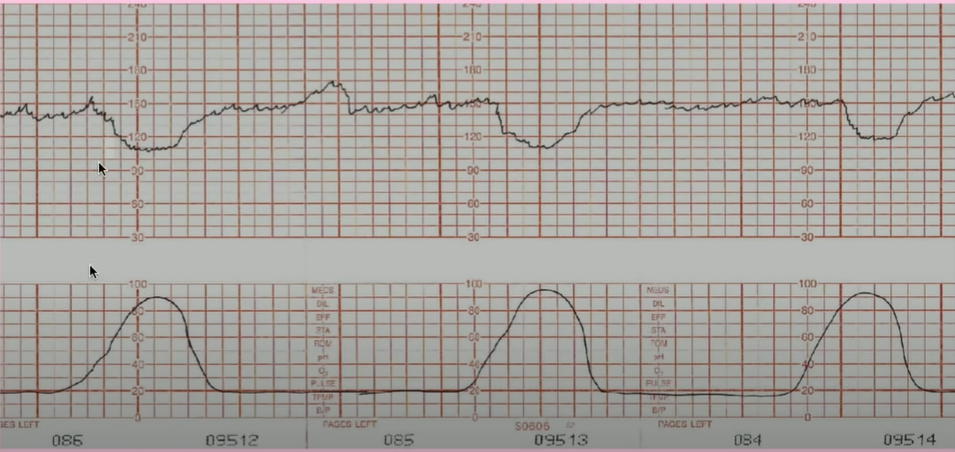
Early deceleration
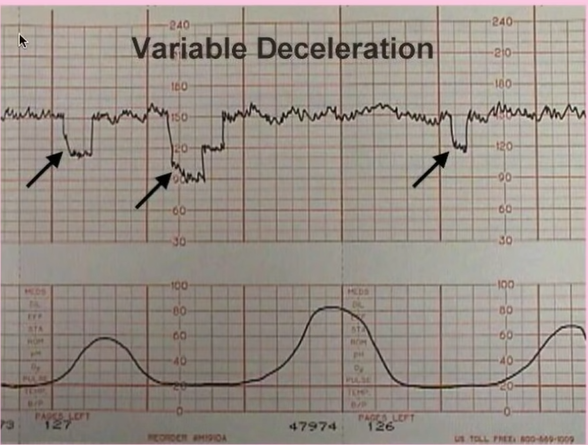
Variable decelerations
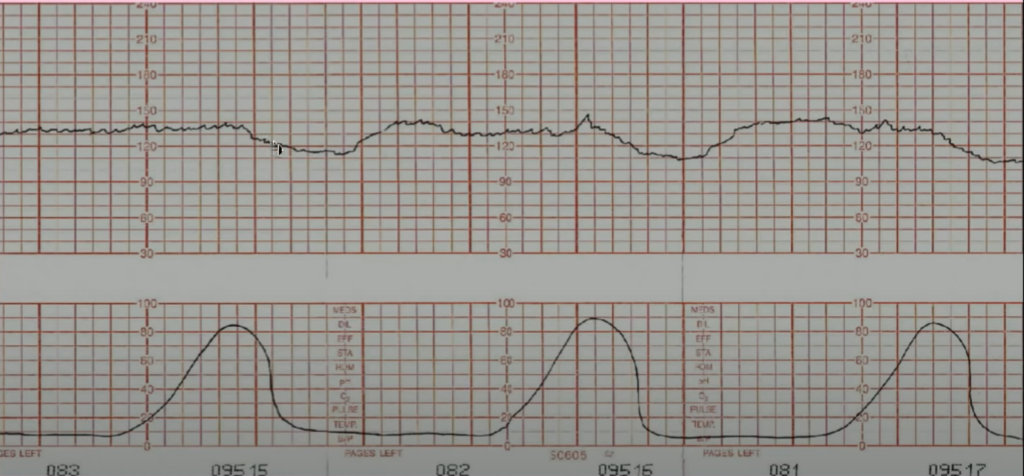
Late decelerations
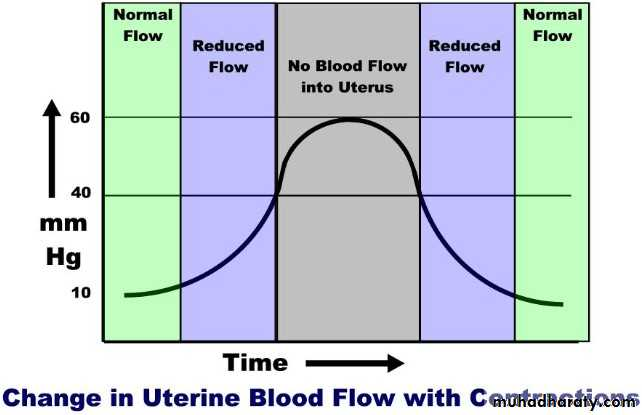
Change in uterine blood flow with contractions
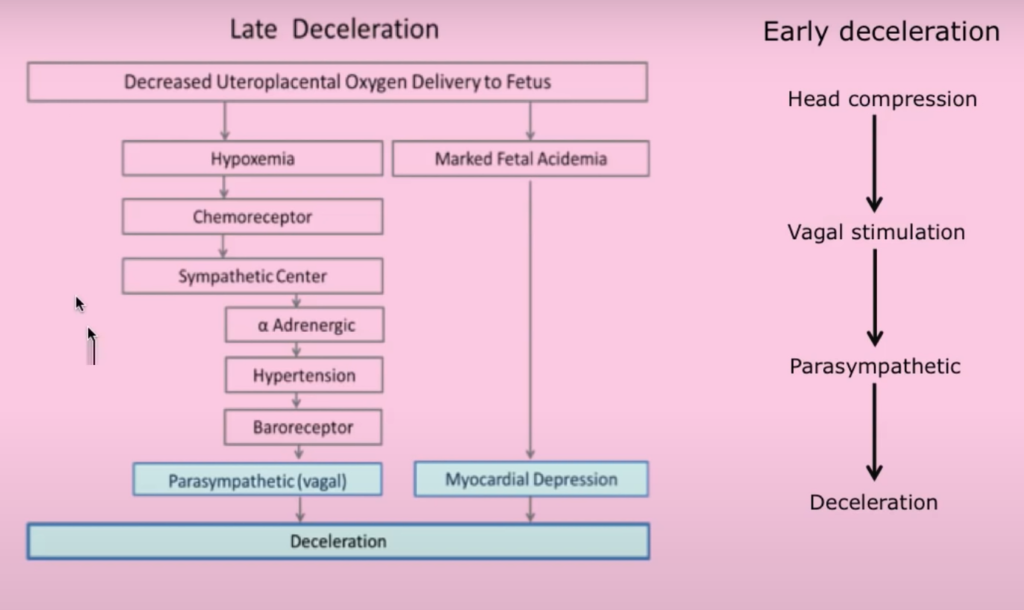
Pathophysiology of late deceleration vs early deceleration. Late deceleration has a lag time to become hypoxic.
Marked variability (difference of 70bpm)
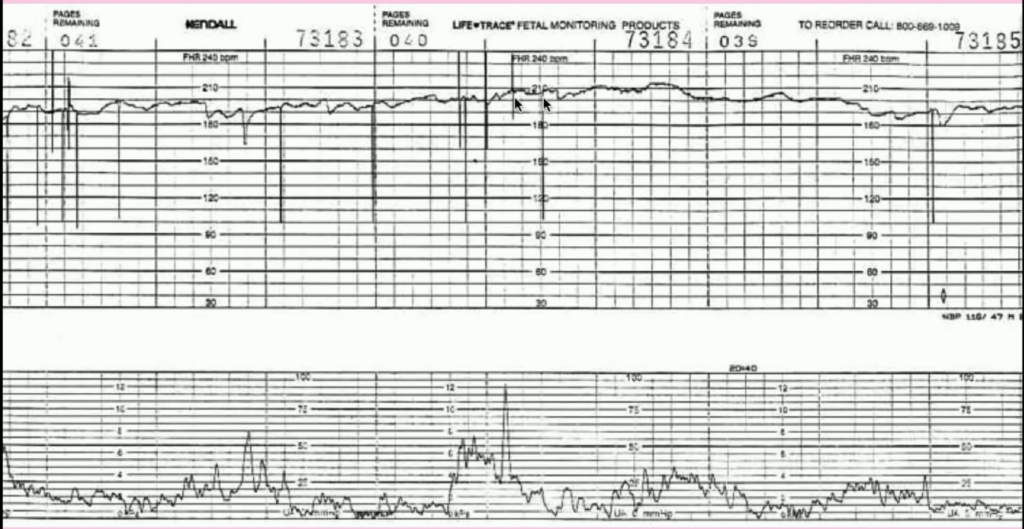
Tachycardia (baseline FHR of 190)
Absent variability and late decelerations
Biophysical Profile Score
The biophysical profile score is real-time ultrasonography that combines at least four variables to assess fetal well-being
- VariablesBATMaN
- Breathing movements in 30 minutes
- Amniotic fluid volume
- Tone
- Movements in 30 minutes (Gross body or limb movements)
- Non-stress test (not done routinely)
Scoring
| Variable | 2 | 1 | 0 |
|---|---|---|---|
| Fetal Breathing Movements | One episode lasting at least 60 seconds within 30 minutes | One episode lasting 30-60 seconds within 30 minutes | No breathing movement or breathing movements less than 30 seconds within 30 minutes |
| Fetal Reactivity | Definity reactivity (over 2 accelerations in 30 min) | Equivocal reactivity (1 or 2 accelerations in 30 minutes0 | No reactivity (no accelerations in 30 minutes) |
| Amniotic Fluid Vlume | 2cm square or more | Between 1cm and 2 cm | Less than 1 cm |
| Fetal Tone | At least one episode involving both extremities and spine | At least one episode involving either extremitites or spine | Extension movement of extremities not followed by return to flexion |
| Fetal Movement | 3 or more in 30 min | 1 or 2 in 30 min | No movement in 30 min |
Interpretation of scores
| Score | Interpretation |
|---|---|
| 10 – 8 with normal AFI | Normal |
| 6 | Potential problem. Further evaluation necessary |
| < 4 | Abnormal. Consider delivery if > 32 weeks. Further monitoring and evaluation if < 32 weeks. Increased risk of Stillbirth or asphyxia |
| 0 | Intrauterine fetal death (IUFD) |
Doppler of Umbilical Artery
Waveforms in the umbilical arteries provide information on the fetoplacental blood flow. The resistive index (RI) is the maximum umbilical artery systolic velocity – minimum umbilical end-diastolic velocity. >95th centile on a normal graph indicates hypoperfusion and possible fetal hypoxia
- Indications for umbilical artery doppler
- Hypertension
- Diabetes
- Renal Disease
Doppler of the Middle Cerebral Artery and Abdominal Aorta
- Chronic hypoxia results in the redistribution of blood flow to protect the vital organs (brain, adrenals, heart, spleen) by vasoconstricting other vessels.
- The Middle Cerebral Artery vasodilates in hypoxia while the abdominal aorta vasoconstricts in hypoxia
Fetal Scalp blood sampling
Scalp blood sampling for pH and Lactate can be performed in cases of non-reassuring FHR patterns.
